The role of ischemia-modified albumin, high sensitivity troponin T, and other inflammatory markers in early diagnosis of acute coronary syndrome in patients presenting to the emergency department with chest pain
Inflammatory markers in early diagnosis of acute coronary syndrome
- Received:
- March 3, 2025
- Accepted:
- April 24, 2025
- Published Online:
- April 27, 2025
- Printed:
- December 1, 2025
Authors
Abstract
Aim Early diagnosis of acute coronary syndrome (ACS) is crucial in emergency medicine. While high-sensitivity troponin (hs-Tn) is a key biomarker, its limitations in the early phase highlight the need for additional markers. Ischemia-modified albumin (IMA) has shown potential in detecting myocardial ischemia, but its clinical value remains uncertain.
Methods Patients presenting with chest pain within three hours were included. Serum IMA and hs-Tn levels were measured, and their combined diagnostic value was assessed. Neutrophil-to-lymphocyte ratio (NLR) and platelet-to-lymphocyte ratio (PLR) were also analyzed.
Results IMA levels were significantly higher in ACS patients than in non-ACS cases (p < 0.05). ROC curve analysis showed that IMA alone had moderate diagnostic performance, but its combination with hs-Tn improved sensitivity and specificity. In the ACS group, IMA levels correlated with hs-Tn, particularly in patients with ST-elevation myocardial infarction (STEMI). NLR and PLR showed no significant differences between ACS and non-ACS patients, confirming their limited diagnostic value.
Conclusion IMA appears to be a promising biomarker for early ACS detection, especially when combined with hs-Tn. This combination could enhance diagnostic accuracy and support early clinical decision-making. Conversely, NLR and PLR were not reliable indicators of ACS. Further research is needed to confirm these findings and explore the clinical applications of IMA in emergency settings.
Keywords
Introduction
Chest pain accounts for approximately 5–10% of emergency department (ED) visits 1,2. Among its many causes, acute coronary syndrome (ACS) is associated with high morbidity and mortality. However, approximately 5% of ACS cases go undiagnosed in the ED due to variable clinical presentations 3,4.
For ACS diagnosis, an electrocardiogram (ECG) should be performed within 10 minutes of admission. If ST-elevation myocardial infarction (STEMI) is detected, immediate treatment is required. In non-STEMI cases, serial cardiac enzyme measurements are recommended. However, troponins indicate myocardial necrosis rather than early ischemic changes 5,6. Since ischemia and inflammation precede necrosis, early detection is crucial, and ED monitoring may last 6–12 hours.
Unstable angina pectoris (UAP), a subset of ACS, is diagnosed when cardiac troponin levels are normal and ECG findings are unremarkable. To improve diagnostic accuracy in UAP and non- STEMI cases, novel biomarkers are needed 7,8.
Ischemia-Modified Albumin (IMA) is an altered form of serum albumin that increases during ischemia, making it a potential early ACS marker. However, elevated IMA levels are also observed in stroke, renal and liver disease, neoplasms, sepsis, and patients undergoing cardioversion, limiting its specificity 9,10. While IMA may aid in ACS detection and risk stratification 9,11, some studies suggest it is insufficient as a standalone marker 7,12.
Neutrophil-to-lymphocyte ratio (NLR) and platelet-to- lymphocyte ratio (PLR) are inflammatory markers associated with coronary artery disease (CAD) 13,14. Their role in CAD remains unclear, but endothelial damage and plaque erosion are linked to neutrophil activity 15.
This study evaluates the diagnostic performance of IMA, NLR, PLR, and high-sensitivity troponin (hs-Tn) in identifying ACS in ED patients with chest pain.
Materials and Methods
Study Design and Setting
This study was a single-center, prospective case-control design conducted at the sole tertiary care center in Çanakkale. Ethical approval was obtained from the hospital’s ethics committee prior to commencement.
Patient Selection
91 patients aged 18 or older, who presented to the ED with chest pain between November 21, 2019, and February 21, 2020, and met the inclusion criteria, were enrolled. Exclusion criteria included non-cardiac causes of chest pain, refusal of coronary angiography (CAG), early hospital discharge, or transfer to another center. Additionally, patients with hypoalbuminemia or incomplete data were excluded.
Data Sources
Patients who met the inclusion criteria were randomly selected, and data were gathered from medical records, legal guardians, and the hospital’s automation system. The data collection form was designed to standardize and facilitate systematic data gathering, ensuring all relevant clinical, demographic, and laboratory information was recorded.
