Anesthetic experiences in recurrent electroconvulsive therapy applications in geriatric patients
Anesthetic experiences in electroconvulsive therapy
Authors
Abstract
Aim Depression is observed in 1-5% of geriatric patients. Electroconvulsive therapy (ECT) is preferred in severely depressed patients who do not respond to psychopharmacologic treatments and in whom an immediate therapeutic effect is expected. We aimed to compare the effects of succinylcholine and rocuronium-sugammadex on seizure duration, side effects, recovery, and geriatric depression score in geriatric patients undergoing ECT.
Materials and Methods The study was single-center and retrospective. Thirteen patients over 65 years of age and ASA 1-3 were included. Those who received Sch 0.5 mg/kg IV. as a neuromuscular blocker were named Group S, and those who received rocuronium 0.4 mg/kg IV. were named Group R. Demographic data, duration of hospitalization, duration of EEG and motor seizures, current intensity, side effects, Modified Aldrete Score, Geriatric Depression Score (GDS) values were recorded.
Results The mean age was 65.8 ± 0.75 years; 7 were female (53.8%), and six were male (46.2%). There was no statistical difference in seizure duration, flow dose, and recovery time between the two groups. Muscle pain was statistically more common in Group S (p=0.016). The GDS values after ECT decreased significantly in both groups compared to after ECT (p<0.05), but no difference was observed between the groups.
Discussion In geriatric patients undergoing repeated ECT, Sch and rocuronium showed similar seizure efficacy and recovery characteristics, although the incidence of side effects was different. Geriatric Depression Scores decreased after ECT, and both agents produced similar therapeutic efficacy. Rocuronium- sugammadex can be used as an effective alternative to Sch in geriatric patients.
Keywords
Introduction
Although basic personality traits do not change much over time, the decline in physical skills and cognitive functions, decrease in daily activities, weakening in social relations, deterioration in income, feeling of loneliness, and fear of death trigger depression with advancing age. According to the World Health Organization, depression is a common mental disorder with a prevalence of 5-25% in adults. In our country, this rate varies between 10.2% and 61% [1]. While oral antidepressants are considered to be the most effective pharmacologic agent in the treatment of depression, electroconvulsive therapy (ECT) is preferred in cases of severe depression that don’t respond to psychopharmacological treatments and where immediate therapeutic efficacy is expected [2]. ECT is based on inducing therapeutic convulsions with variable frequency electrical stimulation of the brain through electrodes. ECT has been used with anesthetic agents and muscle relaxants since the 1960s because of fear of the procedure, dramatic seizure appearance after electrical stimulation, and unwanted bone and tooth fractures [3].
The duration and quality of the epileptic seizure induced in ECT procedures are the main factors determining the efficacy, and the drugs used during the procedure affect this duration. Agents that have a rapid onset of action, short recovery time, no residual effect, and produce effective seizures are preferred for the formation of an effective biological response [4]. Succinylcholine (Sch) is a short-acting depolarizing muscle relaxant metabolized by plasma cholinesterase. It produces unsynchronized muscle fasciculation before producing paralysis. Its contraindications include narrow-angle glaucoma and hyperkalemia, prolonged effect in patients using lithium, risk of malignant hyperthermia, and restricted use in pseudocholinesterase enzyme deficiency, leading to the preference for non-depolarizing muscle relaxants in ECT anesthesia [5]. After encountering difficulties in the procurement of Sch in our country, the use of rocuronium- sugammadex as an alternative has begun, and heterogeneous studies have been published on its use. The aim of this study was to compare the effect of Sch and rocuronium-sugammadex on seizure duration, side effects, recovery, and geriatric depression scores in elderly patients undergoing ECT.
Materials and Methods
Thirteen patients (n = 13) who were diagnosed with major depression according to DSM-IV and underwent ECT, whose preanesthetic consents were obtained with verbal information, and who were over 65 years of age and in the ASA 1-3 risk group were included in the study. Patients were divided into two groups: Group R (n=8), undergoing a total of 88 ECT sessions and Group S (n=5) undergoing a total of 55 ECT sessions. Each patient received a total of 9 ECT repetitions 3 times a week. Exclusion criteria: Patients with cardiovascular, respiratory, cerebrovascular, and neuromuscular diseases, comorbid conditions such as renal and hepatic organ failure, antiepileptic therapy that may affect seizure duration, allergies, morbid obesity, patients with seizure duration less than 20 s, and patients who underwent repeated ECT with high-intensity restimulation were excluded from the study.
