Hospitalized with a lower respiratory tract infection, evaluation of children aged 2-5 in terms of breast milk intake
Evaluation of children aged 2-5 in terms of breast milk intake
Authors
Abstract
Aim It was aimed to evaluate the breast milk intake of children aged 2-5 years who were hospitalized with lower respiratory tract infection and to investigate the effect of breast milk on lower respiratory tract infection.
Materials and Methods Between 01.01.2016 and 31.12.2021, Muğla Training and Research Hospital Pediatrics polyclinics; The aim of this study was to retrospectively scan the files of 908 patients aged 2-5 years, who were admitted to the hospital with the diagnosis of pneumonia and bronchiolitis, and who were not admitted to the outpatient clinic for general control or follow-up, and were selected randomly, to compare their breastfeeding status.
Results There is a statistically significant difference in whether the cases are hospitalized or not depending on the duration of breastfeeding. As the duration of breastfeeding increased from 6 months to 24 months, hospitalization rates decreased. There is a statistically significant difference in the hospitalization duration of the cases hospitalized according to the duration of breastfeeding. As the duration of breastfeeding increased from 6 months to 24 months, the average hospital stay decreased.
Discussion In addition to the many benefits and requirements of breast milk, it has been observed that it is protective against lower respiratory tract infections that require hospitalization. However, according to the information obtained in our study, the total duration of breastfeeding and the rate of exclusive breastfeeding for the first 6 months are below the targeted levels.
Keywords
Introduction
Breast milk is the most suitable food in terms of its content and the bond to be established with the mother. The World Health Organization [WHO ] also recommended only breast milk for infant feeding for the first 6 months and said that it would be beneficial to continue up to 2 years [1]. As the content of breast milk can vary depending on many factors, the way of giving breast milk can also differ in terms of the benefit it provides to the newborn. The content of breast milk is greatly affected by the nutritional habits of the mother before birth and continues in this form after birth [2, 3, 4]. In addition to its nutritional function, breast milk contains more than four hundred different proteins that are antimicrobial, responsible for regulating immune events, and responsible for the transport and absorption of different nutrients [5]. It is known to have a protective effect against infections in otitis media, gastroenteritis, necrotizing enterocolitis, lower respiratory tract, and urinary tract infections [5]. Although breastfeeding is common in our country, there is a concern that early or late initiation of complementary foods will pose a significant problem [6]. In our study, we aimed to investigate whether the children who did not have a lower respiratory tract infection that required hospitalization, who did not have a known chronic disease, who applied to the polyclinic for control or reasons that did not require hospitalization, and whether they did not receive breast milk and the duration of it and to give these two groups to supplementary food among themselves. We wanted to compare the onset times, and duration of breastfeeding and investigate the effects of these on diseases such as bronchiolitis and pneumonia.
Materials and Methods
Between 01.01.2016 and 31.12.2021, Muğla Training and Research Hospital Pediatrics polyclinics; is a retrospective and cross-sectional study to compare the breastfeeding status of randomly selected children aged 2-5 who were admitted to the hospital with the diagnoses of pneumonia and bronchiolitis, and children aged 2-5 who were not hospitalized but were admitted to the outpatient clinic for general control or follow-up. Our study focused on the status and duration of breastfeeding of children aged 2-5, who have lower respiratory tract infections that require hospitalization, and who have relatively limited contact with the community yet. Children between the ages of 2 and 5 who were admitted with the diagnosis of pneumonia and bronchiolitis and hospitalized were identified by the data processing unit of our hospital according to the diagnosis codes they received, and after their names and identification information were determined, patient epicrisis was scanned through the hospital information management system and the necessary information was obtained for the research. The list of children aged 2-5 years who have not been admitted to the outpatient clinic for general follow-up and/or reasons that do not require hospitalization was obtained from the IT unit of our hospital, and the randomly selected children between the specified dates were continued to be included in the study until they reached the same numbers as the inpatient group. The duration of breastfeeding throughout the study; was investigated by categorizing it as ‘Never breastfed’, ‘Breastfed for less than 6 months’, ‘From 6 months to 24 months’, and ‘For at least 24 months’. Since the initiation of complementary food is recommended after 6 months, the cases after which month they started solid food were categorized as ‘before 6 months’ and ‘after 6 months’.
