Relationship of the atherogenic index of plasma and CHA₂DS₂-VASc scores patients with acute ST-segment elevation myocardial infarction and non-ST-segment myocardial infarction
Aip and cha₂ds₂-vasc in stemi and nstemi patients
Authors
Abstract
Aim This study assessed the relationship between the CHA₂DS₂-VASc score, the atherogenic index of plasma (AIP), monocyte-HDL ratio (MHR), platelet- lymphocyte ratio (PLR), neutrophil-lymphocyte ratio (NLR), and myocardial infarction (MI) types (STEMI/NSTEMI) in emergency department patients, aiming to identify correlations between these parameters.
Methods Conducted as a retrospective study at Kırşehir Training Education and Research Hospital (2020–2023), this research included 200 STEMI patients, 200 NSTEMI patients, and 200 healthy controls.
Results The mean age of participants was 60.70 ± 12.33. Significant differences emerged across groups in CHA₂DS₂-VASc, AIP, PLR, NLR, and MHR. The CHA₂DS₂-VASc score was higher in NSTEMI versus STEMI and controls. AIP was elevated in both MI groups versus controls. MHR was higher in STEMI than in controls, while NLR was elevated in both MI groups. A weak positive correlation existed between CHA₂DS₂-VASc and NLR/PLR and AIP and MHR. Each 1-unit increase in CHA₂DS₂-VASc, AIP, and NLR raised MI risk by 1.60, 3.24, and 2.59 times, respectively, whereas PLR reduced risk by 1.013 times per unit.
Conclusion All atherosclerosis-related inflammatory markers were elevated in MI patients. CHA₂DS₂-VASc showed no significant correlation with AIP but was notably higher in NSTEMI, while AIP was elevated in both MI groups. CHA₂DS₂-VASc demonstrates strong predictive value for NSTEMI in clinical/emergency settings, whereas AIP lacks significance for specific MI subgroups. Broader multicenter studies are required to clarify their utility in MI risk stratification.
Keywords
Introduction
Cardiovascular disease (CVD) is the leading cause of mortality, with 18.6 million deaths worldwide each year, 85% of which are due to ischemic heart disease such as acute coronary syndromes (ACS) 1. Myocardial Infarction (MI) is responsible for 1 in 3 deaths globally, and its incidence is rising rapidly in developing countries due to increasing obesity, diabetes, and sedentary lifestyles (available at: https://www.who.int/data/ gho/data/themes/mortality-and-global-health-estimates/ghe- leading-causes-of-death). The prevalence of MI in Turkey is 3.5%, which is higher than the European average (2.8%) 2.
ST-elevation myocardial infarction (STEMI) and non-ST elevation myocardial infarction (NSTEMI) are critical clinical conditions in the spectrum of ACS that require urgent intervention. STEMI is characterized by complete occlusion of the coronary artery, whereas NSTEMI usually develops due to unstable plaque rupture or partial occlusion 3.
Although traditional risk factors (hypertension, diabetes, hyperlipidemia) play an important role in the pathogenesis of MI, the prognostic value of atherogenic lipid profiles and systemic inflammation has recently come to the fore. The atherogenic index of plasma (AIP) is a marker calculated by logarithmic transformation of the triglyceride/HDL-C ratio and indirectly reflects the presence of small dense LDL particles 4. Similarly, inflammatory markers such as Monocyte/HDL Ratio (MHR), Platelet-Lymphocyte Ratio (PLR), and Neutrophil-Lymphocyte Ratio (NLR) are used to assess endothelial dysfunction and platelet activation 5. Although the CHA₂DS₂-VASc score was initially developed to predict thromboembolic risk in patients with atrial fibrillation (AF), it is also investigated in MI prognosis due to its association with coronary artery disease severity 6. AIP is an index quantifying an atherogenic and anti-atherogenic lipoprotein imbalance. High AIP ( > 0.21) is associated with an increase in small dense LDL particles, which facilitate endothelial penetration and impair plaque stability 7. The Framingham Study reported that AIP correlated with the coronary artery calcium score 8. MHR is a marker reflecting the interaction between systemic inflammation and lipid metabolism. Pro- inflammatory cytokine release by monocytes and decreased anti-inflammatory effect of HDL are associated with coronary microvascular dysfunction and no-reflow phenomenon 9. PLR and NLR are quantitative indicators of inflammatory response. Increased NLR is associated with neutrophil-induced oxidative stress and myocardial reperfusion injury 10. PLR predicts coronary microthrombus formation by reflecting platelet activation 11.
