Evaluation of end-expiratory lung volume, gain and pulmonary mechanics with PEEP titration in mechanical ventilation of intensive care unit patients
EELV, gain and pulmonary mechanics
Authors
Abstract
Aim Mechanical ventilation is an integral part of intensive care treatment. A wide variety of parameters have been investigated until today in order to direct mechanical ventilation in intensive care units. In patients who are controlled ventilated by mechanical ventilator; individualized optimal selection of positive end-expiratory pressure (PEEP) is important to protect the lung from ventilation-related trauma, to gain atelectatic areas and to prevent the closing of ventilated lung areas.
Materials and Methods In this study, 20 patients followed up with a mechanical ventilator in the intensive care unit of a university were included. In our study, Functional residual capacity (FRC), end-expiratory lung volume (EELV), gain and respiratory mechanics were investigated with increased PEEP titration procedure in patients undergoing controlled mechanical ventilation in the intensive care unit. FRC and EELV were measured by the multiple breath nitrogen wash out technique. Gain and compliance evaluations were made on the dynamic pressure-volume curves created with the intratracheal pressure sensor.
Result It was observed that FRC, EELV, the volume change measurements on dynamic pressure-volume curves and gain measurements are easily applicable at the bedside. Optimal PEEP values; 5 ± 3.62 cmH2O for static compliance, 4.75 ± 3.79 cmH2O for elastance, 4.75 ± 3.43 cmH2O for driving pressure. The optimal PEEP according to the gain was determined as 11.75 ± 3.35 cmH2O. EELV reached the predicted FRC values at an average PEEP level of 4.06 ± 5.83 cmH2O.
Discussion It was found that the gain did not significantly correlate with compliance, elastance, and driving pressure and was not sensitive to lung distension.
Keywords
Introduction
Alveolar collapse, pulmonary oedema, pulmonary inflammation, decreased thoracic compliance are common causes of decreased functional residual capacity (FRC). Positive end-expiratory pressure (PEEP) and alveolar recruitment manoeuvres are very important principles of ventilation strategy [1]. Different indicators such as static pressure/volume curve, upper and lower inflation points or alveolar pressure/volume curve have been used to determine FRC [2, 3]. Many methods have been investigated to reach the ideal method in PEEP titration. A PEEP value at which maximum oxygen (O2) transport coincided with the highest static compliance and the highest FRC was defined, and it was shown that maximal ΔEELV/ΔPEEP and maximal respiratory system compliance were at the same PEEP level [4, 5]. Therefore, theoretically, measuring and monitoring FRC or end-expiratory lung volume (EELV) when PEEP is used may be a valuable tool to optimise respiratory settings in mechanical ventilation [6].
Stenqvist et al. [7] introduced a new method to measure FRC without interruption of mechanical ventilation, based on a simplified and modified nitrogen multiple breath washout (NMBW) technique integrated into a now commercially available intensive care unit ventilator [7]. This method requires a step change in the fraction of inspired oxygen (FiO2) without the need for additional tracer gases or special additional monitoring equipment. Theoretically, FRC can vary with body position, sedation level, intra-abdominal pressure, ventilation mode and ventilator settings, PEEP level and amount of atelectasis [8].
Measurement of EELV may be important during PEEP titration. However, a PEEP-induced increase in EELV may be the result of alveolar recruitment or may be the result of overdistension of open alveoli. Therefore, EELV alone may not be sufficient to assess PEEP response and should be combined with compliance [9]. Gattinoni and Pesenti introduced the concept of lung stress and strain [10]. Stress is defined as transpulmonary pressure. Strain is defined as the change in the size of the lung compared to the baseline state of the lung at rest. The ratio of stress and strain is the lung elastance, which is assumed to be constant or within narrow limits in ARDS. With FRC and tidal volume, stress and strain can be calculated. Therefore, FRC can be the basis for adjustment of lung protective ventilation.
Determining the optimum PEEP level in intensive care unit patients is critical for ventilator management. The aim of our study was to evaluate the volume gain at different PEEP levels compared to the previous level on the pressure-volume curve, FRC-EELV change measured by modified multiple nitrogen flushing technique and compliance. In our study, we aimed to evaluate the usability of FRC-EELV measurement and volume gain for bedside PEEP titration in the clinic.
