The effectiveness of shock indices in predicting mortality in acute pulmonary embolism
Shock indices in pulmonary embolism
Authors
Abstract
Aim Shock indices are important markers in predicting mortality in patients with acute pulmonary embolism. Existing studies on the subject are few. Objectives: Comparison of the predictive power of shock indices for mortality in acute pulmonary embolism patients presenting to the emergency room.
Materials and Methods This was a retrospective study, and shock indices were calculated based on the vital signs of the patients during admission to the emergency room. The diagnostic abilities of shock indices to predict mortality were compared.
Results In this study, 150 adult patients diagnosed with acute pulmonary embolism were examined. Among acute pulmonary embolism patients, 135 (90%) survived, 15 (10%) died. The best shock indices to predict mortality in acute pulmonary embolism patients were diastolic shock index (DSI), modified shock index (MSI), reverse shock index (rSI), and shock index (SI). The optimal cut-off value for DSI was 1.43, and its area under the curve (AUC): 0.952, 95% confidence interval (CI): 0.914-0.989, p˂0.001, sensitivity 100%, specificity 81.48%, positive predictive value (PPV) 37.50%, negative predictive value (NPV) 100%. The optimal cut-off value for MSI was 1.20, and it was AUC: 0.943, 95% CI: 0.898-0.988, p˂0.001, sensitivity 93.33%, specificity 83.70%, PPV 38.89%, NPV 99.12%. The optimal cut-off value for SI was 0.95, and it was AUC: 0.926, 95% CI: 0.865 - 0.987, p˂0.001, sensitivity 86.67%, specificity 87.41%, PPV 43.33%, NPV 98.33%.
Discussion The ability of DSI, MSI, SI, and rSI to predict mortality in acute pulmonary embolism patients was excellent, and DSI was the best among the shock
indices studied.
Keywords
Introduction
The annual occurrence of pulmonary embolism (PE) is 39-115 per 100,000 people. It is the third most common cardiovascular syndrome after stroke and myocardial infarction and is a clinical condition with high mortality and morbidity [1].
In acute pulmonary embolism (APE), there is a boost in pulmonary vascular resistance and pulmonary artery pressure due to occlusion of the pulmonary artery tree by the thromboembolic plug [1]. This leads to increased volume and pressure in the right ventricle, myocyte tension, decreased wall thickness, and compression of the interventricular septum towards the left ventricle [1, 2]. As a result, left ventricular end-diastolic volume decreases, cardiac output decreases, and hypotension and hemodynamic shock develop [1]. These pathophysiologic events that develop in APE are considered the main cause of death in severe PE [1, 2]. In high-risk PE patients, hypotension is considered a diagnostic criterion of hemodynamic instability and determines the treatment modality of PE [1].
Shock index (SI) is achieved by splitting heart rate (HR) by systolic blood pressure (SBP). The power of shock indices to predict prognosis and mortality in emergency departments has been proven by studies conducted in myocardial infarction, PE, trauma, hemorrhage, sepsis, obstetric and pediatric patient groups [3]. When previous studies are analyzed, it is seen that the prognostic significance of SI, age shock index (ASI), and modified shock index (MSI) have been compared in APE patients, but other shock indices have not been compared [4, 5, 6]. The purpose of this study compare the predictive power of SBP, diastolic blood pressure (DBP), mean arterial pressure (MAP), SI, ASI, diastolic shock index (DSI), MSI, age-modified shock index (MSIA), rivers shock index (rSI), rSI times age (rSIA), pulmonary embolism severity index (PESI) for hospital mortality in APE patients presenting to the emergency room (ER).
Materials and Methods
Study Design
This study is retrospective and examines patients admitted to Dicle University Hospital emergency room and diagnosed with pulmonary embolism. Before starting the study, approval was received from the institutional ethics committee.