Relatively milder cases who were hospitalized or responded to treatment within 48-72 hours because a clear decision could not be made between outpatient treatment/inpatient treatment; They were grouped as those who were hospitalized for 3 days or less. Cases in which the treatment is completed between 3-7 days, antibiotic protocols or supportive treatments are completed in the hospital, and the duration of hospitalization can be called moderate; They were grouped as patients who were hospitalized for 3-7 days. Severe cases with no response to treatment or delayed response, treatment change or treatment addition, and long-term hospitalization; They were grouped as those who were hospitalized for more than 7 days. The duration of breast milk intake was compared with whether or not he was hospitalized, whether he received oxygen therapy, whether he received steroid therapy, whether he received antibiotic therapy, and whether he received bronchodilator therapy. The data obtained from the research were evaluated in a computer environment and using a statistical package program [SPSS 26]. In descriptive statistical analyses, percentages, mean, and standard deviation; the Chi-square test was used for comparisons between groups. p<0.05 values were considered statistically significant.
Ethical Approval
Ethics Committee approval for the study was obtained. While conducting the study, international instructions, including the “Regulations on Pharmaceutical Research” and subsequent applicable instructions, were complied with. Ethics committee approval was received from the ethics committee of Muğla Sıtkı Koçman University (Date: 2022-01-14, No: E-72855364- 050.01.04-375108).
Results
11(1.2%) of the cases were excluded according to the exclusion criteria, and the study was continued with 897 cases. 41.9% (n=376) of the cases were female and 58.1% (n=521) were male. 22.4% (n=201) of the children aged 2-5 years included in the study are 2 years old, 37.5% (n=336) are 3 years old, 27.3% (n=245) are 4 years old, 12.8% (n=115) were 5 years old. The mean age of the investigated cases was 3.30 ± 0.95. It was possible to reach the duration of breastfeeding. The average duration of breastfeeding was determined as 12.9 ± 9.2 months in 200 cases whose information could be accessed.
In cases in which the duration of breastfeeding is known; 9% (n=18) have never been breastfed, 33% (n=16.5) have been breastfed but have received less than 6 months, 51% (n=12) have been breastfed between 6 months and 24 months, 23.5% (n=47) were breastfed for at least 24 months. It is shown in Table 1.
The numerical average of 177 cases whose information could be reached, after which month they started complementary food, was found to be 4.9 ± 3.1. While 36.1% (n=64) of the 177 cases known to have started complementary food were found to have started solid food before 6 months, 63.8% (n=113) were found to have started solid food after 6 months. Of the 218 cases whose birth type information could be accessed; 39.9% (n=87) were found to have normal/vaginal deliveries, and 60% (n=131) were found to be delivered by cesarean section. Of the 219 cases whose time of birth could be accessed, 81.2% (n=178) were born at term, and 18.7% (n=41) were born preterm. Of 209 cases whose birth weight information could be accessed, 81.2% (n=178) had a birth weight between 2500 grams and 4500 grams, which is considered normal birth weight, and 18.6% (n=39) had a birth weight of low birth weight. They have birth weights below 2500 grams. It was determined that 0.9% (n=2) of 209 cases whose birth weight information could be accessed had very low birth weight and 0.9% (n=2) had extremely low birth weight. The hospitalization period of 92.8% (n=365) of the hospitalized cases could be reached. The average length of hospital stay was 3.7 ± 2.1.
The causative agent of lower respiratory tract infection could be detected in 4.8% (n=19) of the hospitalized cases, and the causative agent could not be detected in the remaining 95.1%
(374). The detected agents are Boca virus and Metapneumo virus, COVID, COVID-19 Delta, Human Metapneumovirus, Influenza, Rhino/Enterovirus, and RSV.
A statistically significant difference was found between the cases who were hospitalized and the cases who were not hospitalized, in terms of breast milk intake duration. The lowest hospitalization rate of the cases was observed in the group receiving breast milk from 6 months to 24 months. There is an increase in the number of hospitalizations in those who are breastfed for 24 months or more, but this increase does not reach the level of those who are breastfed for less than 6 months. It is shown in Table 2.