This study aims to comprehensively evaluate the relationship between CHA₂DS₂-VASc score and AIP, MHR, PLR, and NLR and the diagnostic-prognostic value of these parameters in STEMI and NSTEMI patients.
Materials and Methods
Study Design and Population
This retrospective cohort study included 200 STEMI and 200 NSTEMI patients with MI who presented to the Emergency Department of Kırşehir Training and Research Hospital with chest pain between January 2020 and December 2023, and 200 control patients without a history of MI. The control group was matched with the patient groups regarding age ( ± 5 years), gender, and comorbidities (hypertension, diabetes). Patients’ data were obtained from the hospital database, and their files were analyzed.
Patients over 18 years of age who had completed laboratory data (lipid profile, complete blood count, cardiac biomarkers) and were diagnosed with STEMI or NSTEMI according to ESC/ AHA guidelines were included in the study. Patients under 18 years of age, pregnant patients, breastfeeding patients, patients diagnosed with active infection or malignancy, patients diagnosed with chronic renal failure (GFR < 30 mL/min), patients with liver cirrhosis, patients with hormonal disorders, and patients taking lipid-lowering or immunomodulatory drugs were excluded.
Data Collection and Score Calculations
The CHA₂DS₂-VASc Score range is 0-9 and includes the following components: Age (<65: 0, 65-74: +1, ≥75: +2), female gender (+1), hypertension (+1), diabetes mellitus (+1), stroke/TIA (+2), vascular disease (previous MI, peripheral arterial disease or aortic plaque) (+1), congestive heart failure (+1) 12. However, the gender component is the opposite in coronary artery disease, i.e., male gender is considered a risk factor. Therefore, in the CHA₂DS₂-VASc score used in cardiovascular disease studies other than AF, the male gender is given a score of (+1) while the female gender is given a score of (0). In our study, the gender component of the score was calculated by giving (+1) points to the male gender and (0) points to the female gender. AIP: the logarithm of the ratio of plasma triglyceride (TG) level to high-density lipoprotein (HDL) level, measured in milligrams per deciliter, to the base 10 and calculated using the formula [log (TG/HDL-C) ratio]. AIP values <0.11 reflect low, 0.11 - 0.21 moderate, and >0.21 high cardiovascular risk 4. In our study, AIP calculation was performed, and patients were categorized as low, intermediate, and high risk according to the result. MHR, PLR, and NLR were calculated using complete blood count data.
Statistical Analysis
Statistical Package for Social Sciences version 27.0 software for Windows (IBM SPSS Statistics for Windows, Version 21.0. Armonk, NY: IBM Corp., USA) was used for statistical analysis of the study. Arithmetic mean, standard deviation for quantitative data, n (%) frequency tables, and median (Min-Max) values for quantitative discrete and qualitative data were given in the study. Normality tests of continuous data were performed with the help of the Kolmogorov-Smirnov test. One-way ANOVA, Kruskal-Wallis, Pearson or Spearman correlation analysis, ROC analysis, and logistic regression analysis were used to analyze the data. p < 0.05 was considered statistically significant.
Ethical Approval
This study was approved by the Ethics Committee of Ahi Evran University, Faculty of Medicine (Date: 2023-09-05, No: 2023- 15/102).
Results
The mean age of all patients included in the study and the control group was 60.70 ± 12.33. When the demographic characteristics were compared according to the groups, the difference in age, gender, and comorbid conditions was statistically significant. It was found that age was older, and male gender was more common in MI groups. The rates of HT, DM, vascular disease, heart failure, and family history were also higher in the MI groups (Table 1).
When scores and blood values were compared according to the groups, significant differences were found in CHA₂DS₂-VASc, AIP, PLR, NLR, and MHR score values (Table 1).
Post-hoc analyses for the scores showed significant differences between the groups. CHA₂DS₂-VASc score was significantly higher in the NSTEMI group than in the STEMI and control groups. AIP score is statistically significantly higher in both NSTEMI and STEMI groups compared to the control group. MHR is statistically significantly higher in the STEMI group compared to the control group. NLR is statistically significantly higher in both NSTEMI and STEMI groups compared to the control group.
