Evaluation of respiratory tract multiplex PCR results in pediatric intensive care unit
Evaluation of respiratory multiplex PCR
Authors
Abstract
Aim Acute respiratory tract infections continue to be among the leading causes of morbidity and mortality in pediatric patients. Early identification of respiratory infections and detection of the causative pathogen are crucial for accurate diagnosis and effective treatment.
Our study aims to evaluate the multiplex PCR results of pediatric patients admitted to the intensive care unit, determine the prevalence of respiratory pathogens, and investigate their association with clinical outcomes.
Materials and Methods The study was conducted retrospectively on pediatric patients aged 1 month to 18 years who were admitted to the PICU and underwent respiratory multiplex PCR testing between April 15, 2021, and April 15, 2023.
Results The study included a total of 160 patients, 53.1% of whom were female. A viral pathogen was detected in 79 patients (49.4%), a bacterial pathogen in 39 patients (24.4%), while no pathogen was identified in 26.2% of cases. The most frequently detected bacterial pathogen was Haemophilus influenzae in 33 patients (20.6%), followed by Streptococcus pneumoniae in 15 patients (9.4%). The most common viral pathogen was Rhinovirus/Enterovirus, detected in 18 patients (11.2%), followed by RSV at 10% prevalence. Patients with positive PCR results had higher ALT, AST, and lactate levels.
Discussion The respiratory multiplex PCR panel, with its rapid diagnostic capability, can help reduce unnecessary antibiotic use in critically ill pediatric patients, thereby minimizing antimicrobial resistance development.
Keywords
Introduction
Lower respiratory tract infections (LRTIs) represent a significant health concern in children, affecting the bronchi and alveoli. These infections continue to contribute to high morbidity and mortality rates in the pediatric population.
Acute respiratory infections characteristically initiate in the upper respiratory tract, as the entry point for pathogens is via the nose, mouth, or eyes. These infections typically require two to four days to disseminate to the lower parts of the airways. The manifestations of these infections are often analogous, with symptoms including fever, cough, and malaise [1].
The diversity of organisms causing ASRI in children and the delay in diagnosis (approximately 30%) have been shown to affect the treatment process. The majority of patients admitted to pediatric intensive care units (PICU) are still diagnosed with ASRI. Co-infections have been detected in approximately 26– 35% of hospitalized children with pneumonia, and this condition is thought to increase the severity of infection [2].
Accurate identification of respiratory pathogens is crucial for the clinical diagnosis, treatment, and epidemiological surveillance of ASRIs. PCR is widely used for molecular detection, and innovative multiplex PCR methods, which can identify multiple pathogens simultaneously, have significantly improved the efficiency of respiratory pathogen detection [3]. Multiplex RT-PCR assays are widely used tools for detecting and differentiating a range of respiratory viral pathogens [4]. Quantitative multiplex-PCR testing of respiratory secretions in, the respiratory tract is a highly sensitive method for the diagnosis of viral infections. With this test, viral pathogens as well as atypical bacterial pathogens can be confirmed [5]. These techniques the classical methods of virus isolation or direct fluorescent antibody (DFA) tests offer higher sensitivity. It is also shorter time and provides specific results for a larger number of pathogens. Recently a study showed that multiplex PCR methods can detect up to 16 pathogens in a single test. Simultaneously detect and differentiate lower respiratory tract infections [6]. Inadequate etiologic diagnosis of lower respiratory tract infections, unnecessary and inappropriate use of antibiotics, and widening hospital stays, hospital can lead to increased costs and antibiotic resistance. Viral rapid depletion of viruses, early diagnosis, and clinical use by pediatricians are extremely important for decision-making [7]. In this study, we analyzed the multiplex respiratory PCR results of pediatric patients admitted to the PICU. We aimed to identify the etiological agents responsible for ASRI in children and to demonstrate their demographic and clinical characteristics. By presenting the detected pathogens through multiplex respiratory PCR, we aimed to increase awareness in this field.
Materials and Methods
The study was conducted retrospectively on pediatric patients aged 1 month to 18 years who were admitted to the PICU and underwent respiratory multiplex PCR testing between April 15, 2021, and April 15, 2023. Patient data were retrieved from the hospital information system. The recorded variables included age, gender, reasons for admission, symptoms, clinical findings, laboratory parameters, respiratory support interventions, and prognosis.