Materials and Methods
This study was conducted in the anaesthesiology and reanimation intensive care units of a university between November 2019 and March 2021. 22 patients over 18 years of age, without primary lung disease, intubated and receiving controlled mechanical ventilation were included in the study. Patients with severe cardiovascular instability, pneumothorax, pneumonectomy operation, lung transplantation, severe airway obstruction due to chronic obstructive pulmonary disease, thoracic deformity, acute respiratory distress syndrome, and spontaneous breathing in CPAP mode of mechanical ventilator or T-tube were excluded. Relatives of all patients were informed clearly and in detail before the study. Written informed consent was obtained. During the study, oxygen consumption (VO2) and carbon dioxide production (VCO2) measurements did not reach the desired steady state in one patient, and haemodynamic instability developed in another patient during measurement. Therefore, they were excluded from the study. Data were analysed in 20 patients.
Patients included in the study were connected to the CARESCAPE R860 (GE Healthcare) mechanical ventilator. Patients were curarised with rocuronium bromide (0,6 mg/kg) and sedated with midazolam (0,03-0,1 mg/kg/h) and remifentanil (0.1-1 mcg/kg/min) to eliminate spontaneous respiratory effort and provide sedation. Patients were ventilated in volume-controlled ventilation mode. A tidal volume of 6 ml/kg was applied according to the predicted body weight. Respiratory rate was adjusted to ensure normocarbia. End-expiratory positive pressure was reset. The end-inspiratory pause was set to 20%. Inspired oxygen concentration (FiO2) was adjusted so that oxygen saturation was above 92% in each patient. Inspiratory/ expiratory ratio was set to ½.
The ECOV-X (GE Healthcare) module was attached to the ventilator for gas measurements and allowed to warm up. A spirometry kit was inserted between the Y-piece in the ventilator circuit and the intubation tube or bacterial filter, if any.
An intratracheal pressure sensor was inserted to measure pressure levels independent of circuit and tube resistance and to evaluate them on the SpiroDynamics (GE Healthcare) application. Placement was made according to the marked area on the sensor and the sensor tip was aimed to be at the level of the carina.
After all connections were completed, VO2 and VCO2 of the patients were measured and they were expected to reach steady state within the last 30 minutes. In stabilised patients, the PEEP titration procedure called Lung INview (GE Healthcare) was initiated. An ascending PEEP trial was performed at four different PEEP levels determined as 0, 5, 10, and 15 cmH2O.
The lung was ventilated at each PEEP level for 10 minutes, during which FRC, EELV were measured with a modified multiple nitrogen flushing technique on the ventilator. The pressure-volume curve formed by the intratracheal pressure sensor at each PEEP level was analysed by SpiroDynamics application. The application generated a curve representing dynamic compliance during the analysis and determined the volume changes in this curve at each PEEP level. The difference between the EELV and the volume change in the pressure- volume curve was reflected as gain.
Static compliance was measured by performing an end- inspiratory pause at the end of each 10-minute step. Pulse rate, arterial blood pressure and peripheral oxygen saturation were monitored and recorded at each PEEP level. Tidal volume, peak pressure (Ppeak) and driver pressure were recorded at each step. Respiratory system elastance was calculated using an equation mentioned in the study of Henderson et al. [11] global and static strain was calculated using an equation in the study of Protti et al [12].
Statistical Analysis
When it was assumed that a strong effect size (d=0.8) would be obtained for the difference to be obtained between the two groups as a result of the power analysis performed hypothetically in the direction of expectations, it was calculated that at least 19 people should be included in the study in order to obtain 80% power with 95% confidence.
Data were analysed with IBM Statistics SPSS 25.0 package programme. Continuous variables were calculated by adding mean ± standard deviation, median, and minimum value- maximum value. Categorical variables were given as numbers and percentage. In dependent group comparisons, repeated measures analysis of variance was used when parametric test assumptions were met, and Friedman test was used when parametric test assumptions were not met. In addition, the relationships between continuous variables were analysed by Spearman or Pearson correlation analyses and the differences between categorical variables were analysed by Chi-square analysis.
Ethical Approval
This study was approved by the Ethics Committee of Pamukkale University, Faculty of Medicine (Date: 2019-10-24, No:18).
Results
A total of 20 patients, 11 males and 9 females, were included in the study.
There was no significant difference between the tidal volume, saturation, systolic and diastolic blood pressures of the patients during the PEEP trial. Pulse rate was significantly higher at 15 cmH2O PEEP level compared to 0 (p=0.007), 5 (p=0.002), and 10 cmH2O (p=0.013) PEEP levels.
The PEEP level with the highest static compliance was measured as 5 ± 3.62 cmH2O on average. The PEEP level with the lowest driver pressure was measured as 4.75 ± 3.43 cmH2O on average. The PEEP level with the lowest elastance was measured as 4.75 ± 3.79 cmH2O on average. The PEEP level with the highest total volume gain was measured as 11.75 ± 3.35 cmH2O on average. At each PEEP level, when the amount of gain compared to the previous PEEP level was evaluated, no significant difference was observed between the steps.