Emergency Service Management
Patients admitted to the ER were examined, detailed history was taken, examined and vital signs were checked. Diagnosis and treatment of patients in the ER were performed according to the European Society of Cardiology (ESC) guideline [1]. Computed tomography pulmonary angiography (CTPA) was performed in patients with suspected pulmonary embolism using Wells criteria or revised Geneva score clinical decision rules, and the diagnosis was made [1]. Oxygen support was provided in APE patients admitted to the emergency department with SaO2 <90%. Patients were treated with parenteral anticoagulants (intravenous anfractionated heparin or subcutaneous low molecular weight heparin) at therapeutic doses. Acute high- risk pulmonary embolism patients were provided with volume, vasopressor, and inotropic support. Thrombolytic therapy was initiated in hemodynamically unstable pulmonary embolism patients (unless thrombolytic therapy was contraindicated). Patients were hospitalized, and their follow-up and treatment continued.
Study Population and Inclusion Criteria
A total of 210 adult patients above 18 years presenting to the ER between January 2016 and December 2019 and diagnosed with PE were consecutively analyzed. We excluded 60 patients who were sent to our hospital after being admitted to another center, who were sent from our hospital to another treatment center, who had cardiopulmonary arrest while presenting to the ER, and who had incomplete or inaccurate patient data. A total of 150 patients who were admitted directly to the ER, diagnosed with primary PE, and hospitalized for treatment were taken into research (Fig. 1).
Data collection and variables
Patient information was received from the electronic hospital record system by reviewing patient files. Age, gender, presenting symptoms, comorbidities, PE risk factors, Wells and revised Geneva scores, HR, SBP, DBP, intensive care unit stay, and survival data were recorded. PESI score was calculated [2]. MAP, SI, ASI, DSI, MSI, MSIA, rSI, and rSIA shock indices were calculated based on the patient’s vital signs while presenting to the ER.
The studied parameters were calculated as follows.
MAP = (SBP + 2 × DBP) / 3
SI = HR / SBP
ASI = Age × SI
DSI = HR / DBP
MSI = HR / MAP
MSIA = MSI × Age
rSI = SBP / HR
rSIA = rSI × Age
Statistical Analyses
If numerical continuous variables were normally distributed, Student’s t-test was applied. They were shown as mean and standard deviation (mean ± SD). If numerical continuous variables were abnormally distributed, the Mann-Whitney U-test was applied. They were shown as the median, interquartile range (IQR, q1 - q3). The chi-square test (χ2) test was applied for categorical data, and they were shown with frequency and percentage. The diagnostic decision-making properties of SBP, DBP, MAP, SI, ASI, DSI, MSI, MSIA, rSI, rSIA, shock indices, and PESI in predicting mortality in APE patients were analyzed by receiver operating characteristic (ROC) curve analysis. The accuracy of the parameter in predicting mortality outcomes was defined as the area under the curve (AUC). The best cut-off point, sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV) were determined. A value of p < 0.05 was accepted as statistically meaningful. IBM SPSS 21.0 for the Windows statistical package program was used.
Ethical Approval
This study was approved by the Ethics Committee of Dicle University, Faculty of Medicine with the date and session number (Date: 2023-04-12, No: 115 ).
Results
Of the PE patients, 135 (90%) survived, and 15 (10%) died. The median age of all patients was 58.50 (42 - 73) years, the median age of the living patients was 58 (40.50 - 72) years, and the median age of the deceased patients was 64 (44.50 - 77) years. Statistically, age did not affect mortality (p = 0.194). Of the PE patients, 59 (39.3%) were male and 91 (60.7%) were female. Gender did not affect mortality (p = 0.373). The mean ± standard deviation comparison of rSI in the living and deceased patients was 1.372 ± 0.301- 0.836 ± 0.222. Comparison of median (q1-q3) values in living and deceased patients; HR 86 (78 - 98) - 122 (108 - 132), SBP 120 (110 - 130) - 100 (80 - 110), DBP 70 (70 - 80) -60 (50 - 70), MAP 86.70 (80 - 96.70) - 66.70 (60 - 98), SI 0.74 (0.64 - 0.84) - 1.16 (0.96 - 1.55), ASI 42.83 (30. 40 - 54) - 71.68 (54.92 - 111.32), DSI 1.17 (1.02 - 1.36) - 2.24 (1.51 - 2.52), MSI 0.97 (0.85 - 1.11) - 1.80 (1.27 - 2.06), MSIA 58.50 (40.71 - 70.89) - 114. 23 (72.50 - 158.79), rSIA 76.08 (50.90 - 97.50) - 47.86 (37.82 - 59.15), PESI 83 (64 - 99) -111 (103 - 143.50). When the vital parameters were analyzed, SI, ASI, DSI, MSI, MSIA, and PESI values were higher in the deceased and were the factors affecting mortality (p < 0.001). SBP, DBP, MAP, rSI, and rSIA values were lower in those who died and were the factors affecting mortality (p = 0.001 for rSIA, p < 0.001 for others) (Tab. 2).