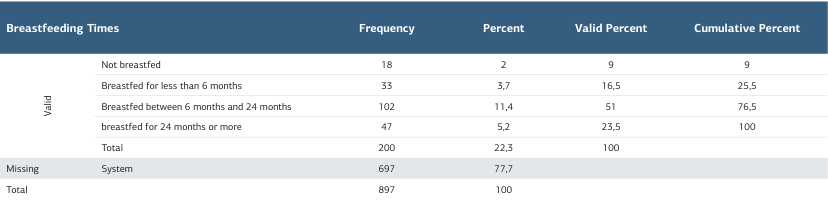
A statistically significant difference was found between the cases who were hospitalized for less than 7 days and those who were hospitalized for more than 7 days, in terms of breastfeeding duration. The lowest hospitalization rate of the cases for more than 7 days was observed in the group receiving breast milk from 6 months to 24 months, and the highest was observed in the group receiving breast milk for less than 6 months. It is shown in Table 3.
As a result of the research, it was determined that the cases received breast milk for an average of 12.9 ± 9.2 months. The average time to start supplementary food was found to be
4.9±3.1 months. 47.4% (n=94) of 198 cases, in whom both the duration of breastfeeding and the time to start complementary feeding could be reached, were fed exclusively with breast milk for the first 6 months.
Discussion
The fact that breastfeeding is still not at the desired levels, even in the literature, reminds us that very few children worldwide can fully benefit from the protective effects of breast milk. However, in the literature, it is stated that breastfeeding reduces fever, respiratory tract infections, infective gastroenteritis, and otitis media in babies aged 3-6 months; Data from 6 to 18 months, in which breast milk intake in any 3 months is negatively associated with the probability of conjunctivitis, laryngitis, tracheitis, ear infection, and infective gastroenteritis indicate a protective effect from infections, which like our study [7, 8, 9, 10]. We think that it supports the protective effects of taking it even in a certain period. In addition, considering that breastfeeding between 6-24 months reduces hospitalization and shortens hospital stays, we can think that it is reasonable that breast milk may have a protective effect against infection.
In a meta-analysis, of 16 studies examined, it was found that breastfeeding increased the incidence, prevalence, and hospitalization of respiratory tract infections in babies younger than 6 months. It is reported that it reduces the amount of hospitalization and has a protective effect against deaths [8]. It is observed that half of the diarrhea and one-third of respiratory tract infections in all babies can be prevented even with optimal breastfeeding [9, 10]. Our study suggests that breast milk may have a protective effect.
Dixon’s study comparing breastfed babies with formula-fed babies in terms of immunological advantage showed that breastfed babies had less respiratory distress, less need for oxygen support therapy, and fewer hospitalizations for bronchiolitis, which other studies have shown this situation has led to the interpretation that breast milk protects against RSV, the most common cause of bronchiolitis [11]. In our study, the rate and duration of hospitalization decreased in the period of breast milk intake from 6 months to 24 months, as well as the introduction of complementary foods from the 6th month. The low hospitalization rates of children with early onset suggest the protective effect of breast milk against infection, even if complementary feeding is started early, even if breast milk is consumed for an average of 4.9 ± 3.1 months.
In a study by Tromp et al., in which they investigated the relationship between the duration of breastfeeding and lower and upper respiratory tract infections in children aged 1-4 years, it was shown that breastfeeding for 6 months or more reduces lower respiratory tract infections [12]. In the same study, breastfeeding for 3-6 months reduces the risk of lower respiratory tract infections. It has been shown that children who have been breastfed for less than 3 months have lower respiratory tract infections less frequently than children who have been breastfed for less than 3 months [12].
Bachrach et al.’s meta-analysis study, based on 33 studies, investigating the effect of breastfeeding on respiratory tract infections in infants, found that infants who were not breastfed were three times more likely to be hospitalized due to respiratory tract infections than babies who were breastfed for at least 4 months. has shown the protection of breast milk [13]. We see that Bachrach’s study is compatible with our study, as it is protective against infections and the close duration of breastfeeding.
In another study conducted by Tarrant et al., in the study of hospitalizations due to childhood infections and breast milk, children who were breastfed for 3 months were less likely to be hospitalized due to infective diseases in the first 6 months of life than children who were not breastfed at all [14]. We can say that this study by Tarrant et al. differs from our data in terms of evaluating the long-term effects of breast milk.