Patients were evaluated in two groups: patients receiving 0.7 mg/kg of IV propofol as a hypnotic and those receiving 0.5 mg/kg of IV Sch as a neuromuscular blocker (Group S). Patients who received rocuronium at a dose of 0.4 mg/kg IV as a neuromuscular blocking agent and sugammadex at a dose of 4 mg/kg IV as a reversal agent were assigned to group R. The patients in group S were ventilated until the fasciculations disappeared, while the patients in group R were ventilated for 90 seconds after the administration of rocuronium. A rolling sponge was then placed in the mouth, and electrical stimulation was administered. As in our routine practice, the isolated arm technique was applied by placing a cuff on the left arm and inflating it before the neuromuscular blocker was administered by placing a cuff on the left arm after the vascular access from the dorsum of the right hand or the antecubital region for anesthetic induction. Manual ventilation was performed with an appropriate face mask using 100% oxygen via a semi-closed equipped circuit with EtCO2 in the range of 25-40 mmHg. Patient demographics, previous ECT procedures, length of hospital stay, duration of motor ECT seizures, duration of EEG seizures, current intensity, side effects, Modified Aldrete Score (MAS), and GDS scores were recorded. In our routine practice, drugs that influence the duration and quality of seizures are discontinued 24 hours before ECT. In anesthesia, propofol was used as a hypnotic, Sch was used as a neuromuscular blocker in the period when there were no supply shortages in Turkiye, rocuronium was used later, and sugammadex was used as a reverser. In the psychiatric clinic of our hospital, ECT is performed under anesthesia using the Thymatron System IV 4, a bipolar ECT device (Somatics LLC. Lake Bluff, IL, USA) capable of delivering 70-130 volts of alternating current with bi-frontotemporal electrodes. Seizure duration was measured with the ECT device, and EEG activity and monitoring were recorded by a psychiatrist.
EEG seizure duration, motor seizure duration, current dose, and whether seizures were inadequate were determined from psychiatric records. Those who had medical intervention for bradycardia, tachycardia, arrhythmia, headache, myalgia, nausea/vomiting, delirium, and post-ECT agitation were recorded as adverse events. In determining cognitive function, duration of recovery, orientation time, MAS 12, and GDS scores were evaluated.
Statistical Analysis
For the analysis of the study, the data were uploaded to the SPSS (IBM, SPSS Statistics version 27) program, and descriptive statistics were determined for each variable. Compliance of quantitative measurements with normal distribution was evaluated by the Shapiro-Wilk test. A comparison of quantitative measurements that did not conform to normal distribution between two independent groups was performed with the Mann-Whitney U test. A comparison of qualitative variables between two independent groups was performed with the Pearson Chi-Square test. While a paired sample t-test was used for the comparison of repetitive values within the group, a Student t-test was used for the comparison of values before and after ECT application between the groups. Descriptive statistics of the study were presented as mean± standard deviation for quantitative variables and median (minimum-maximum) when necessary and as number and percentage (n(%)) for qualitative variables. The significance level (p) was accepted as 0.05.
Ethical Approval
This study was approved by the Ethics Committee of Fırat University (Date: 2023-06-11, No: 15880).
Results
The mean age of the patients was 65.8 ± 0.75 years (65-67); 7 were female (53.8%) and six were male (46.2%). Gender, age, BMI, and ASA values of the patients according to the groups are similar. No statistically significant difference was observed in the demographic data of both groups (p > 0.05). According to the distribution of the patients according to their diagnoses before ECT, 23.07% (n = 3) had monopolar depression, 38.46% (n = 5) had bipolar depression, 30.76% (n = 4) had schizoaffective depression, and 7.69% (n = 1) had catatonia.
When the two groups were compared in terms of seizure duration, current dose, clinical efficacy, and recovery time, no statistical difference was observed (Table 1).