Data Collection
Demographic, clinical, and laboratory data were collected, including vital parameters, medical history, smoking and alcohol habits, chest pain characteristics, and laboratory results such as high-sensitivity troponin (hs-Tn), ischemia- modified albumin (IMA), neutrophil-to-lymphocyte ratio (NLR), platelet-to-lymphocyte ratio (PLR), and mean platelet volume (MPV). Informed consent was obtained from all patients. Blood samples were collected for various analyses, stored at -80°C, and analyzed after the study period.
IMA and Hs-Tn Analysis
IMA levels were measured using an ELISA method with specific human IMA kits, while hs-Tn was analyzed using an automated photometric-colorimetric method in the biochemistry laboratory. MPV, NLR, and PLR were determined via automated hemogram analysis.
Outcome Measures
The primary outcome was that IMA exhibited higher specificity than hs-Tn in early ACS detection. The secondary outcome emphasized the potential for false positives with hs-Tn due to its sensitivity, suggesting the combined use of IMA and hs-Tn could reduce diagnosis delays.
Statistical Analysis
SPSS software version 26.0 was used for data analysis. Descriptive statistics, univariate analysis, and receiver operating characteristic (ROC) curve analysis were performed. Sensitivity and specificity were calculated for parameters with an area under the curve (AUC) > 0.600, with a p-value of < 0.05 considered statistically significant.
Ethical Approval
This study was approved by the Ethics Committee of Çanakkale Onsekiz Mart University Faculty of Medicine (Date: 2019-11- 13, No: 2019-18).
Results
A total of 91 patients were included, with 64.84% male and a mean age of 57.79 ± 18.28 years. Of these, 61.54% (n = 56) presented within 3 hours of chest pain onset. Hypertension (38.5%), diabetes mellitus (24.2%), coronary artery disease (37.4%), and smoking (37.4%) were the most common comorbidities. The average hs-troponin level was 304.26 ± 901.28 pg/mL, with 73.6% diagnosed with acute coronary syndrome (ACS), including 52.2% NSTEMI, 26.9% STEMI, and 20.9% unstable angina pectoris (USAP) (Table 1).
ACS patients were significantly older (p < 0.001), but no significant differences were found regarding gender, vital signs, or comorbidities. ACS patients had significantly higher hs-troponin and IMA levels (p < 0.001), but no differences in MPV, NLR, and PLR values. ACS patients showed higher ECG abnormalities and hospitalization rates.
STEMI patients were significantly older than those with NSTEMI or USAP. No significant differences were found between ACS types in terms of gender, vital parameters, comorbidities, or laboratory results. USAP patients had lower ECG abnormalities and hospitalization rates compared to STEMI and NSTEMI patients.
In early-presenting patients (≤ 3 hours), hs-troponin levels were higher in the 3–24 hour group, while IMA levels were higher in the early-presenting group. NLR and PLR were higher in patients presenting later (3–24 hours), but no significant difference was found in MPV levels (Table 2).
A strong positive correlation (r = 0.86) was observed between IMA and hs-troponin, and a moderate positive correlation (r = 0.39) between IMA and NLR (p = 0.05) (Table 3).
For early presenters (≤ 3 hours), IMA had an AUC of 0.690 with 69% sensitivity and 82% specificity at a cutoff of 1.28. For those presenting within 24 hours, IMA’s AUC was 0.650 with 73.6% sensitivity and 60% specificity at a cutoff of 0.415. In comparison, hs-troponin had an AUC of 0.780 for ≤ 3 hours and 0.910 for ≤ 24 hours, indicating higher specificity after 3 hours. IMA showed higher specificity in the first 3 hours (Figure 1, Figure 2).
Discussion
Introduction and Significance of Early ACS Diagnosis
Chest pain is a common cause of emergency department visits, significantly straining resources. Diagnosing Acute Coronary Syndrome (ACS) is crucial to avoid risks to patient lives and medicolegal issues for clinicians. There is a need for biomarkers to improve the early diagnosis of ACS. In our study, Ischemia Modified Albumin (IMA) emerged as a more sensitive parameter than high-sensitivity troponin (hs-troponin), especially in patients presenting within the first 3 hours. We believe that IMA could serve as an early marker of ischemia before necrosis occurs.