Nasopharyngeal samples were collected and transported to the laboratory for analysis (Seeplex® RV15 ACE, Seegene, South Korea). The test was performed according to the manufacturer’s protocol.
Data analysis was conducted using IBM SPSS Statistics 25 © Copyright SPSS Inc. 1989, 2017. The normality of distribution for continuous variables was assessed using the Kolmogorov- Smirnov test. Categorical variables were presented as frequency (n) and percentage (%), while continuous variables were expressed as mean ± standard deviation (SD), median (IQR 25-75), and minimum-maximum values.
For independent two-group comparisons, the Mann-Whitney U test was applied due to non-normal distribution of data. The Kruskal-Wallis H test was used for comparisons of more than two independent groups, and post-hoc Bonferroni correction was performed based on the Kruskal-Wallis H test results.
For categorical variable analyses, Pearson’s Chi-Square test, Fisher’s Exact test, Fisher-Freeman-Halton Exact test, Yates’ correction, and post-hoc Bonferroni correction were applied. Statistical significance was set at p < 0.05.
Ethical Approval
This study was approved by the Ethics Committee Ümraniye Training and Research Hospital (Date: 2023-06-20, No: 218500688).
Results
The study included a total of 160 patients, of whom 53.1% were female. The mean age of the patients was 6.66 ± 5.26 years. Among them, 152 (95%) had received routine vaccinations and 94 (58.8%) had comorbid conditions. PCR results were positive in 96 (60%) patients. The demographic characteristics of the patients are summarized in Table 1.
A viral pathogen was detected in 79 (49.4%) patients, while bacterial pathogens were identified in 39 (24.4%) patients; in 26.2% of cases, no pathogen was detected. The most frequently detected bacterial pathogen was Haemophilus influenzae, found in 33 (20.6%) patients, followed by Streptococcus pneumoniae in 15 (9.4%) patients.
The most commonly detected viral pathogen was Rhinovirus/ Enterovirus, found in 18 (11.2%) patients, followed by RSV at a frequency of 10%. The distribution of pathogens identified through respiratory multiplex PCR is presented in Table 2.
The most common reason for PICU admission was respiratory distress (47.5%), followed by convulsions (15%) and postoperative monitoring (13.8%). A significant association was observed between younger age and higher PCR positivity rates (Figure 1).
Among the patients, 68% exhibited single pathogen growth, 24.7% had dual pathogen growth, and 7.2% had three or more pathogens detected.
The most frequently observed symptoms were fever (81.1%), cough (58.6%), nasal discharge (41.3%), vomiting (17.5%), diarrhea (11.3%), and rash (7.5%), in descending order of prevalence. The laboratory parameters of PCR-positive and PCR-negative patient groups were compared. ALT, AST, creatinine, and lactate levels were significantly higher in PCR- positive patients than in PCR-negative patients (p = 0.030, p = 0.002, p = 0.032, and p = 0.045, respectively). However, neutrophil counts were significantly lower in PCR-positive patients (p = 0.024).
A total of 67 patients (41.9%) required mechanical ventilation for respiratory support. The types of respiratory support were compared between PCR-positive and PCR-negative patient groups.
Patients with spontaneous breathing who did not receive oxygen therapy or other forms of respiratory support had a significantly higher PCR negativity rate compared to those receiving respiratory support (p = 0.023, ) However, no significant differences were found between groups receiving oxygen via mask, invasive mechanical ventilation (IMV), and non-invasive ventilation (NIV).
There were no statistically significant differences between the types of respiratory support and the number of pathogens detected (single, dual, or triple growth) or the type of pathogens identified (viral vs. bacterial) (p > 0.05).
A chest X-ray was performed on all patients for whom a respiratory panel was requested. The rate of pulmonary infiltration was significantly higher in PCR-positive patients compared to PCR-negative patients (p < 0.001). However, there was no significant difference between the groups in terms of pleural effusion and pneumothorax incidence.
Antibacterial treatment was administered to 97.5% of the patients, while 21.9% received antiviral therapy. No significant difference was found between PCR-positive and PCR-negative patient groups in terms of antiviral and antibacterial treatment administration (p > 0.05). Similarly, there was no significant difference between the groups in terms of seasonal distribution (p = 0.548, p > 0.05).