AUC, confidence interval ( 95% CI): lower bound - upper bound of SBP, DBP, MAP and shock indices; SBP (AUC: 0.784, 95% CI: 0.637 - 0.931), DBP (AUC: 0.825, 95% CI: 0.702 - 0.948), MAP
(AUC: 0.830, 95% CI: 0.694 - 0.967), SI (AUC: 0.926, 95% CI: 0.865 - 0.987), ASI (AUC: 0.846, 95% CI: 0.730 - 0.961), DSI (AUC: 0.952, 95% CI: 0.914 - 0.989), MSI (AUC: 0.943, 95% CI: 0.898 - 0.988), MSIA (AUC: 0.858, 95% CI: 0.747 - 0.968), rSI (AUC: 0.926, 95% CI: 0.865 - 0.987), rSIA (AUC: 0.760, 95% CI: 0.661 - 0.859), PESI (AUC: 0.806, 95% CI: 0.686 - 0.925). The p-value was p = 0.001 for rSIA, and the p-value was p < 0.001 for others (Tab. 3). DSI, MSI, SI, and rSI had the best AUC values among the shock indices. (Fig. 2).
Discussion
Pathophysiologic events developing due to APE affect the cardiovascular system and cause hemodynamic instability. Hypotension in APE patients is considered a poor prognosis criterion [1]. SBP, DBP, and HR are frequently used and easily accessible vital signs to predict the prognosis of patients in emergency departments. This study determined that shock indices calculated using SBP, DBP, and HR at the time of presentation to the ER were superior to these classical vital parameters in predicting mortality in APE patients. DSI was the most successful in predicting mortality in APE patients of the shock indices analyzed in this review. Then, the shock indices with the highest ability to predict mortality were MSI, SI, and rSI, respectively. The ability of DSI, MSI, SI, and rSI to predict mortality in APE patients was excellent. These shock indices were superior to both classical vital parameters and PESI scores.
In APE patients, SI ≥ 1 was associated with increased mortality independent of echocardiographic findings [7]. In another study of APE patients, SI was significantly successful in predicting hospital mortality, myocardial necrosis, and right ventricular dysfunction [8]. Otero et al. found SI ≥ 1, SBP < 100 mmHg, and SBP < 90 mmHg to be independent predictors of 30-day mortality in APE patients. The AUC (95% CI) values were 0.79 (0.77 - 82), 0.78 (0.75 - 0.80), and 0.77 (0.75 - 0.8), respectively [9]. In another prospective study of APE patients with SBP ≥ 90 mmHg admitted to the ER, SBP, HR, SI, and PESI scores were associated with 30-day mortality. For SI > 1, AUC was 0.84, sensitivity 80%, specificity 83.3%, PPV 52.2%, NPV 94.8%. For the PESI cut-off value of 114, AUC: 0.79, sensitivity 100%, specificity 56.6%, PPV 34.1%, NPV 100% [6]. In a study of APE patients presenting to the ER, SI and ASI were superior to PESI scores in predicting mortality [10]. In the study by Gökçek et al., ASI was the best determinant of mortality in APE patients, while the PESI score was superior to MSI and SI [4]. According to studies examining APE patients, shock indices were superior to classical vital parameters in predicting mortality. Shock indices showed differences in predicting mortality when compared with the PESI score. This study shows similarities and differences with the literature in many aspects. This may be explained by the different methods employed in the studies.
In the study by Gökçek et al., the ASI cut-off value for 54 was AUC: 0.90, sensitivity 76%, specificity 82%, PPV 18%, NPV 95%; the PESI cut-off value for 144 was AUC: 0.84, sensitivity 69%, specificity 70%, PPV 13%, NPV 90%; AUC for MSI cut-off value 0.90 was 0.75, sensitivity 76%, specificity 73%, PPV 15%, NPV 88%; AUC for SI cut-off value 0.82 was 0.72, sensitivity 74%, specificity 78%, PPV 12%, NPV 91% [4]. In the study by Kara et al., the ASI cut-off value for 66.6 was AUC: 0.825, sensitivity of 80%, specificity 72%; the SI cut-off value for 0.97 was AUC: 0.824, sensitivity 93%, specificity 65% [10]. In both studies examining APE patients, the prediction power of ASI, MSI, and SI for mortality was good to moderate. In this review, the prediction power of MSI and SI was excellent, and ASI was good.
