Our treatment results of distal radius torus fractures with static wrist splint
Wrist splint for torus fractures
Authors
Abstract
Aim There is a wide spectrum in the treatment of distal radius torus fractures (DRTF), from soft bandaging to plaster immobilization. In this study, we aimed
to show the results of static wrist splints in the treatment of torus fractures.
Methods 34 children with DRTF were included in the study and analyzed retrospectively. These patients were given full-time static wrist splint for three weeks. Visual pain score (VAS) and function scores were examined.
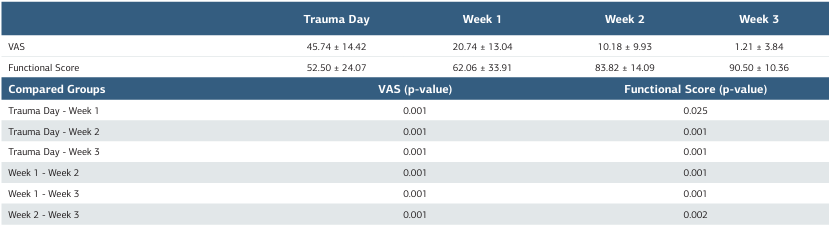
Results The average VAS scores of the patients were on the first day of trauma (45.74 ± 14.42); At the end of the 1st week (20.74 ± 13.04); It was (10.18 ± 9.93) at the end of the 2nd week and (1.21 ± 3.84) at the end of the 3rd week. The average function score of the patients was on the first day of the trauma (52.50 ± 24.07), at the end of the first week (62.06 ± 33.91); It was (83.82 ± 14.09) at the end of the 2nd week and (90.50 ± 10.36) at the end of the 3rd week. When the weekly scores of the groups were compared with each other, it was seen that there was a significant improvement every week (p <0.05).
Conclusion It can be easily removed by parents at home by giving full verbal and written instructions and recommendations at the first outpatient clinic visit after torus fractures, and it provides much more comfortable immobilization for the patient compared to a plaster splint. However, prospective randomized studies are needed on the adequacy of wrist splint.
Keywords
Introduction
The term “torus” is derived from the Latin word “tori” and refers to the integrity of the periosteum in the metaphyseal-diaphyseal junction, implying undisturbed or minimally disturbed fractures with intact cortex 1. It is believed that compression forces at the transitional zone between trabecular metaphyseal bone and lamellar dense diaphyseal bone in its pathophysiology2. Distal radius torus fractures (DRTF) are common fractures in childhood and constitute a significant portion of the orthopedic workload in emergency departments 1,3,4. They typically occur after a fall while the wrist is in extension position, and patients present with a history of tenderness and swelling. Torus fractures and greenstick fractures are specific to the pediatric patient population5,6. As seen in Figure 2, torus fractures are more stable compared to greenstick fractures 7. Torus fractures can usually be successfully treated with conservative methods; however, minimally displaced fractures are of concern due to their potential instability8. There are significant differences in the treatment of DRTF among different hospitals and orthopedic surgeons. The standard treatment involves immobilization in a short-arm cast for three weeks followed by outpatient examination and control radiography for cast removal 2,9. Alternative treatments such as orthoses, elastic bandaging, and circular plaster immobilization have been described. Recent studies have shown that circular plaster immobilization may be unnecessary and that short-term wrist support may be sufficient 2. Our hypothesis is that treatment with a static wrist splint may be sufficient for torus fractures and that using a wrist splint that can be removed and re-applied after necessary precautions, instead of methods like circular plaster that may disrupt patient comfort, may be advantageous. Therefore, in our study, we attempted to determine the treatment outcomes, both in terms of pain and function, of patients with DRTF treated with a static wrist splint.