Role of IMA in ACS Diagnosis
IMA, an FDA-approved biomarker for ruling out ACS, increases in ischemic conditions due to alterations in the N-terminal sequence of human albumin. In myocardial infarction, IMA rises rapidly and normalizes within 24 hours 17. Previous studies have demonstrated that IMA has a high negative predictive value (NPV) and outperforms other biomarkers in excluding ACS 18,19,20. In our study, IMA had better specificity than hs- troponin in the first 3 hours. We suggest that combining IMA with hs-troponin could improve early ACS detection.
Inflammation and Cardiovascular Disease
Inflammation plays a critical role in both ACS and atherosclerosis. Parameters like Neutrophil-to-Lymphocyte Ratio (NLR), Platelet- to-Lymphocyte Ratio (PLR), and Mean Platelet Volume (MPV) help monitor these inflammatory processes. While studies have shown NLR and PLR’s value in cardiovascular risk prediction 21,23,24, our study found them ineffective in identifying ACS patients or distinguishing ACS subtypes. NLR and PLR levels were higher in patients presenting later (3–24 hours).
Limitations
Our study has limitations, including being a single-center study with a small sample size. To generalize the findings, future multicenter, randomized, double-blind studies with larger sample sizes are needed.
Conclusion
This conclusion highlights the importance of early, accurate diagnostics in patients presenting with chest pain. It seems that combining IMA with hs-troponin could be a promising approach to improve the detection of acute coronary syndrome (ACS) in the critical early hours. Your findings emphasize the need for careful interpretation of NLR and PLR in these cases.
Declarations
Ethics Declarations
This study was approved by the Ethics Committee of Çanakkale Onsekiz Mart University (Date: 2019-11-13, No: 2019-18)
Animal and Human Rights Statement
All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Data Availability
The datasets used and/or analyzed during the current study are not publicly available due to patient privacy reasons but are available from the corresponding author on reasonable request.
Conflict of Interest
The authors declare that there is no conflict of interest.
Funding
None
Scientific Responsibility Statement
The authors declare that they are responsible for the article’s scientific content, including study design, data collection, analysis and interpretation, writing, and some of the main line, or all of the preparation and scientific review of the contents, and approval of the final version of the article.
References
-
Owens PL, Barrett ML, Gibson TB, Andrews RM, Weinick RM, Mutter RL. Emergency department care in the United States: A profile of national data sources. Ann Emerg Med. 2010;56:150-65.
-
Jawade P, Khillare KM, Mangudkar S, Palange A, Dhadwad J, Deshmukh M. A comparative study of ischemia-modified albumin: A promising biomarker for early detection of acute coronary syndrome. Cureus. 2023;15(8):e44357.
-
Bhardwaj A, Truong QA, Peacock WF, et al. A multicenter comparison of established and emerging cardiac biomarkers for the diagnostic evaluation of chest pain in the emergency department. Am Heart J. 2011;162(2):276-82.
-
Çakır A, Akyol PY, Acar H. The effect of stress hyperglycemıa seen ın acute ST- segment elevatıon ın myocardıal ınfarctıon on ın-hospıtal mortalıty. Ir J Med Sci. 2023;192(3):1109-14.
-
Thygesen K, Alpert JS, White HD, et al. Universal definition of myocardial infarction. Circulation. 2007;116(22):2634-2653. doi:10.1161/CIRCULATIONAHA.107.187397.
-
Lin S, Yokoyama H, Rac VE, Brooks SC. Novel biomarkers in diagnosing cardiac ischemia in the emergency department: A systematic review. Resuscitation. 2012;83(6):684-91.
-
Shin H, Kim JG, Jang BH, et al. Diagnostic accuracy of ischemia-modified albumin for acute coronary syndrome: A systematic review and meta-analysis. Medicina (Kaunas). 2022;58(5):614.
-
Mou H, Shao J, Zhang J, Yang J, Yu S, Wang H. Ischemia-modified albumin to evaluate short-term prognostic of patients with acute coronary syndrome. J Coll Physicians Surg Pak. 2021;31(7):841-5.
-
Ralapanawa U, Sivakanesan R, Tennakoon S, Karunathilake P. Ischemia- modified albumin: Is it a promising marker in acute coronary syndrome? BMC Cardiovasc Disord. 2024;24(1):436.
-
Kumar A. Ischemia-modified albumin: Its diagnostic implications and shortfalls. J Biomed Sci. 2022;1(3):1-3.