In a study comparing shock indices in predicting hospital mortality in patients with ST-segment elevation myocardial infarction, MSIA was significant (AUC: 0.813, 95% CI 0.787 - 0.837) [11]. In a study examining shock indices in acute decompensated heart failure, the MSIA cut-off value for 66.7 was AUC: 0.659 (95% CI: 0.622 - 0.696), sensitivity 62%, specificity 60% [12]. In this review, the optimal cut-off value of MSIA was higher, and its power to predict mortality was better in APE patients.
There is a direct relationship between DBP and arterial vasomotor tone, which is the essence of DSI [13]. DBP is influenced by the duration of the cardiac cycle, ejection fraction, arterial compliance, and prolonged diastole duration, resulting in lower DBP. Under pathologic conditions, simultaneous low DBP, increased heart rate, and prolonged diastole duration result in severe impairment of cardiovascular function [14]. Kim et al. found DSI and lactate levels to be moderately effective in predicting the need for vasopressors in hypotensive patients with suspected infection in a study conducted in the emergency department [15]. Avci et al. found AUC: 0.737 (95% CI: 0.705 - 0.767), sensitivity 70.92%, specificity 72.63%, PPV 65.3%, NPV 77.5% for DSI > 1.35 to predict mortality in COVID-19 pneumonia [16]. In this study, DSI was the highest-quality predictor of mortality in APE patients.
In a study of trauma patients presenting to the ER, an rSI < 1, even without hypotension, was an indicator of poor outcome [17]. In this study, the predictive power of rSI for mortality in APE patients was high.
MSIA, DSI, and rSI shock indices have not been previously studied in APE patients. These shock indices were good or excellent in predicting mortality in this study. The variables in this study show similar relationships with the literature. However, in this study, classical vital parameters and PESI score were good at predicting mortality, whereas DSI, MSI, SI, and rSI had excellent ability. Different cut-off values, mortality durations, and patient groups may explain these differences.
Limitations
This study had some limitations. First, it was a single-center and retrospective cross-sectional study. Second, the number of patients analyzed was small. Third, the history of anti- hypertensive anti-arrhythmic drug intake of the patients in the study was unknown. Fourth, the study only examined hospital mortality and not a long life span. Fifth, the vital parameters of the patients were measured by different health personnel. However, the devices used for measurement were the same. Therefore, the results of the study cannot be generalized. For this, multicenter and comprehensive studies are needed.
Conclusion
This study revealed that shock indices calculated at the time of presentation to the ER have diagnostic value in predicting mortality in APE patients. DSI, MSI, SI, and rSI had excellent ability to predict mortality in APE patients, and DSI was the highest of the shock indices studied.