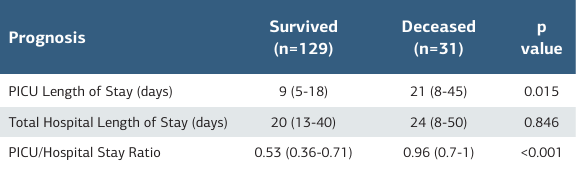
A total of 31 patients (19.4%) died, and no significant difference Table 1. Demographic characteristics of the patients in mortality rates was observed between the patient groups (p = 0.111). However, the length of PICU stay was significantly longer in deceased patients compared to survivors (Table 3).
Discussion
Acute respiratory tract infections are a major cause of morbidity and mortality in childhood. Identifying the causative agents of these infections and implementing appropriate interventions are crucial. These infections predominantly affect children aged 0–5 years, with viral pathogens being the most common causative agents. Additionally, co-infections involving viral- viral or viral-bacterial agents can also occur. The widespread adoption of multiplex PCR, a diagnostic method with high sensitivity and reliability for respiratory infections, has the potential to facilitate rapid diagnosis and treatment, thereby improving patient prognosis.
A study conducted in a pediatric intensive care unit (PICU) in India reported that 85% of patients with positive respiratory PCR test results had viral pathogens [8] Similarly, in our study, viral pathogen positivity was detected in 81.3% of cases. In recent years, the misuse of antibiotics and the emergence of antimicrobial resistance have become growing concerns. We believe that the increasing use of PCR can help reduce unnecessary and widespread antibiotic use.
Appak et al. reported that rhinovirus/enterovirus and respiratory syncytial virus (RSV) were the most commonly detected pathogens in pediatric patients [9] Similarly, a 2023 study found that the most prevalent pathogens were rhinovirus/ enterovirus (31.6%), RSV (18.8%), and adenovirus (15%) [10]. In our study, the most frequently detected viruses, consistent with the literature, were rhinovirus/enterovirus (18.8%) and RSV (16.7%).
Results may vary based on the studied age group and clinical setting. Akkoç et al. found that RSV was the most common pathogen in children aged ≤5 years, followed by rhinovirus [11]. The higher incidence of RSV in this age group is well established. We believe that the differing results in our study may be due to the inclusion of critically ill patients and a broader age range. A 2022 study reported that PCR positivity was most frequently observed in children aged 2–4 years [12]. Consistently, our study found that PCR positivity was most common in children aged 0–5 years (p = 0.022).
Lower respiratory tract infections often lead to respiratory distress, necessitating oxygen therapy, invasive mechanical ventilation (IMV), or non-invasive ventilation (NIV) in some cases. In our study, the PCR negativity rate was 28.1% in patients who did not require respiratory support, whereas it decreased to 12.5% in PCR-positive patients (p = 0.02). Similarly, respiratory distress was more frequently observed in PCR-positive patients (p = 0.03).
These findings suggest that multiplex respiratory PCR testing should be performed in critically ill patients with respiratory distress, facilitating the early identification of pathogens. This approach may improve patient outcomes by enabling early targeted treatments and timely respiratory support.
Several studies have investigated the impact of co-infections on clinical outcomes. A study conducted in Italy found that viral co-infections were not a risk factor for mechanical ventilation, whereas viral-bacterial co-infections were significantly associated with mechanical ventilation requirement (p < 0.001) [13].
Similarly, in a study by Chien-Yu Lin et al., approximately one- quarter of patients were co-infected with two or more viruses, but no significant differences were found between single- pathogen infections and co-infections in terms of clinical or laboratory findings [14].
In our study, patients with spontaneous breathing who did not require oxygen or other respiratory support had a significantly higher PCR negativity rate compared to those who required respiratory support (p = 0.023). However, there was no significant difference among patients receiving oxygen via mask, IMV, or NIV. Additionally, there was no statistically significant difference between the type of respiratory support and the number of pathogens detected (single, dual, or triple) or the type of pathogens (viral vs. bacterial).
Radiographic findings play a crucial role in the diagnosis and management of viral and bacterial respiratory infections. Javier et al. (2021) reported that patients with PCR positivity had a higher prevalence of lung infiltration on chest X-rays [15]. Similarly, in our study, pulmonary infiltration was significantly more frequent in PCR-positive patients compared to PCR- negative patients (p < 0.001). However, no significant difference was observed between the groups regarding pleural effusion or pneumothorax incidence.