-
Yang F, Ma L, Zhang L, et al. Association between serum lipoprotein- associated phospholipase A2, ischemic modified albumin and acute coronary syndrome: a cross-sectional study. Heart Vessels. 2019;34(10):1608-14.
-
Demir MT, Baydin A, Amanvermez R, Erenler AK, Güzel M, Yücel O. Comparison of pentraxin-3 and ischemia-modified albumin with troponin in early diagnosis of acute coronary syndrome. Bratisl Lek Listy. 2018;119(8):509-12.
-
Maleki M, Tajlil A, Separham A, et al. Association of neutrophil to lymphocyte ratio (NLR) with angiographic SYNTAX score in patients with non-ST-segment elevation acute coronary syndrome (NSTE-ACS). J Cardiovasc Thorac Res. 2021;13(3):216-21.
-
Rajakumar HK, Coimbatore Sathyabal V, Vasanthan M, Dasarathan R. The predictive role of Systemic Inflammation Response Index (SIRI), Neutrophil- Lymphocyte Ratio (NLR), and Platelet-Lymphocyte Ratio (PLR) in the prognosis of acute coronary syndrome in a tertiary care hospital. Heliyon. 2024;10(20):e39029.
-
Badiger S, M J L, Jugati AV. Assessment of severity of ST-elevation myocardial infarction using neutrophil-to-lymphocyte ratio and its correlation with thrombolysis in myocardial infarction risk score. Cureus. 2024;16(9):e68877.
-
Peacock F, Morris DL, Anwaruddin S, et al. Meta-analysis of ischemia-modified albumin to rule out acute coronary syndromes in the emergency department. Am Heart J. 2006; 152:253-62.
-
Patil SM, Banker MP, Padalkar RK, et al. The clinical assessment of ischemia- modified albumin and troponin I in the early diagnosis of the acute coronary syndrome. J Clin Diagn Res. 2013;7:804-8.
-
Christenson RH, Duh SH, Sanhai WR, et al. Characteristics of an albumin cobalt binding test for assessment of acute coronary syndrome patients: A multicenter study. Clin Chem. 2001;47(3):464-70.
-
Lee YW, Kim HJ, Cho YH, Shin HB, Choi TY, Lee YK. Application of albumin- adjusted ischemia modified albumin index as an early screening marker for acute coronary syndrome. Clin Chim Acta. 2007;384:24-7.
-
Wahab MAKA. Ischemia modified albumin (IMA) in acute coronary syndrome (ACS) and left bundle branch block (LBBB). Does it make the difference? Egypt Heart J. 2017;69(3):183-90.
-
Li Q, Yu Y, Zhou YQ, et al. Predictive value of neutrophil-to-lymphocyte ratio in coronary chronic total occlusion patients. J Geriatr Cardiol. 2024;21(5):542-9.
-
Zhang M, Sun Y, Zhang L, Xu Y, Liu Y, Li K. The application of mass defect percentage in the evaluation of acute coronary syndrome. Nucl Med Commun. 2025;46(1):1-6.
-
Verdoia M, Barbieri L, Di Giovine G, Marino P, Suryapranata H, De Luca G. Novara Atherosclerosis Study Group (NAS). Neutrophil to lymphocyte ratio and the extent of coronary artery disease: Results from a large cohort study. Angiology. 2016;67(1):75-82.
-
Zhou D, Fan Y, Wan Z, et al. Platelet-to-lymphocyte ratio improves the predictive power of GRACE risk score for long-term cardiovascular events in patients with acute coronary syndrome. Cardiology. 2016;134(1):39-46.