When the correlations between the scores were analyzed, it was found that there was a weak statistically significant positive correlation between CHA₂DS₂-VASc score and NLR and PLR. There was a weak statistically significant correlation between AIP and MHR in a positive direction and a weak statistically significant correlation with PLR in a negative direction.
Logistic regression analysis to predict the risk of STEMI or NSTEMI was found to be significant (omnibus test p < 0.001). The accuracy of the model was 78.5%. The independent variable of the model is the presence of MI (ref: control risk: MI). Independent variables of the model are age, CHA₂DS₂- VASc score, AIP, PLR, NLR, and MHR. The Forward LR method was used, and MHR and age were not found to contribute significantly to the model. A one-unit increase in CHA₂DS₂-VASc score increases the risk of MI by 1.60 times, a one-unit increase in AIP score increases the risk of MI by 3.24 times, a one-unit increase in NLR increases the risk of MI by 2.59 times, and a one-unit increase in PLR decreases the risk of MI by 1.013 times (Table 2).
It was found that the dependent variables did not affect each other, and there was no multicollinearity. Multinomial logistic regression analysis to evaluate the role of scores in predicting MI type was found to be significant (p < 0.001). The model’s independent variables are CHA₂DS₂-VASc score, AIP, PLR, NLR, MHR, and age. The dependent variable of the model is group (ref: control). It was found that MHR and age did not significantly contribute to the model, while the other variables significantly contributed to the model. A one-unit increase in CHA₂DS₂-VASc score increases the risk of STEMI by 1.63-fold, a one-unit increase in AIP score by 3.09-fold, a one-unit increase in NLR by 2.70-fold, while a one-unit increase in PLR decreases the risk of MI by 1.019-fold. A one-unit increase in CHA₂DS₂- VASc score increases the risk of NSTEMI by 1.85 times, a one- unit increase in AIP score by 2.86 times, a one-unit increase in NLR by 2.58 times, while a one-unit increase in PLR decreases the risk of MI by 1.013 times (Table 3).
Discussion
The CHA₂DS₂-VASc score is a scoring system developed to predict thromboembolic risk in patients with AF 13. However, in recent years, studies on its prognostic and diagnostic value in ACS, such as MI, have increased. This study examined the relationships between CHA₂DS₂-VASc score and atherosclerosis markers such as AIP, PLR, NLR, and MHR in STEMI and NSTEMI patients. The CHA₂DS₂-VASc score was statistically significantly higher in the NSTEMI group compared to the STEMI and control group (p < 0.05). The AIP score was higher in both the STEMI and NSTEMI groups than in the control group. MHR was significantly higher in the STEMI group, and NLR was significantly higher than in the control group in both MI groups. There was a weak positive correlation between CHA₂DS₂-VASc score and NLR and PLR (r = 0.2-0.3), a positive correlation between AIP and MHR (r = 0.25), and a negative correlation with PLR (r = -0.18). In the risk increase analyses, a one-unit increase in CHA₂DS₂-VASc score increased the risk of MI 1.60-fold (p < 0.001), AIP 3.24- fold (p < 0.001), NLR 2.59-fold (p < 0.001), while a one-unit increase in PLR decreased the risk 1.013-fold (p = 0.02).
In the literature, the association of CHA₂DS₂-VASc score with clinical outcomes after MI has been addressed in a broad perspective. Kiliszek et al., in a prospective study including 2557 AF patients, reported that the CHA₂DS₂-VASc score was an independent predictor of mortality at 5-year follow-up, and the AUC value reached 0.82 in ROC analysis 14. Zorlu et al. emphasized that the median CHA₂DS₂-VASc score was significantly higher in patients with reperfusion failure after primary PCI (p < 0.001), and a score ≥ 2 predicted reperfusion failure with a sensitivity of 83% 15. In our study, the CHA₂DS₂- VASc score was found to be high in MI patients. Evaluating this score in patients diagnosed in the emergency department and considered for coronary intervention may be important regarding MI and treatment prognosis. Keskin et al. found that 12-month mortality increased to 27.1% in STEMI patients with CHA₂DS₂-VASc score ≥ 4 and AUC = 0.88 (p < 0.001) for in-hospital mortality in ROC analysis 16. In our study, the mortality relationship was not evaluated; however, we think that risk analysis with CHA₂DS₂-VASc score in MI patients admitted to the emergency department may be beneficial in terms of reducing mortality and morbidity. Fang et al. reported that the CHA₂DS₂-VASc score had a moderate predictive value for major adverse cardiovascular events (MACE) in STEMI with AUC = 0.74, and the cut-off value was optimal at 3.5 17.