As a side effect, muscle pain was statistically more common in Group S (p = 0.016) (Table 2). Geriatric depression scores of the patients before and after ECT decreased significantly in both groups (p < 0.05), and a good clinical response was observed. No significant difference was found between the groups (Table 3).
Discussion
Patients resistant to medical treatment and poorly responsive to psychotherapy exhibit a 55% response rate to ECT, especially when there is an acute exacerbation of psychotic symptoms or if catatonic symptoms are prominent. This rate has been reported to reach 90% in patients with depression. Despite its short-term efficacy and the need for repeated sessions, ECT is generally considered more therapeutic than pharmacotherapy, particularly in depression patients [6]. Antidepressants combined with ECT are associated with a high response rate and safety for treating depression, regardless of age [7]. As ECT applications have become widespread, studies comparing the anesthetic agents used have been conducted, but we did not find a similar study in geriatric patients in the literature. In this study, we aimed to contribute to the literature by comparing the seizure duration, applied current dose, side effects, clinical efficacy (GDS), and effects on recovery (MAS) of Esmeron-Sugammadex compared to Sch in geriatric repeated ECT applications. In conclusion, there was no statistical difference between the seizure duration, current dose, clinical efficacy, and recovery time of the two muscle relaxants with different mechanisms of action. As a side effect, muscle pain was statistically more common in Group S (p = 0.016). Geriatric depression scores of the patients after ECT decreased significantly in both groups compared to before ECT, and a good clinical response was observed. No significant difference was found between the groups. Rocuronium may be preferred as an alternative in geriatric patients with similar efficacy to Sch.
ECT recommended therapeutic seizure duration is at least 25 seconds, and care should be taken that anesthetics do not affect this duration. The patient should be given the lowest electric current that produces convulsions at the neuronal level [8]. Compared to those receiving pharmacological treatments, geriatric patients constitute an especially high proportion of those who receive ECT [9]. The seizure threshold is higher in geriatric patients; therefore, higher current stimulation is needed to induce convulsions with ECT [10]. In our study, no statistically significant difference was found when current dose values were compared between the groups (Group S 76.88 ± 9.22 and Group R 80.41±9.99) (p = 0.132).
For a successful ECT procedure, convulsions must be induced in sufficient time. The duration of convulsion determines the effectiveness of the procedure, and the anesthetics used affect this duration. In geriatric patients, seizure duration may shorten with age, and the need for more ECT may occur [11]. In the study by Türkkal et al., 13 patients were included, and ECT was applied 3 times a week. Motor seizure duration and time to spontaneous breathing were compared in two groups using rocuronium and Sch. Seizure duration and time to spontaneous respiration were longer in the rocuronium group, and no difference was found between the two groups in tests of eye-opening and tongue protrusion [12]. Nishiyama et al., a total of 40 ECT applications in 10 patients were divided into four groups. These groups were group TS: thiopental and suxamethonium, group PS: propofol and suxamethonium, group TV: thiopental and vecuronium, and group PV: propofol and vecuronium. There was no difference in hemodynamic measurements between the four groups. When comparing seizure duration, no significant difference was found between thiopental and propofol, but vecuronium was found to shorten seizure duration compared with suxamethonium [13]. Köksal et al. compared rocuronium-sugammadex (group R) and Sch (group S) in the ECT procedure in terms of recovery and side effects and found that motor seizure duration was significantly longer (p = 0.002), and MAS values were significantly lower (p = 0.047) in group R [14]. In our study, EEG seizure duration (p = 0.844), motor seizure duration (p = 0.454), and duration of MAS 12 (pv= 0.949) were similar between the two groups.
Succinylcholine is the most commonly used depolarizing muscle relaxant, but it has side effects (increased intraocular and intragastric pressure, hyperkalemia), contraindications (pseudocholinesterase enzyme deficiency), and potential risks (neuroleptic malignant syndrome, malignant hyperthermia). Rocuronium is increasingly used in ECT practice today. Rocuronium has been shown to provide adequate neuromuscular blockade when used at appropriate doses in various studies [15]. The absence of cardiovascular side effects with sugammadex, a new generation gamma-cyclodextrin derivative used to terminate its effect, is a very important advantage [16]. One of the most common side effects following ECT administration is headache, and its etiology is not fully understood. Especially after the use of succinylcholine, muscle fasciculations, masseter muscle spasm, and serotonergic neurotransmission in the brain are suggested to trigger headaches On average, it occurs as high as 48-85% and sometimes lasting 2-3 days [17]. We determined that the most common side effect in Group S was headache 27.5% (n = 19) and tachycardia 29% (n = 9) in Group R. The most common side effect in Group S was myalgia 14.5% and postoperative confusion 21.1% in Group R. When the groups were compared, muscle pain was statistically more common in Group S (p = 0.016) (p < 0.05).