Figures
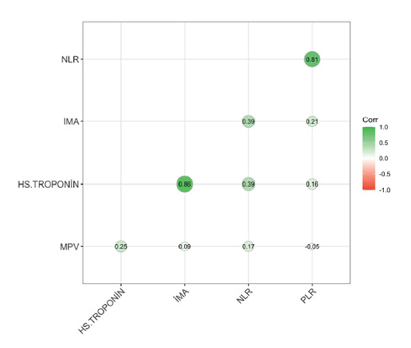
Figure 1. Evaluation of the correlation between cases and IMA levels
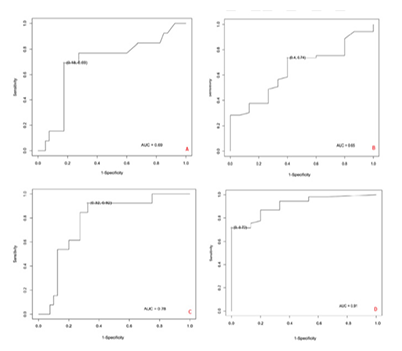
Figure 2. Evaluation of sensitivity and specificity levels of IMA and Hs-Troponin levels in the first 3 hours and first 24 hours
Tables
Table 1. Comparison of demographic and clinical data of cases according to ACS diagnoses
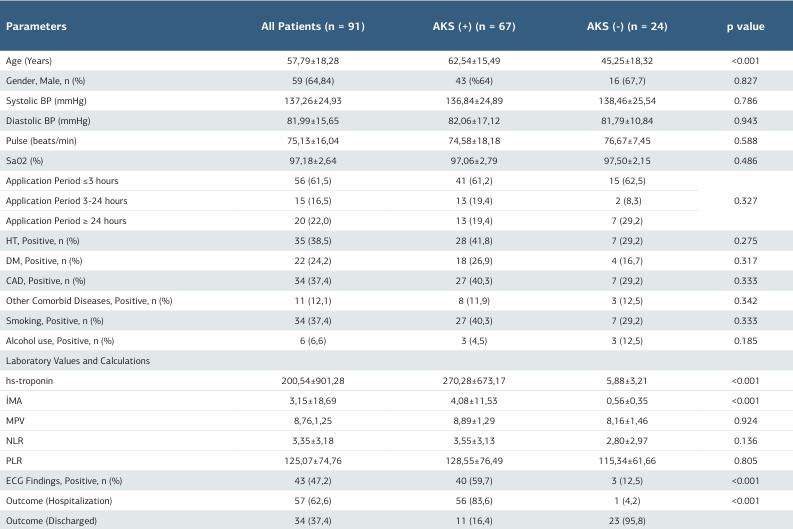
BP: Blood Pressure; Data shown in n (%) or mean± standard deviation
Table 2. Comparison of demographic and clinical data of cases according to ACS types
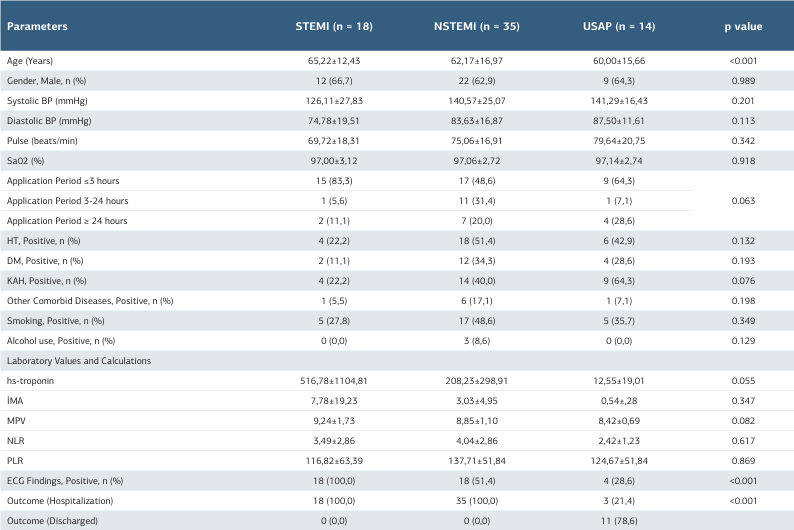
BP: Blood Pressure; Data shown in n (%) or mean± standard deviation
Table 3. Comparison of biomarkers according to application times
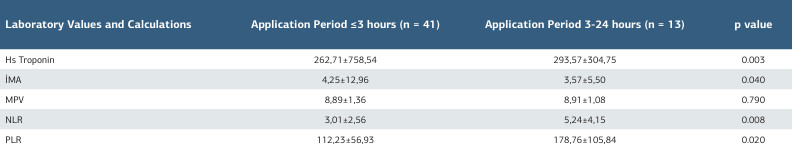
*:T Test used
Additional Information
Publisher’s Note
Bayrakol MP remains neutral with regard to jurisdictional and institutional claims.
Rights and Permissions
About This Article
How to Cite This Article
Yasemin Çetinkaya, Canan Akman. The role of ischemia-modified albumin, high sensitivity troponin T, and other inflammatory markers in early diagnosis of acute coronary syndrome in patients presenting to the emergency department with chest pain. Ann Clin Anal Med 2025;16(12):867-871