Materials and Methods
Patients diagnosed with distal radius torus fractures and undergoing weekly follow-ups between June 1, 2020, and December 31, 2021, at Konya City Hospital and Niğde Ömer Halisdemir University Hospital Orthopedics Clinics were included in the study. Comprehensive verbal and written explanations were provided to the parents of pediatric patients who would undergo wrist splinting. Patients who experienced multiple traumas, had a second fracture, had systemic comorbidities, or did not comply with outpatient appointments were excluded from the study. All patients received a standard treatment protocol consisting of cold therapy and elevation for traumatic extremities for the first 48 hours, followed by full-time static wrist splinting for three weeks(Figure 1). Patients and their families were instructed that they could remove the splint for bathing and hand hygiene. Weekly follow-ups were conducted throughout the treatment duration. Pain severity was assessed using a visual analog scale (VAS), and functional scores were determined using standardized questionnaires. The VAS score was determined by asking the question, “On a scale of 0 to 10, with 0 being no pain and 10 being the worst pain imaginable, what is your current level of pain?” Subjective functional scores were determined by asking, “On a scale of 0 to 100, with 0 being no movement in the uninjured wrist and 100 being full movement, what is your current wrist movement?” Both scores were recorded after outpatient visits.
Statistical analysis of the data was performed using IBM SPSS 22.0 for Windows (SPSS Inc, Chicago, IL, USA). Descriptive statistics for demographic data and variables were presented as mean ± standard deviation. The normality of independent variables was assessed using the Shapiro-Wilk test. Due to non-normal distribution of the data, the Wilcoxon test was used. All analyses were performed with 80% power and >95% confidence level. p-values <0.05 were considered statistically significant.
Ethical Approval
The research was approved by the Erciyes University Clinical Research Ethics Committee (Date: 2018-07-04, No: 2018/348).
Results
During the 19-month study period, wrist splints were applied to 35 torus fractures that met the appropriate criteria. However, one patient developed refracture and was excluded from the study due to a diagnosis of attention deficit, leaving 34 patients whose data were analyzed. Of these patients, 26 were male (76.5%) and 8 were female (23.5%). The mean age was 9.15 ± 2.53 years in males (range: 5–14), 9.50 ± 2.67 years in females (range: 5–12), and 9.24 ± 2.52 years overall (range: 5–14). All 34 patients showed excellent healing of distal radius torus fractures. VAS and functional scores showed statistically significant improvement each week (p < 0.05). The VAS score improved the most during the first week, while the functional score improved the most during the second week (Figure 3). The VAS scores were 45.74 ± 14.42 at week 0, 20.74 ± 13.04 at week 1, 10.18 ± 9.93 at week 2, and 1.21 ± 3.84 at week 3. The functional score was 52.50 ± 24.07 at week 0, 62.06 ± 33.91 at week 1, 83.82 ± 14.09 at week 2, and 90.50 ± 10.36 at week 3. All patient data are provided in Table 1. There were no cases of reduction loss or other complications in any of the 34 patients. Significant differences were observed between VAS values on the day of trauma and at weeks 1, 2, and 3 (p = 0.001 for each). Significant differences were also observed between VAS values in the first week and at weeks 2 and 3 (p = 0.001 for each). Additionally, significant differences were found between VAS values at week 2 and week 3 (p = 0.001). Similarly, significant differences were observed between functional scores on the day of trauma and at weeks 1, 2, and 3 (p = 0.025, p = 0.001, p = 0.001, respectively). Significant differences were also found between functional scores in the first week and at weeks 2 and 3 (p = 0.001 for each), as well as between functional scores at week 2 and week 3 (p = 0.002). All statistical values are provided in Table 1.
Discussion
In our study, we evaluated the outcomes of using static wrist splints instead of commonly used plaster casts in the orthopedic practice for torus fractures, which are encountered very frequently. The use of wrist splints appears to be a cost- effective and less complicated method with greater comfort for patients in the treatment of torus fractures.