The MAS is a widely used scoring system to determine patient readiness for transfer from the recovery room to the ward. When the score reaches 12 points, patients can be transferred from the recovery room to the ward. The postoperative recovery time and MAS 12 were statistically similar between the groups. Oflazer et al., 134 ECT patients compared the seizure variables and clinical outcomes of using rocuronium-sugammadex as a neuromuscular blocker instead of Sch with propofol anesthesia in the first session and showed similar results [18]. Takazawa et al. reported that the recovery time from muscle relaxation after Sch administration was significantly longer than that after rocuronium-sugammadex administration [19]. Sağır et al. reported that it would be more appropriate to use MAS, TOF, and other positive clinical tests together when evaluating recovery from neuromuscular blockade [20]. Kadoi et al. [21] showed that there was no significant difference in the reversal of neuromuscular blockade with 0.6 mg kg -1 rocuronium using different doses of sugammadex (4, 8, and 16 mg kg -1).
The GDS used in our study is a self-report, easy-to-administer scale consisting of 15 easy-to-answer questions for older people, the validity and reliability of which have been established in our country [22]. In determining the scale score, 0-4 reflects that there is no depression, 5-8 reflects mild depression, 9-11 reflects moderate depression, and 12-15 reflects that the individual is severely depressed. Şahin et al. investigated the effect of ECT on oxidative metabolism in major depression. When the Hamilton Depression Rating Scale (HDRS) scores were compared before and after ECT, a significant decrease was observed after ECT. The mean score of the DRS was calculated as 28.04 ± 5.56 before ECT and 8.73 ± 3.96 after ECT [23]. In our study, GDS values decreased in intra-group comparison after ECT and correlated with similar previous studies. There was no difference between the groups in terms of GDS scores before and after ECT; however, post-ECT GDS values were significantly lower in both groups (P = 0.003) according to the Student-t test.
Limitations
The most important limitation of our study is that it was retrospective and conducted with a small number of patients. Prospective planning of future studies may help to determine the side effects in more detail.
Conclusion
In conclusion, Sch and rocuronium-sugammadex combination during anesthesia showed similar seizure efficacy and recovery in geriatric patients undergoing repeated ECT. Geriatric Depression Scores of the patients before ECT decreased compared to after ECT, and both agents had similar therapeutic efficacy. As a side effect, muscle pain was more common in the group using Sch, but no systemic side effect leading to serious problems was observed. Rocuronium-sugammadex may be preferred as an alternative to Sch in geriatric patients.