No statistically significant difference was found when the expected FRC value of the patients (2279 ± 452.05) was compared with the FRC values measured at 0 cmH2O PEEP (1991.5 ± 600.33). (p=0.191). The expected FRC was reached at a mean PEEP level of 4.06 ± 5.83 cmH2O.
The correlations of the analysed parameters with each other at different PEEP steps were evaluated. The correlation of the data with each other is shown in Table 3.
Discussion
Mechanical ventilator support is an essential part of treatment in intensive care units. Directing mechanical ventilator therapy on a wide range of patient populations in intensive care units depends on many parameters. While determining these parameters, it is necessary to avoid harmful effects and possible complications that may develop in patients. In our study, we evaluated the relationship between lung mechanics and each other in order to guide ventilation.
Bikker et al. [9] evaluated the effect of PEEP on EELV measurements in intensive care patients undergoing mechanical ventilation; EELV decreased significantly as the PEEP level decreased. Since we did not perform recruitment manoeuvre before the elevated PEEP trial in our study, we think that alveolar recruitment at high PEEP level may have contributed to both compliance and EELV. According to the baseline measurement, the amount of alveolar recruitment at PEEP levels of 10 and 15 cmH2O contributed to gain, compliance, and EELV, but we could not follow this in other steps.
Maisch et al. [14] showed significant correlation between PEEP increase and EELV in 20 anaesthetised patients. In the study, the optimal PEEP was found to be 10 cmH2O. In our study, the
optimal PEEP value was different according to compliance. In our study, the rising PEEP trial performed without recruitment may have resulted in lower compliance values. In our study, saturation and arterial blood pressure did not show a significant change similar to the study by Maisch et al. [14], pulse rate increased with increasing PEEP and this increase was statistically significant at the 15 cmH2O PEEP level compared to other PEEP levels. This may be explained by the fact that intensive care patients are more sensitive to the decrease in the preload of the heart with the increase in intrathoracic pressure and give a tachycardia response to maintain cardiac output.
In a PEEP trial in ARDS patients, Guo et al. [15] determined the PEEP values at which static compliance was best as 10 and 12 cmH2O. The fact that ARDS patients have lower compliance and FRC and need higher PEEP than our patient population to restore atelectatic alveoli to respiration may have led to higher PEEP results compared to our study.
Heinze et al. [16] showed that FRC and compliance values were moderately correlated after cardiac surgery. They showed that the correlation between FRC and compliance decreased when the measured FRC value of the patients exceeded the expected FRC value. In our study, while a significant decrease in compliance was observed at 15 cmH2O, this decrease was less in patients with higher FRC gain. This may be explained by the fact that high PEEP causes less distension in patients who gain more volume after opening of closed alveoli.
The optimal PEEP level according to minimum elastance of PEEP in ARDS patients was found to be 20.5 ± 7.97 cmH2O [17]. %85 of our patients reached the minimum elastance at PEEP levels of 0 and 5 cmH2O. The fact that our patients without lung pathology provided sufficient alveolar patency with lower PEEP caused lung distension in our patients at the high PEEP levels required by ARDS patients.
In our study, no significant correlation was found between volume gain changes and changes in compliance and EELV. According to the pressure-volume curve, compliance was found to be significantly lower at 15 cmH2O PEEP level, at which the volume change was the highest. This may be due to the difference in the amount of atelectatic and recoverable alveoli between the study populations. In addition, the volume gain in the pressure-volume curve exceeded the EELV in some patients in our study. This suggests that increases in the pressure-volume curve are not a sensitive marker of alveolar distension. In fact, in this case, the gain is also negatively affected. In line with our hypothesis, negative gain may indicate distension. When we evaluated respiratory mechanics, we found that EELV and strain were increased in patients with high PEEP (15 cmH2O), similar to the study of Dellamonica et al. This suggests that high PEEP levels increase alveolar strain in our patient population [18].
Patroniti et al. [19] reported that EELV increased as PEEP increased and neglecting EELV changes in pressure-volume curves may be misleading in calculating the amount of recruitment. The gain consists of the difference between EELV and volume change in the pressure-volume curve. Therefore, we may have determined the amount of recruitment more optimally. Similar to the study of Stahl et al. [20], there were volume increases in the pressure-volume curve at each PEEP level compared to the previous level, and this may not indicate lung strain or recruitment.