The CHA₂DS₂-VASc score has also been associated with CAD severity and intracoronary thrombus burden. Kılıç et al. showed that the CHA₂DS₂-VASc-HS score was more effective than the standard score in predicting failed reperfusion after thrombolytic therapy in STEMI (AUC = 0.764 vs. 0.660; p < 0.001) and a cut-off value of ≥3 provided 76% sensitivity 18. The high CHA₂DS₂-VASc score in MI patients in our study may give an idea about the prognosis of our patient group in the light of other studies. Ipek et al. found that the CHA₂DS₂- VASc score was an independent predictor in patients without reperfusion after PCI (OR = 1.58; p < 0.001), and score ≥2 was associated with 66% sensitivity, and in-hospital mortality was also significantly associated with high CHA₂DS₂-VASc scores 19. In conclusion, the CHA₂DS₂- VASc score is associated with a higher risk of non-reperfusion and in-hospital mortality rates in patients undergoing primary PCI. Yasar et al. reported a significant correlation between total coronary occlusion and CHA₂DS₂-VASc score in NSTEMI and that the predictive power increased when combined with the GRACE score 20.
Studies have also focused on the interaction of the score with inflammatory markers. Satılmış et al. reported that high intracoronary thrombus burden was associated with CHA₂DS₂- VASc score, high CRP, and low albumin in NSTEMI 21. Huang et al. emphasized that the CHA₂DS₂-VASc score is superior to the CHADS2 score in predicting coronary lesion severity (AUC = 0.947) and prognosis (AUC = 0.931) in STEMI 22. When the available literature data are evaluated, it is seen that a high CHA₂DS₂-VASc score is an important risk marker associated with poor prognosis in MI patients. In our study, this score was found to be significantly higher in the MI group, suggesting an increased atherosclerotic burden. The findings support the hypothesis that clinical follow-up of high-score patients should be planned more closely. Routine evaluation of CHA₂DS₂-VASc score in MI patients presenting to the emergency department may play a critical role in personalizing treatment strategies and prognosis prediction.
Limitations
The limitations include its single-center retrospective design, possible shortcomings in the data collection process, and the possibility that fasting/fasting status may affect lipid profiles. However, the findings support that the CHA₂DS₂-VASc score may be a practical tool in the clinic for risk stratification, determination of reperfusion strategies, and mortality prediction in MI patients presenting to the emergency department. It has been suggested that approaches such as early invasive intervention or intensive medical therapy may reduce morbidity, especially in patients with high scores 14,17. Future studies are recommended to investigate the predictive value of this score in combination with other biomarkers (e.g., hs-CRP) and validate it in prospective multicenter cohorts.
Conclusion
CHA₂DS₂-VASc score, AIP, MHR, PLR, and NLR have proven to be important markers in MI diagnosis and risk stratification. Combining these parameters can be used as a noninvasive, cost-effective, and practical risk assessment tool. Further studies are recommended to investigate the association of these markers with long-term clinical outcomes and integrate them into treatment strategies.