Limitations
A retrospective study, with its inherent limitations on the number of subjects and the range of situations that can be assessed, was the basis of our investigation. Notably, this retrospective study was conducted in pediatric intensive care units.
The evaluation of multiplex PCR results in inpatients revealed the prevalence and clinical impact of co-infections and various causative agents on clinical outcomes.
The findings of this study suggest a substantial impact of co- infections and various causative agents on clinical outcomes. The results are indicative of the need for further research in this field. The interaction of viral and bacterial agents, as well as the implications of seasonal changes on disease management, are of particular importance for clinical practice.
The results of the study have revealed significant findings.
Conclusion
Multiplex respiratory PCR panels, by providing rapid diagnostic results, may help prevent unnecessary antibiotic use in critically ill pediatric patients, thereby reducing the risk of antimicrobial resistance. Furthermore, by enabling targeted therapy, they may contribute to improving clinical outcomes. However, their use in critically ill pediatric patients should consider limitations such as cost and accessibility.
Tables
Table 1. Demographic characteristics of the patients
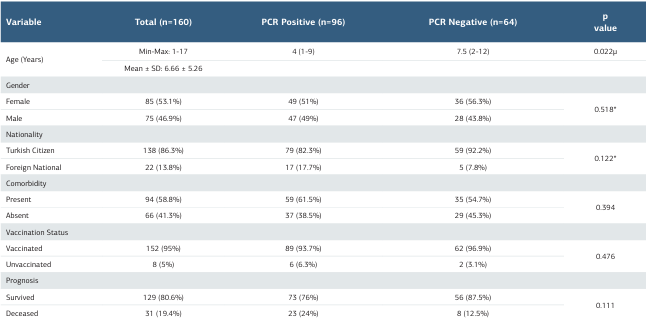
Table 2. Pathogens detected by respiratory multiplex PCR
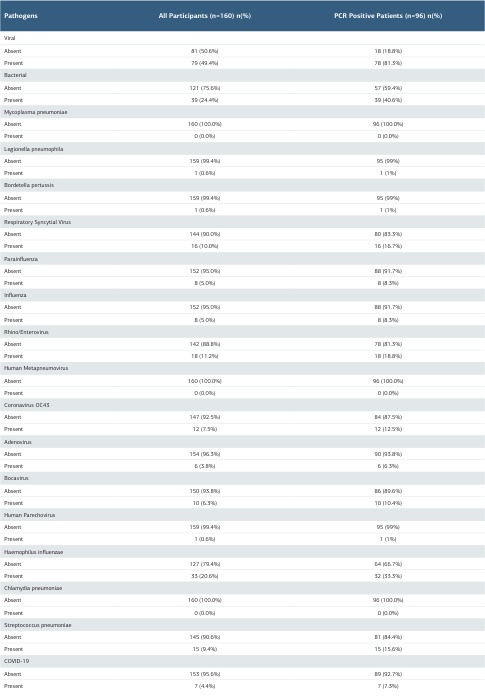
Table 3. Comparison of length of hospital stay based on patient prognosis
References
-
van Doorn HR, Yu H. Viral respiratory infections. In: Ryan ET, Hill DR, Solomon T, Aronson NE, Endy TP, eds. Hunter’s Tropical Medicine and Emerging Infectious Diseases. 10th ed. Edinburgh: Elsevier; 2020:284–8. doi:10.1016/B978-0-323-55512-8.00033-8.
-
Sarfo JO, Amoadu M, Gyan TB, et al. Acute lower respiratory infections among children under five in Sub-Saharan Africa: a scoping review of prevalence and risk factors. BMC Pediatr. 2023;23(1):225. doi:10.1186/s12887-023-04033-x.
-
Chen X, Wang F, Fu Y, et al. Development and evaluation of a multiplex digital PCR method for sensitive and accurate detection of respiratory pathogens in children. Virology. 2024;590:109948. doi:10.1016/j.virol.2023.109948.
-
Deng J, Ma Z, Huang W, et al. Respiratory virus multiplex RT-PCR assay sensitivities and influence factors in hospitalized children with lower respiratory tract infections. Virol Sin. 2013;28(2):97-102. doi:10.1007/s12250-013-3312-y.