In a prospective study by Ardıç et al., which investigated the long-term effects of breast milk in children under 5 years of age between 2011 and 2018; The fact that breastfeeding for more than 12 months is protective in terms of acute otitis media and acute gastroenteritis compared to breastfeeding for less than 12 months, but does not make a significant difference in terms of acute respiratory tract infections and acute urinary tract infections, supports our thesis and other studies indicating the protection of breast milk [15]. It is beneficial, but it also points to the need for larger prospective studies.
In this context, the study by Li et al. in 2014, investigating the relationship between breastfeeding duration and common infections in 6-year-old children, found that there was no significant difference between breastfeeding duration and upper respiratory tract infections, lung infections and urinary system infections, but ear infections, throat infections and sinusitis in the long term suggests the necessity of obtaining more specific infectious agents, and the need to obtain more detailed data on the amount of breast milk that children receive and the times when it is given, that is, breast milk [16].
Limitations
The most important limitation of our study is that the data were collected from the parents when the children came to the hospital and were obtained by reviewing old hospital records. In the study where 897 children were examined, the duration of breastfeeding of 200 children could only be reached due to reasons such as parents not providing accurate information or patient records being incomplete. Accordingly, the representativeness of the universe of the study was reduced.
Conclusion
In addition to the many benefits and requirements of breast milk, it has been observed that it is protective against lower respiratory tract infections that require hospitalization. However, according to the information obtained in our study, the total duration of breastfeeding and the rate of exclusive breastfeeding for the first 6 months are below the targeted levels. Necessary information and incentive policies should be implemented in this regard.
Tables
Table 1. Breast milk intake times
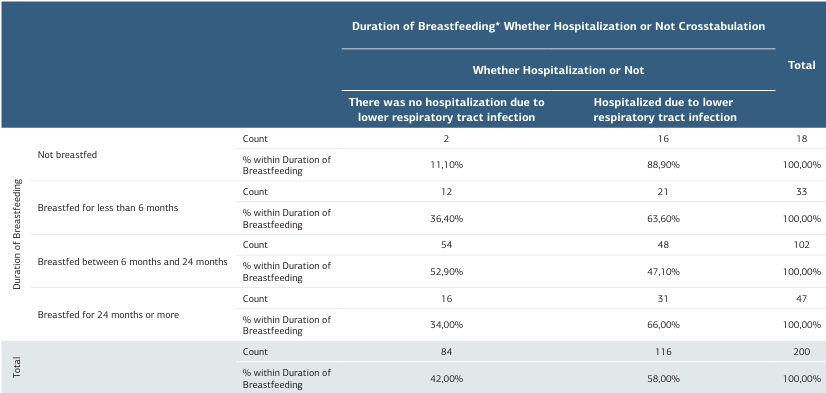
Table 2. Comparison of duration of breastfeeding and hospitalization (likelihood ratio test value p: 0,002 )
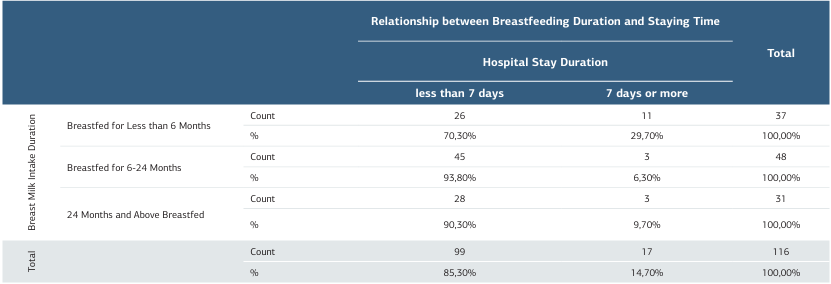
Table 3. Comparison of breastfeeding duration and hospitalization duration (likelihood-ratio value p: 0,009 )
References
-
Erick M. Breast milk is conditionally perfect. Med Hypotheses. 2018;111:82-9.
-
Bilgen H, Kültürsay N, Türkyılmaz C, editors. Sağlıklı term bebeğin beslenmesi rehberi [A guide to feeding a healthy term baby]. Ankara: Turkish Neonatology Association Publications; 2018.p:7-9.
-
Samur G, editors. Anne sütü[Breast milk]. Ankara: Klasmat Printing; 2008.p:11-8.