Tables
Table 1. Characteristics of the patient and control groups and comparison of scores and blood-derived ratio indices according to groups
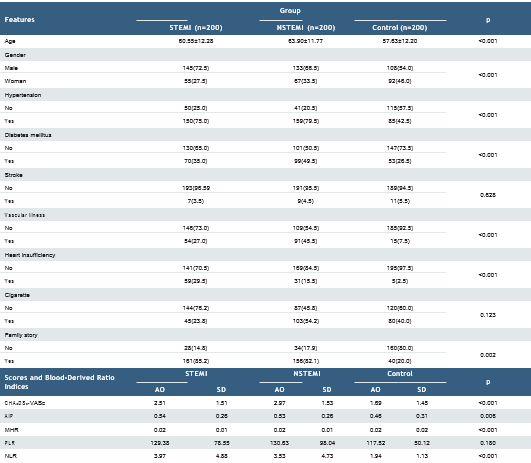
AO: Arithmetic mean, SD: Standard deviation
Table 2. MI risk estimated logistics regression analysis
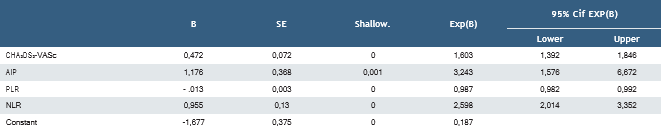
Table 3. Multinomial regression analysis control according to STEMI and NSTEMI estimated
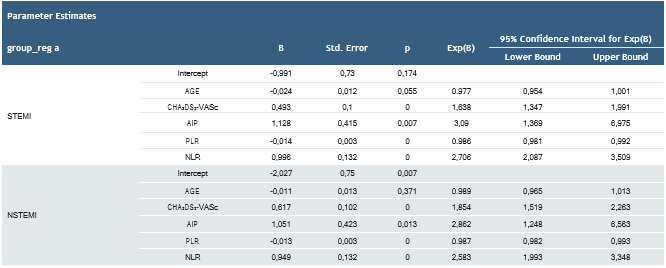
a. The reference category is: Control
References
-
Roth GA, Mensah GA, Johnson CO, et al. Global burden of cardiovascular diseases and risk factors, 1990–2019. J Am Coll Cardiol. 2020;76(25):2982-3021.
-
Onat A, Senocak MS, Surdum-Avci G, Ornek E. Prevalence of coronary heart disease in Turkish adults [Türk erişkinlerinde koroner kalp hastalığı prevalansı]. Arch Turk Soc Cardiol. 2019;47(4):328-35.
-
Amsterdam EA, Wenger NK, Brindis RG, et al. 2014 AHA/ACC guideline for the management of patients with Non-STelevation acute coronary syndromes. J Am Coll Cardiol. 2014;64(16):e139-e228.
-
Dobiásová M, Frohlich J. Atherogenic index of plasma [log(Triglycerides/HDL-Cholesterol)]. Clin Biochem. 2001;34(7):583-8.
-
Cetin MS, Ozcan Cetin EH, Kalender E, et al. Monocyte to HDL cholesterol ratio predicts coronary artery disease severity and future major cardiovascular adverse events in acute coronary syndrome. Heart Lung Circ. 2016;25(11):1077-86.
-
Lip GY, Nieuwlaat R, Pisters R, Lane DA, Crijns HJ. Refining clinical risk stratification for AF using CHA2DS2-VASc. Chest. 2010;137(2):263-72.
-
Wu J, Zhou Q, Wei Z, Wei J, Cui M. Atherogenic index of plasma predicts coronary artery disease. Front Cardiovasc Med. 2021;8:817441.
-
Ikezaki H, Lim E, Cupples LA, Liu CT, Asztalos BF, Schaefer EJ. Small dense LDL and atherogenesis. J Am Heart Assoc. 2021;10(10):e019140.
-
Karataş MB, Çanga Y, Özcan KS, et al. Monocyte to high-density lipoprotein ratio as a new prognostic marker in patients with STEMI undergoing primary percutaneous coronary intervention. Am J Emerg Med. 2016;34(2):240-4.
-
Tamhane UU, Aneja S, Montgomery D, Rogers EK, Eagle KA, Gurm HS. Association between admission neutrophil to lymphocyte ratio and outcomes in patients with acute coronary syndrome. Am J Cardiol. 2008;102(6):653-7.
-
Azab B, Shah N, Akerman M, McGinn JT Jr. Value of Platelet/Lymphocyte Ratio as a predictor of all-cause mortality after non-STelevation myocardial infarction. J Thromb Thrombolysis. 2012;34(3):326-34.
-
Gage BF, Waterman AD, Shannon W, Boechler M, Rich MW, Radford MJ. Validation of clinical classification schemes for predicting stroke: Results from the national registry of atrial fibrillation. JAMA. 2001;285(22):2864-70.
-
Saliba W, Gronich N, Barnett-Griness O, Rennert G. Usefulness of CHADS2 and CHA2DS2-VASc scores in the prediction of new-onset atrial fibrillation: A population-based study. Am J Med. 2016;129(8):843-9.
-
Kiliszek M, Szpakowicz A, Filipiak KJ, et al. CHA2DS2-VASc and R2CHA2DS2- VASc scores have predictive value in patients with acute coronary syndromes. Pol Arch Med Wewn. 2015;125(7-8):545-52.