Simple falls perceived as minor injuries by parents can be diagnosed as delayed torus fractures in the emergency department. Torus fractures are fractures where the bone cortex swells due to compression forces along the longitudinal axis of the bone. Recent research emphasizes that this fracture is a stable injury and can be treated with supportive care and pain control alone 1,2,4,9. There are various treatment options available, including long or short arm casts, wrist splints, and soft bandages. Plint et al. have shown that patients treated with wrist splints have better physical function and experience less difficulty in certain activities compared to those treated with casts, with no difference in pain levels10. In our study, parents’ satisfaction with the wrist splint was also very high. Pediatric patients and their parents who were able to express themselves reported being pleased with the ability to remove the wrist splint for bathing. The fact that parents could remove the splint themselves also reduces the workload of plaster technicians in orthopedic clinics. Additionally, parents noted that accompanying their children to the clinic was reduced, saving them time.
After torus fractures, during the initial clinic visit, providing comprehensive verbal and written instructions and recommendations enables parents to easily remove the splint at home, which provides much more comfortable immobilization for the patient compared to a plaster cast. Farman showed that medical studies conducted after plaster application for torus fractures are unnecessary and that multiple radiographs do not alter fracture management 11. In our study, all fractures healed smoothly both clinically and radiologically during follow- up visits. No complications requiring radiological follow-up were observed. It is important to economically evaluate health- related technologies and treatment strategies 12.
The 35 wrist splints we applied provide important data for evaluating the effects of wrist torus fracture treatment. However, one of the patients we treated later received a diagnosis of attention deficit and unfortunately developed a refracture, suggesting that if the patient cannot show the necessary attention and care during this treatment process, the risk of fracture recurrence may increase. Therefore, patient education and continuous monitoring are important in wrist splint treatment for torus fractures, and various supportive strategies should be considered to improve patient compliance. In cases where compliance is poor and the risk of complications is high, plaster treatment may be preferred.
We believe that discharging patients with wrist splints can provide significant savings in terms of cost and workload. Wrist splint can be considered a low-cost, low-complication, easy, and acceptable treatment method for RAUTK treatment.
Limitations
Our study has some limitations. Firstly, it should be noted that the data collection process of a retrospective study is based on the past and may be exposed to uncontrolled variables. Additionally, the inclusion of a small number of patients may affect the diversity of results. Prospective studies with a larger patient population in the future will help to strengthen the foundation of the results.
Conclusion
We believe that discharging patients with wrist splints can provide significant savings in terms of cost and workload. Wrist splint can be considered a low-cost, low-complication, easy, and acceptable treatment method for RAUTK treatment.
Figures

Figure 1. Application of wrist splint (Necessary permissions were obtained from parents for the use of images)
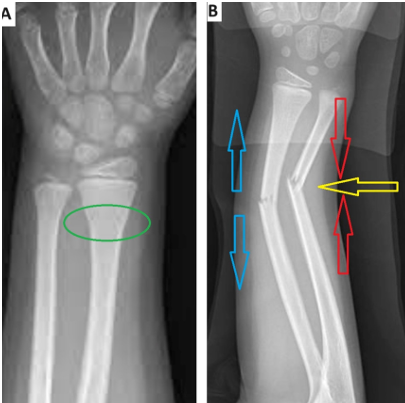
Figure 2. A illustrates a torus fracture (buckle fracture), showing the swelling and plastic deformation at the metaphyseal- diaphyseal junction indicated by the green circle. FB depicts a greenstick fracture, where the deforming force, compressive forces indicated by the red arrow, and tensile forces represented by the blue arrow are shown. In greenstick fractures, there is plastic deformation on one side while the opposite cortex has a fracture
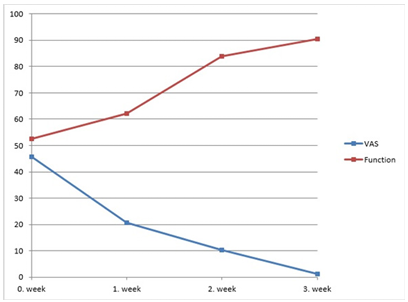
Figure 3. VAS and functional score
Tables
Table 1. Pain and function scores of patients
References
-
Davidson J, Brown D, Barnes S, Bruce C. Simple treatment for torus fractures of the distal radius. J Bone Joint Surg Br. 2001;83(8):1173-5.