Figures
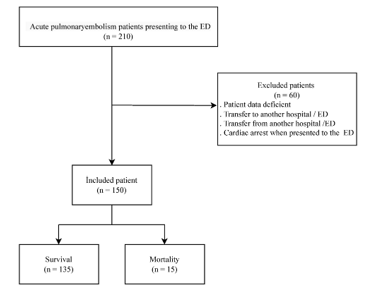
Figure 1. Flowchart of this research
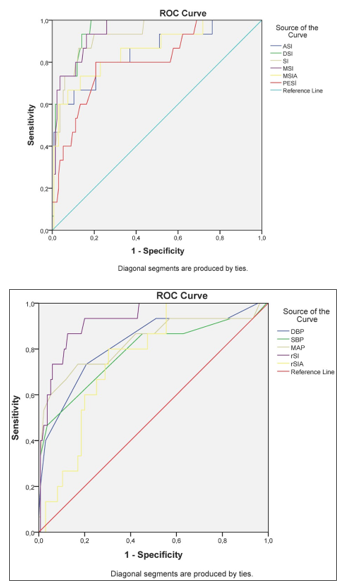
Figure 2. AUC value of shock indices in predicting the mortality of pumonary embolism patients. a; ROC curve of ASI, DSI, SI, MSI, MSIA, PESI. b; ROC curve of DBP, SBP, MAP, rSI, rSIA
Tables
Table 1. Clinical characteristics of pulmonary embolism patients
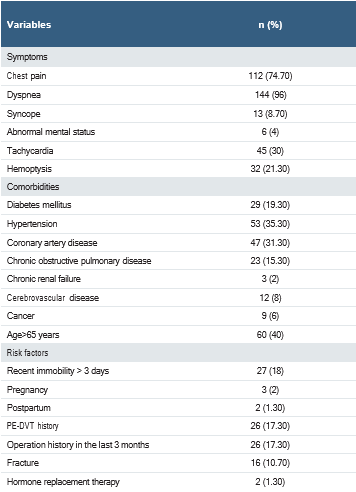
Abbreviations: PE, pulmonary embolism; DVT, deep-vein thrombosis
Table 2. Distribution of shock indices according to mortality
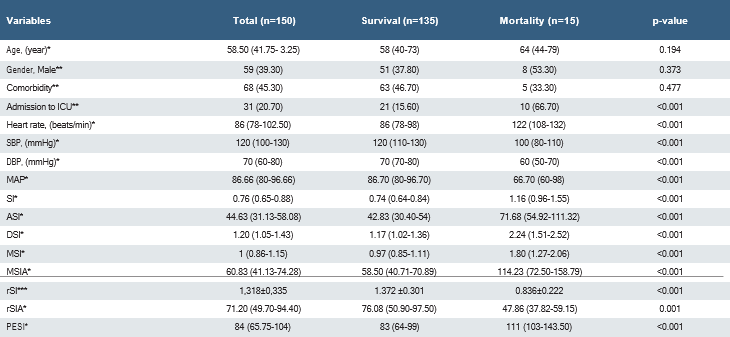
Abbreviations: ICU: intensive care unit; DBP, diastolic blood pressure; SBP, systolic blood pressure; MAP, mean arterial pressure; SI, shock index; DSI, diastolic shock index; MSI, modified shock index; ASI, age shock index; rSI, reverse shock index; MSIA, MSI multiplied by age; rSIA, rSI multiplied by age; PESI, pulmonary embolism severity index. *: median (interquartile range); **: n (%); ***: mean ± standard deviation
Table 3. Optimal cut-point values in predicting hospital mortality for shock indices in pulmonary embolism patients
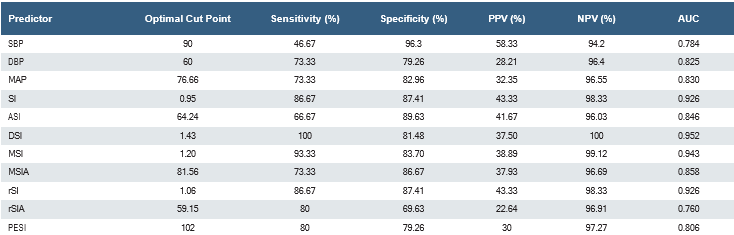
Abbreviations: PPV, positive predictive value; NPV, negative predictive value; AUC, area under the curve.
References
-
SV Konstantinides, G Meyer, C Becattini, et al. 2019 ESC Guidelines for the diagnosis and management of acute pulmonary embolism developed in collaboration with the European Respiratory Society (ERS). Eur Heart J. 2020;41(4):543-603.
-
Huisman MV, Barco S, Cannegieter SC, et al. Pulmonary embolism. Nat Rev Dis Primers. 2018;4(18028):1-17.
-
Koch E, Lovett S, Nghiem T, Riggs RA, Rech MA. Shock index in the emergency department: utility and limitations. Open Access Emerg Med. 2019;11:179-199.
-
Gökçek K, Gökçek A, Demir A, Yıldırım B, Acar E, Alataş OD. In-hospital mortality of acute pulmonary embolism: Predictive value of shock index, modified shock index, and age shock index scores. Med Clin. 2022;158(8):351-5.