Recent studies emphasise that EELV measurement may be useful in mechanical ventilation strategies. Rollas et al. [21] provided better oxygenation and compliance with EELV- guided PEEP titration than PaO2-guided PEEP titration. They also showed that EELV can be used in prognosis and disease
severity monitoring [22] and tidal volume determination [23]. For this reason, we think that EELV monitoring is important.
Limitations
The use of muscle relaxants to perform measurements in patients may not have fully reflected the dynamic physiological state. Taking a single measurement from the patients and not continuing ventilation of the patients under the determined ideal PEEP conditions and not performing further evaluations were limiting in determining, complications, morbidity and mortality effects.
Conclusion
Volume gain was not correlated with compliance, elastance and driver pressure in a way to support our hypothesis. In conclusion; FRC-EELV, volume changes in pressure-volume curves and gain parameters do not seem to be sensitive to lung distension. Respiratory mechanics that increase with PEEP should be used together with lung distension-sensitive markers to guide ventilation for optimal PEEP selection.
Tables
Table 1. Demographic data

SD: Standard Deviation; Min, Maks: Maximum and minimum values
Table 2. Lung mechanics at different PEEP levels

PEEP: Positive End Expiratory Pressure EELV: End-Expiratory Lung Volume *: Significant according to 0 cmH2O PEEP, ⁻: Significant according to 5 cmH2O PEEP, ⌃: Significant according to 10 cmH2O PEEP, p<0.05 was accepted as significant.
Table 3. Correlation of respiratory mechanics in PEEP trial
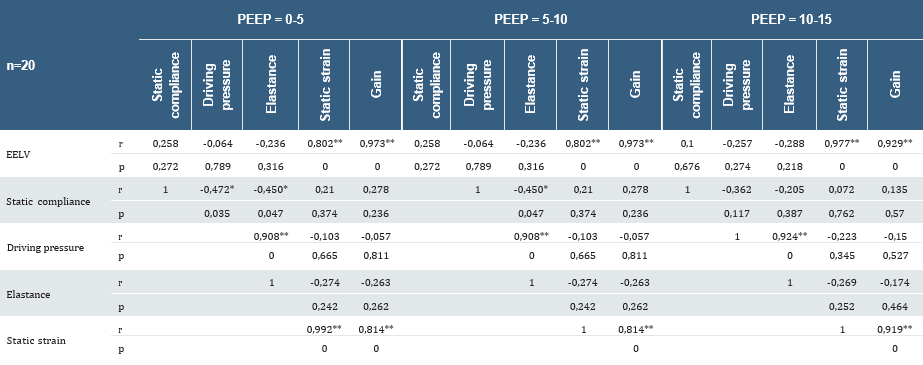
* Correlation is significant according p=0,05 ** Correlation is significant according p=0,01
References
-
Ware LB, Matthay MA. The acute respiratory distress syndrome. N Engl J Med. 2000;342(18):1334-1349.
-
Falke KJ, Pontoppidan H, Kumar A, Leith DE, Geffin B, Laver MB. Ventilation with end-expiratory pressure in acute lung disease. J Clin Invest. 1972;51(9):2315- 2323.
-
Sondergaard S, Kárason S, Wiklund J, Lundin S, Stenqvist O. Alveolar pressure monitoring: An evaluation in a lung model and in patients with acute lung injury. Intensive Care Med. 2003;29(6):955-962.
-
Suter PM, Fairley HB, Schlobohm RM. Shunt, lung volume and perfusion during short periods of ventilation with oxygen. Anesthesiology. 1975;43(6):617-627.
-
Casserly B, McCool FD, Saunders J, Selvakumar N, Levy MM. End-Expiratory Volume and Oxygenation: Targeting PEEP in ARDS Patients. Lung. 2016;194(1):35- 41.
-
Hedenstierna G. The recording of FRC--is it of importance and can it be made simple?. Intensive Care Med. 1993;19(7):365-366.
-
Olegård C, Söndergaard S, Houltz E, Lundin S, Stenqvist O. Estimation of functional residual capacity at the bedside using standard monitoring equipment: A modified nitrogen washout/washin technique requiring a small change of the inspired oxygen fraction. Anesth Analg. 2005;101(1):206-212.
-
Heinze H, Eichler W. Measurements of functional residual capacity during intensive care treatment: the technical aspects and its possible clinical applications. Acta Anaesthesiol Scand. 2009;53(9):1121-1130.
-
Bikker IG, van Bommel J, Reis Miranda D, Bakker J, Gommers D. End-expiratory lung volume during mechanical ventilation: A comparison with reference values and the effect of positive end-expiratory pressure in intensive care unit patients with different lung conditions. Crit Care. 2008;12(6): R145.