Tables
Table 1. Measures of ECT stimulus dose, EEG seizure duration, motor seizure duration, hospitalization, orientation, and postoperative recovery time of the groups
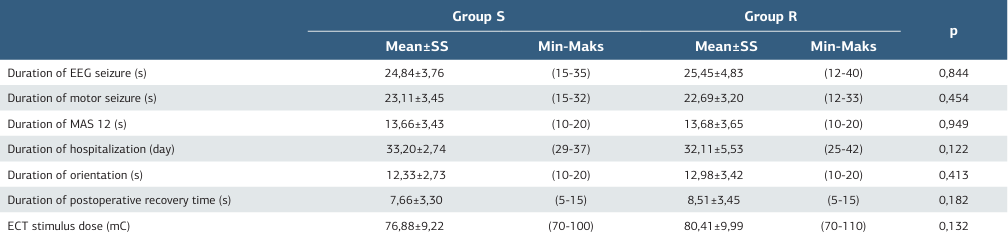
Table 2. Side effects of the groups
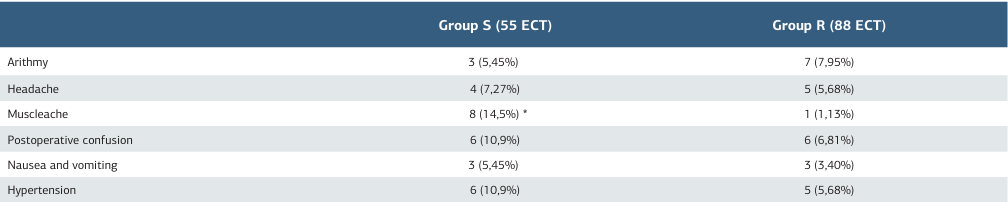
Group S: ECT using succinylcholine as a neuromuscular blocker, Group R: ECT using rocuronium as a neuromuscular blocker, ECT: Electroconvulsive therapy *: p < 0.05
Table 3. Geriatric depression score before ECT and after ECT of the groups
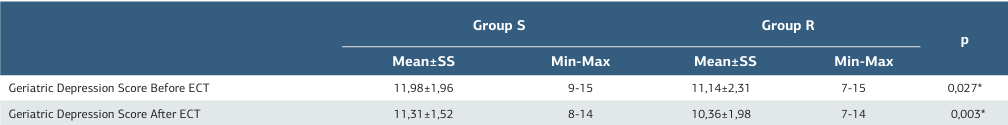
Group S: ECT using succinylcholine as a neuromuscular blocker, Group R: ECT using rocuronium as a neuromuscular blocker, ECT: Electroconvulsive therapy *: p< 0.05. SS: Standard deviation, Min: Minimum, Max: Maximum
References
-
Durmaz B, Soysal P, Ellidokuz H, Isik AT. Validity and reliability of geriatric depression scale-15 (short form) in Turkish older adults. North Clin Istanb. 2018;5(3):216-20.
-
Heijnen WT, Birkenhäger TK, Wierdsma AI, van den Broek WW. Antidepressant pharmacotherapy failure and response to subsequent electroconvulsive therapy: A meta-analysis. J Clin Psychopharmacol. 2010;30(5):616-9.
-
Wagner KJ, Möllenberg O, Rentrop M, Werner C, Kochs EF. Guide to anaesthetic selection for electroconvulsive therapy. CNS Drugs. 2005;19(9):745-58.
-
Kadiyala PK, Kadiyala LD. Anaesthesia for electroconvulsive therapy: An overview with an update on its role in potentiating electroconvulsive therapy. Indian J Anaesth. 2017;61(5):373-80.
-
Oflezer C, Atay Ö, Kaşdoğan ZE, Özakay G, İpekçioğlu D, Bahadır H. Does the use of rocuronium-sugammadex instead of succinylcholine in electroconvulsive therapy affect seizure duration? Psychiatry Investig. 2022;19(10):824-31.
-
Taylor S. Electroconvulsive therapy: A review of history, patient selection, technique, and medication management. South Med J. 2007;100(5):494-8.
-
Li H, Hou L, Wang D, et al. Response rate and safety of antidepressants combined with electroconvulsive therapy in adolescent depression: Real-world clinical application. J Affect Disord. 2023;339(10):98-103.
-
Kellner CH, Husain MM, Knapp RG, et al. A Novel Strategy for Continuation ECT in geriatric depression: Phase 2 of the PRIDE study. Am J Psychiatry. 2016;173(11):1110-8.
-
Sackeim HA. Electroconvulsive therapy in late-life depression. In: Roose SP& Sackeim HA, editors. Late-life depression. Oxford University Press; 2004.p.241– 278.
-
Kaliora SC, Zervas IM, Papadimitriou GN. Electroconvulsive therapy: 80 years of use in psychiatry. Psych. 2018;29(4):291-302.
-
Weiner RD, Reti IM. Key updates in the clinical application of electroconvulsive therapy. Int Rev Psychiatry. 2017;29(2):54-62.
-
Türkkal DC, Gökmen N, Yıldız A, et al. A cross-over, post-electroconvulsive therapy comparison of clinical recovery from rocuronium versus succinylcholine. J Clin Anesth. 2008;20(8):589-93.
-
Nishiyama M, Togashi H. Effects of anesthetic agents on seizure duration and hemodinamics in electroconvulsive therapy. Masui. 2009;58(10):1266-9.