-
Beaty JH, Kasser JR. Rockwood and Wilkins’ Fractures in Children. 8th ed. Philadelphia, PA: Wolters Kluwer; 2015.p.571-575.
-
Jiang N, Cao Z-h, Ma Y-f, Lin Z, Yu B. Management of pediatric forearm torus fractures: A systematic review and meta-analysis. Pediatric emergency care. 2016;32(11):773-8.
-
Solan M, Rees R, Daly K. Current management of torus fractures of the distal radius. Injury. 2002;33(6):503-5.
-
Randsborg PH, Sivertsen EA. Distal radius fractures in children: Substantial difference in stability between buckle and greenstick fractures. Acta orthopaedica. 2009;80(5):585-9.
-
Schmuck T, Altermatt S, Büchler P, et al. Greenstick fractures of the middle third of the forearm. A prospective multi-centre study. Eur J Pediatr Surg. 2010;20(5):316-20.
-
Pountos I, Clegg J, Siddiqui A. Diagnosis and treatment of greenstick and torus fractures of the distal radius in children: A prospective randomised single blind study. J Child Orthop. 2010;4(4):321-6.
-
West S, Andrews J, Bebbington A, Ennis O, Alderman P. Buckle fractures of the distal radius are safely treated in a soft bandage: A randomized prospective trial of bandage versus plaster cast. J Pediatr Orthop. 2005;25(3):322-5.
-
Vernooij CM, Vreeburg ME, Segers MJ, Hammacher ER. Treatment of torus fractures in the forearm in children using bandage therapy. J Trauma Acute Care Surg. 2012;72(4):1093-97.
-
Plint AC, Perry JJ, Correll R, Gaboury I, Lawton L. A randomized, controlled trial of removable splinting versus casting for wrist buckle fractures in children. Pediatrics. 2006;117(3):691-7.
-
Farbman KS, Vinci RJ, Cranley WR, Creevy WR, Bauchner H. The role of serial radiographs in the management of pediatric torus fractures. Arch Pediatr Adolesc Med. 1999;153(9):923-5.
-
Bozic KJ, Rosenberg AG, Huckman RS, Herndon JH. Economic evaluationin orthopaedics. JBJS. 2003;85(1):129-42.
Declarations
Scientific Responsibility Statement
The authors declare that they are responsible for the article’s scientific content, including study design, data collection, analysis and interpretation, writing, and some of the main line, or all of the preparation and scientific review of the contents, and approval of the final version of the article.
Animal and Human Rights Statement
All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Funding
None
Conflict of Interest
The authors declare that there is no conflict of interest.
Ethics Declarations
This study was approved by the Ethics Committee of Erciyes University Clinical Research (Date: 2018-07-04, No: 2018/348)
Data Availability
The data supporting the findings of this article are available from the corresponding author upon reasonable request, due to privacy and ethical restrictions. The corresponding author has committed to share the de-identified data with qualified researchers after confirmation of the necessary ethical or institutional approvals. Requests for data access should be directed to bmp.eqco@gmail.com
Additional Information
Publisher’s Note
Bayrakol MP remains neutral with regard to jurisdictional and institutional claims.
Rights and Permissions
About This Article
How to Cite This Article
Ahmet Yurteri, Ahmet Sinan Sarı, Muhammet Zeki Gültekin, Fatih Doğar, Özgün Karakuş, Ahmet Yıldırım. Our treatment results of distal radius torus fractures with static wrist splint. Ann Clin Anal Med 2025; DOI: 10.4328/ACAM.22253
Publication History
- Received:
- May 6, 2024
- Accepted:
- July 2, 2024
- Published Online:
- April 3, 2025
- Printed:
- November 1, 2025