-
Gattinoni L, Pesenti A. The concept of “baby lung”. Intensive Care Med. 2005;31(6):776-784.
-
Henderson WR, Chen L, Amato MBP, Brochard LJ. Fifty Years of Research in ARDS. Respiratory Mechanics in Acute Respiratory Distress Syndrome. Am J Respir Crit Care Med. 2017;196(7):822-833.
-
Protti A, Andreis DT, Monti M, et al. Lung stress and strain during mechanical ventilation: Any difference between statics and dynamics?. Crit Care Med. 2013;41(4):1046-1055.
-
Villar J. The use of positive end-expiratory pressure in the management of the acute respiratory distress syndrome. Minerva Anestesiol. 2005;71(6):265-272.
-
Maisch S, Reissmann H, Fuellekrug B, Wismann D, Rutkowski T, Tusman G, et al. Compliance and dead space fraction indicate an optimal level of positive end-expiratory pressure after recruitment in anesthetized patients. Anesth Analg. 2008;106(1):175-181.
-
Fengmei G, Jin C, Songqiao L, Congshan Y, Yi Y. Dead space fraction changes during PEEP titration following lung recruitment in patients with ARDS. Respir Care. 2012;57(10):1578-1585.
-
Heinze H, Sedemund-Adib B, Heringlake M, Meier T, Eichler W. Relationship between functional residual capacity, respiratory compliance, and oxygenation in patients ventilated after cardiac surgery. Respir Care. 2010;55(5):589-594.
-
Chiew YS, Pretty CG, Shaw GM, et al. Feasibility of titrating PEEP to minimum elastance for mechanically ventilated patients. Pilot Feasibility Stud. 2015;1:9.
-
Dellamonica J, Lerolle N, Sargentini C, et al. PEEP-induced changes in lung volume in acute respiratory distress syndrome. Two methods to estimate alveolar recruitment. Intensive Care Med. 2011;37(10):1595-1604.
-
Patroniti N, Bellani G, Cortinovis B, et al. Role of absolute lung volume to assess alveolar recruitment in acute respiratory distress syndrome patients. Crit Care Med. 2010;38(5):1300-1307.
-
Stahl CA, Möller K, Schumann S, et al. Dynamic versus static respiratory mechanics in acute lung injury and acute respiratory distress syndrome. Crit Care Med. 2006;34(8):2090-2098.
-
Rollas K, Hanci P, Topeli A. Effects of end-expiratory lung volume versus PaO2 guided PEEP determination on respiratory mechanics and oxygenation in moderate to severe ARDS. Exp Lung Res. 2022;48(1):12-22.
-
Hao S, Wei Y, Wang Y, et al. End-expiratory lung volumes as a potential indicator for COVID-19 associated acute respiratory distress syndrome: A retrospective study. BMC Pulm Med. 2024;24(1):298.
-
Grassi A, Teggia-Droghi M, Borgo A, Szudrinsky K, Bellani G. Feasibility of Setting the Tidal Volume Based on End-Expiratory Lung Volume: A Pilot Clinical Study 2024;6(1):e1031.
Declarations
Scientific Responsibility Statement
The authors declare that they are responsible for the article’s scientific content including study design, data collection, analysis and interpretation, writing, some of the main line, or all of the preparation and scientific review of the contents and approval of the final version of the article.
Animal and Human Rights Statement
All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Funding
None
Conflict of Interest
The authors declare that there is no conflict of interest.
Ethics Declarations
This study was approved by the Ethics Committee of Pamukkale University (Date: 2019-10-24, No: 18)
Data Availability
The data supporting the findings of this article are available from the corresponding author upon reasonable request, due to privacy and ethical restrictions. The corresponding author has committed to share the de-identified data with qualified researchers after confirmation of the necessary ethical or institutional approvals. Requests for data access should be directed to bmp.eqco@gmail.com
Additional Information
Publisher’s Note
Bayrakol MP remains neutral with regard to jurisdictional and institutional claims.
Rights and Permissions
About This Article
How to Cite This Article
Anıl Kuvandık, Selvinaz Yüksel Tanrıverdi, Fatih Sargın, Hülya Sungurtekin. Evaluation of end-expiratory lung volume, gain and pulmonary mechanics with PEEP titration in mechanical ventilation of intensive care unit patients. Ann Clin Anal Med 2025; DOI: 10.4328/ACAM.22470
Publication History
- Received:
- October 29, 2024
- Accepted:
- March 19, 2025
- Published Online:
- April 23, 2025
- Printed:
- November 1, 2025