-
Krause JC, Panning M, Hengel H, Henneke P. The role of multiplex PCR in respiratory tract infections in children. Dtsch Arztebl Int. 2014;111(38):639-45. doi:10.3238/arztebl.2014.0639.
-
Bierbaum S, Forster J, Berner R, et al; CAPNETZ study group. Detection of respiratory viruses using a multiplex real-time PCR assay in Germany, 2009/10. Arch Virol. 2014;159(4):669-76. doi:10.1007/s00705-013-1876-3.
-
Aktürk H, Sütçü M, Badur S, Törün SH, et al. Evaluation of epidemiological and clinical features of influenza and other respiratory viruses. Turk Pediatri Ars. 2015;50(4):217-25. doi:10.5152/TurkPediatriArs.
-
Barchha S, Shobhavat L, Solomon R, Harnal S. Etiology of acute respiratory infections using multiplex polymerase chain reaction in children admitted to pediatric intensive care unit: a single-centered retrospective observational study from Western India. J Pediatr Crit Care. 2023;10(6):257-61. doi:10.4103/jpcc. jpcc_61_23.
-
Appak Ö, Duman M, Belet N, Sayiner AA. Viral respiratory infections diagnosed by multiplex polymerase chain reaction in pediatric patients. J Med Virol. 2019;91(5):731-7. doi:10.1002/jmv.25379.
-
Tiew WT, Chen YC, Hsiao HL, Chen CL, Chen CJ, Chiu CH. Impact of multiplex polymerase chain reaction syndromic panel on antibiotic use among hospitalized children with respiratory tract illness during COVID-19 pandemic. J Microbiol Immunol Infect. 2023;56(4):688-94. doi:10.1016/j.jmii.2023.01.009.
-
Akkoc G, Dogan C, Bayraktar S, Sahin K, Elevli M. Evaluation of viral respiratory pathogens in children aged under five hospitalized with lower respiratory tract infections. North Clin Istanb. 2022;9(2):162-172. doi:10.14744/nci.2021.69923.
-
Chiu YT, Tien N, Lin HC, et al. Detection of respiratory pathogens by application of multiplex PCR panel during early period of COVID-19 pandemic in a tertiary hospital in Central Taiwan. J Microbiol Immunol Infect. 2022;55(6 Pt 2):1144-50. doi:10.1016/j.jmii.2021.09.011.
-
De Luca M, D’Amore C, Romani L, et al. Severe viral respiratory infections in the pre-COVID era: A 5-year experience in two pediatric intensive care units in Italy. Influenza Other Respir Viruses. 2023;17(1):e13038. doi:10.1111/irv.13038.
-
Lin CY, Hwang D, Chiu NC, et al. Increased detection of viruses in children with respiratory tract infection using PCR. Int J Environ Res Public Health. 2020;17(2):564. doi:10.3390/ijerph17020564.
-
Javier KB, Navoa-Ng JA, Cotoco-Chu N. Rapid detection of respiratory pathogens using a multiplex PCR assay among hospitalized children with acute respiratory infection. PIDSP J. 2021;22(2):55-65. doi:10.56964/pidspj20212202008.
Declarations
Scientific Responsibility Statement
The authors declare that they are responsible for the article’s scientific content, including study design, data collection, analysis and interpretation, writing, and some of the main line, or all of the preparation and scientific review of the contents, and approval of the final version of the article.
Animal and Human Rights Statement
All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Funding
None
Conflict of Interest
The authors declare that there is no conflict of interest.
Ethics Declarations
This study was approved by the Ethics Committee of Ümraniye Training and Research Hospital (Date: 2023-06-20, No: 218500688)
Data Availability
The datasets used and/or analyzed during the current study are not publicly available due to patient privacy reasons but are available from the corresponding author on reasonable request.
Additional Information
Publisher’s Note
Bayrakol MP remains neutral with regard to jurisdictional and institutional claims.
Rights and Permissions
About This Article
How to Cite This Article
Mehmet Fatih Aybar, Gürkan Atay, Hazal Ceren Tugrul, Ceren Bilgün, Seher Erdoğan. Evaluation of respiratory tract multiplex PCR results in pediatric intensive care unit. Ann Clin Anal Med 2026;17(1):10-15
Publication History
- Received:
- March 4, 2025
- Accepted:
- May 5, 2025
- Published Online:
- May 26, 2025
- Printed:
- January 1, 2026