-
Köksal E, Üstün YB, Kaya C, Sahin AR, Sahinoglu AH. Elektrokonvülzif tedavide rokuronyum-sugammadeks ve süksinilkolinin derlenme üzerine etkilerinin karşılaştırılması [Comparing the effects of rocuronium-sugammadex and succinylcholine on recovery during electroconvulsive therapy]. Anadolu Psikiyatri Derg. 2015;16(3):198-204.
-
Mirzakhani H, Guchelaar HJ, Welch CA, et al. Minimum effective doses of succinylcholine and rocuronium during electroconvulsive therapy: A prospective, randomized, crossover trial. Anesth Analg. 2016;123(3):587-96.
-
Yalcin S, Aydogan H, Serdaroglu H. Rocuronium-sugammadex as an alternative to succinylcholine in electroconvulsive therapy. J Anesth. 2011;25(4):631.
-
Kramer BA, Kadar AG, Clark K. Use of the Neuro-Wrap system for severe post- electroconvulsive therapy headaches. J ECT. 2008;24(2):152-5.
-
Oflezer C, Atay Ö, Kaşdoğan ZE, Özakay G, İpekçioğlu D, Bahadır H. Does the use of rocuronium-sugammadex instead of succinylcholine in electroconvulsive therapy affect seizure duration? Psychiatry Investig. 2022;19(10):824-31.
-
Takazawa T, Suto T, Aihara M, et al. Comparison between succinylcholine and rocuronium as neuromuscular blocking agents for electroconvulsive therapy in a patient with pseudocholinesterase deficiency. JA Clin Rep. 2015;1(1):7.
-
Sagir O, Yucesoy Noyan F, Koroglu A, Cicek M, Ilksen Toprak H. Comparison between the effects of rocuronium, vecuronium, and cisatracurium using Train of Four and Clinical Tests in elderly patients. Anesth Pain Med. 2013;2(4):142-8.
-
Kadoi Y, Hoshi H, Nishida A, Saito S. Elektrokonvülsif tedavi sırasında üç farklı dozda sugammadeks ve süksinilkolin ile geri döndürüldükten sonra rokuronyumun neden olduğu kas gevşemesinden iyileşme sürelerinin karşılaştırılması [Comparison of recovery times from rocuronium-induced muscle relaxation after reversal with three different doses of sugammadex and succinylcholine during electroconvulsive therapy]. J Anesth. 2011;25(6):855-9.
-
Ertan T, Eker E, Şar V. Geriatrik depresyon ölçeğinin Türk yaşlı nüfusunda geçerlilik ve günenirliği [Validity and reliability of the geriatric depression scale in Turkish elderly population]. Arch Neuropsychiatry. 1997;34(1):62-71.
-
Şahin S, Aybastı Ö. Major depresyonda elektrokonvulsif terapinin oksidatif metabolizma üzerine etkisi [Effect of electroconvulsive therapy on oxidative metabolism in major depressive disorder]. Cukurova Med J. 2017;42(3):513-7.
Declarations
Scientific Responsibility Statement
The authors declare that they are responsible for the article’s scientific content, including study design, data collection, analysis and interpretation, writing, and some of the main line, or all of the preparation and scientific review of the contents, and approval of the final version of the article.
Animal and Human Rights Statement
All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Funding
None
Conflict of Interest
The authors declare that there is no conflict of interest.
Ethics Declarations
This study was approved by the Ethics Committee of Fırat University (Date: 2023-06-11, No: 15880)
Data Availability
The datasets used and/or analyzed during the current study are not publicly available due to patient privacy reasons but are available from the corresponding author on reasonable request.
Additional Information
Publisher’s Note
Bayrakol MP remains neutral with regard to jurisdictional and institutional claims.
Rights and Permissions
About This Article
How to Cite This Article
Serpil Bayındır, Hilal Kaya, Ayşe Azak Bozan, Ümit Karatepe. Anesthetic experiences in recurrent electroconvulsive therapy applications in geriatric patients. Ann Clin Anal Med 2025;16(12):851-855
Publication History
- Received:
- November 20, 2024
- Accepted:
- December 24, 2024
- Published Online:
- January 2, 2025
- Printed:
- December 1, 2025