-
Zorlu Ç, Köseoğlu C. Comparison of RCHA2DS2-VASc score and CHA2DS2- VASc score prediction of no-reflow phenomenon in patients with ST-segment elevation myocardial infarction [ST segment yükselmeli miyokart enfarktüsü olan hastalarda ‘no reflow’ öngörmede RCHA2DS2-VASc skoru ve CHA2DS2-VASc skorlarının karşılaştırılması]. Turk Kardiyol Dern Ars. 2020;48(7):664-72.
-
Keskin K, Sezai Yıldız S, Çetinkal G, et al. The value of CHA2DS2-VASC score in predicting all-cause mortality in patients with ST-segment elevation myocardial infarction who have undergone primary percutaneous coronary intervention. Acta Cardiol Sin. 2017;33(6):598-604.
-
Fang C, Chen Z, Zhang J, Jin X, Yang M. Association of CHA2DS2-VASC score with in-hospital cardiovascular adverse events in patients with acute ST-segment elevation myocardial infarction. Int J Clin Pract. 2022;2022:3659381.
-
Kilic S, Kocabas U, Can LH, Yavuzgil O, Çetin M, Zoghi M. Predictive value of CHA2DS2-VASc and CHA2DS2-VASc-HS scores for failed reperfusion after thrombolytic therapy in patients with ST-segment elevation myocardial infarction. Cardiol J. 2019;26(2):169-75.
-
Ipek G, Onuk T, Karatas MB, et al. CHA2DS2-VASc score is a predictor of no-reflow in patients with ST-segment elevation myocardial infarction who underwent primary percutaneous intervention. Angiology. 2016;67(9):840-5.
-
Yaşar E, Bayramoğlu A, Karakuş Y, Çakmak T. The CHA2DS2-VASc risk score predicts total occlusion in infarct-related arteries in patients with non-ST elevation myocardial infarction. Angiology. 2022;73(4):380-6.
-
Satılmış S, Durmuş G. Predictive accuracy of CHA2DS2-VASc score in determining the high thrombus burden in patients with non-STelevation myocardial infarction. Acta Cardiol. 2021;76(2):140-6.
-
Huang X, Lv H, Liu Z, Liu Y, Yang X. Study on the predictive ability of emergency CHADS2 score and CHA2DS2-VASc score for coronary artery disease and prognosis in patients with acute ST-segment elevation myocardial infarction. J Thorac Dis. 2022;14(7):2611-20.
Declarations
Scientific Responsibility Statement
The authors declare that they are responsible for the article’s scientific content, including study design, data collection, analysis and interpretation, writing, and some of the main line, or all of the preparation and scientific review of the contents, and approval of the final version of the article.
Animal and Human Rights Statement
All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Funding
None
Conflict of Interest
The authors declare that there is no conflict of interest.
Ethics Declarations
This study was approved by the Ethics Committee of Ahi Evran University (Date: 2023-09-05, No: 2023-15/102)
Acknowledgment
This study has been prepared as a part of Dr. Samet Altunbaş’s dissertation. The authors would like to acknowledge helpful and insightful anonymous reviewer comments and recommendations. The authors declare that there is no conflict of interest.
Data Availability
The data supporting the findings of this article are available from the corresponding author upon reasonable request, due to privacy and ethical restrictions. The corresponding author has committed to share the de-identified data with qualified researchers after confirmation of the necessary ethical or institutional approvals. Requests for data access should be directed to bmp.eqco@gmail.com
Additional Information
Publisher’s Note
Bayrakol MP remains neutral with regard to jurisdictional and institutional claims.
Rights and Permissions
About This Article
How to Cite This Article
Samet Altunbaş, Hacı Mehmet Çalışkan, Erdoğan Sökmen, Burak Şahin, Ömer Jaradat. Relationship of the atherogenic index of plasma and cha₂ds₂-vasc scores in patients with acute st-segment elevation myocardial infarction and non-st-segment myocardial infarction. Ann Clin Anal Med 2025; DOI: 10.4328/ ACAM.22652
Publication History
- Received:
- March 15, 2025
- Accepted:
- April 15, 2025
- Published Online:
- April 23, 2025
- Printed:
- November 1, 2025