-
Spampinato MD, Covino M, Passaro A, et al. Predicting in-hospital mortality in pulmonary embolism patients: development and external validation of the PATHOS score Clin Exp Emerg Med. 2023;10(1):26-36.
-
Çağlar A, Akıllı NB, Köylü R, Alpaydın MS. Jugular vein diameter: A new player in normotensive pulmonary embolism. Clin Imaging. 2021;74:4-9.
-
Toosi MS, Merlino JD, Leeper KV. Prognostic Value of the Shock Index Along With Transthoracic Echocardiography in Risk Stratification of Patients With Acute Pulmonary Embolism. Am J Cardiol. 2008;101(5):700-5.
-
Keller K, Coldewey M, Geyer M, Beule J, Balzer JO, Dippold W. Shock index for outcome and risk stratification in acute pulmonary embolism. Artery Research. 2016;15: 30-5.
-
Otero R, Trujillo-Santos J, Cayuela A, et al. Hemodynamically unstable pulmonary embolism in the RIETE Registry: systolic blood pressure or shock index? Eur Respir J. 2007 30(6): 1111-6.
-
Kara H, Degirmenci S, Bayir A, Ak A. Pulmonary embolism severity index, age-based markers and evaluation in the emergency department. Acta Clin Belg. 2015; 70(4):259-64.
-
Zhou J, Shan PR, Xie QL, et al. Age shock index and age-modified shock index are strong predictors of outcomes in ST-segment elevation myocardial infarction patients undergoing emergency percutaneous coronary intervention. Coron Artery Dis. 2019;30(6):398-405.
-
Bondariyan N, Vakhshoori M, Sadeghpour N, Shafie D. Prognostic value of shock index, modified shock index, and age-adjusted derivatives in prediction of in-hospital mortality in patients with acute decompensated heart failure: Persian registry of cardiovascular disease/heart failure study. Anatol J Cardiol. 2022;26(3):210-7.
-
Dalmau R. The diastolic shock index works…but what is it? Ann Intensive Care. 2020;10(103):1-2.
-
Ospina-Tascón GA, García-Gallardo G, Orozco N. Using the diastolic shock index to determine when to promptly administer vasopressors in patients with septic shock. Clin Exp Emerg Med.2022;9(4):367-9.
-
Kim DS, Park JE, Hwang SY, et al. Prediction of vasopressor requirement among hypotensive patients with suspected infection: usefulness of diastolic shock index and lactate. Clin Exp Emerg Med. 2022;9(3):176-86.
-
Avci M, Doganay F. Prognostic performance of shock index, diastolic shock index, age shock index, and modified shock index in COVID-19 pneumonia. Disaster Med Public Health Prep. 2022;17(e189):1-6.
-
Lai WH, Wu SC, Rau CS, Kuo PJ, Hsu SY, Chen YC. Systolic blood pressure lower than HR upon arrival at and departure from the emergency department ındicates a poor outcome for adult trauma patients. Int J Environ Res Public Health. 2016;13(6):528.
Declarations
Scientific Responsibility Statement
The authors declare that they are responsible for the article’s scientific content, including study design, data collection, analysis and interpretation, writing, and some of the main line, or all of the preparation and scientific review of the contents, and approval of the final version of the article.
Animal and Human Rights Statement
All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Funding
None
Conflict of Interest
The authors declare that there is no conflict of interest.
Ethics Declarations
This study was approved by the Ethics Committee of Dicle University, Faculty of Medicine (Date: 2023-04-12, No: 115)
Data Availability
The data supporting the findings of this article are available from the corresponding author upon reasonable request, due to privacy and ethical restrictions. The corresponding author has committed to share the de-identified data with qualified researchers after confirmation of the necessary ethical or institutional approvals. Requests for data access should be directed to bmp.eqco@gmail.com
Additional Information
Publisher’s Note
Bayrakol MP remains neutral with regard to jurisdictional and institutional claims.
Rights and Permissions
About This Article
How to Cite This Article
Mustafa İçer, Veysi Tekin. The effectiveness of shock indices in predicting mortality in acute pulmonary embolism. Ann Clin Anal Med 2025; DOI: 10.4328/ ACAM.22519
Publication History
- Received:
- December 10, 2024
- Accepted:
- January 23, 2025
- Published Online:
- March 20, 2025
- Printed:
- November 1, 2025