-
Öztürk Ö, Sarıkaya P, Özdemir Ş, Çikendin Z, Zünbül N. Anne sütü ve emzirme ile ilgili anneler tarafından bilinen doğrular ve yanlışlar [True and falses known by the mothers about mother milk and breastfeeding]. JCP. 2018;16(2):40-54.
-
Andreas NJ, Kampmann B, Mehring K, Le Doare A. Human breast milk: A review on its composition and bioactivity. Early Hum Dev. 2015;91(11):629-35.
-
Battaloğlu İnanç B. 15-49 yaş arası annelerin anne sütü ile ilgili uygulamaları ve etki eden faktörler [Breastfeeding practices and influencing factors of mothers aged 15-49]. Türk Aile Hek Derg. 2013;17(2):51-5.
-
Frank NM, Lynch KF, Uusitalo U, Yang J, Lönnrot M, Virtanen SM, et al. The relationship between breastfeeding and reported respiratory and gastrointestinal infection rates in young children. BMC Pediatrics. 2019;19(1):1-12.
-
Victora CG, Bahl R, Barros AJ, França GV, Horton S, Krasevec J, et al. Breastfeeding in the 21st century: Epidemiology, mechanisms, and lifelong effect. The Lancet. 2016;387(10017): 475-90.
-
Muslu M, Muslu Ş. Çocuk ve kadın hakları çerçevesinde; anne sütü ve emzirme [Within the framework of children’s and women’s rights; breast milk and breastfeeding]. Selçuk Sağlık Derg. 2021;2(2):168-96.
-
WHO Team. WHO editors. Short term effects of breastfeeding: A systematic review of the benefits of breastfeeding on diarrhea and pneumonia mortality. Geneva: World Health Organization Press;2013.p:30-3.
-
Dixon DL. The role of human milk ımmunomodulators in protecting against viral bronchiolitis and development of chronic wheezing illness. Children (Basel). 2015;2(3):289-304.
-
Tromp I, Kiefte-de Long J, Raat H, et al. Breastfeeding and the risk of respiratory tract infections after infancy: The generation R study. PLoS ONE. 2017;12(2):1-9.
-
Virginia R, Bachrach G, Schwarz E, Bachrach LR. Breastfeeding and the risk of hospitalization for respiratory disease in ınfacny: A-meta analysis. Arch Pediatr Adolec Med. 2003;157(3):237-43.
-
Tarran M, Man-Ki K, Tai-Hing L, Gabriel M, Leun B, Schooling MC. Breast-feeding and childhood hospitalizations for infections. Epidemiology. 2010;21(6):847–54.
-
Ardıç C, Yavuz E. Effect of breastfeeding on common pediatric infections: A 5-year prospective cohort study. Arch Argent Pediatr. 2018;116(2):126-32.
-
Li R, Dee D, Chuan-Ming L, Hoffman HJ, Laurence M, Grummer-Strawn A. Breastfeeding and risk of ınfections at 6 years. Pediatrics. 2014;134(1):13–20.
Declarations
Scientific Responsibility Statement
The authors declare that they are responsible for the article’s scientific content including study design, data collection, analysis and interpretation, writing, some of the main line, or all of the preparation and scientific review of the contents and approval of the final version of the article.
Animal and Human Rights Statement
All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Funding
None
Conflict of Interest
The authors declare that there is no conflict of interest.
Ethics Declarations
This study was approved by the Ethics Committee of Muğla Sıtkı Koçman
University (Date: 2022-01-14, No: E-72855364-050.01.04-375108)
Data Availability
The data supporting the findings of this article are available from the corresponding author upon reasonable request, due to privacy and ethical restrictions. The corresponding author has committed to share the de-identified data with qualified researchers after confirmation of the necessary ethical or institutional approvals. Requests for data access should be directed to bmp.eqco@gmail.com
Additional Information
Publisher’s Note
Bayrakol MP remains neutral with regard to jurisdictional and institutional claims.
Rights and Permissions
About This Article
How to Cite This Article
Veli Can Yılmaz, Betül Battaloğlu Inanc, Yaşar Topal. Hospitalized with a lower respiratory tract infection, evaluation of children aged 2-5 in terms of breast milk intake. Ann Clin Anal Med 2025; DOI: 10.4328/ACAM.22503
Publication History
- Received:
- December 7, 2024
- Accepted:
- February 4, 2025
- Published Online:
- March 20, 2025
- Printed:
- November 1, 2025

