Retrospective evaluation of pulp revascularization treatment in immature permanent teeth
Regenerative endodontic treatment
Authors
Abstract
Aim The aim of this study was to investigate the results of regenerative endodontic treatments (RETs) for necrotic immature teeth.
Materials and Methods Data were collected on children who were treated with RETs and were followed up for two years. The American Association of Endodontists protocol for RETs was used to treat all patients. The outcome of RETs was evaluated as complete healing, incomplete healing, and failure. Twenty-four teeth were included in the study.
Result Among these 24 teeth, 10 were anterior, 2 were premolars, and 12 were molars. During the follow-up period, 15 out of 24 teeth (62.5%) healed completely, 8 teeth (33.3%) showed incomplete healing, and one tooth (4.1%) failed and required further treatment.
Discussion Within the limitations of this study, the results indicate that regenerative endodontic treatments (RETs) using calcium hydroxide as an intracanal medicament are effective in promoting periapical healing and root maturation in immature necrotic teeth. The high success rate observed supports RET as a viable alternative to apexification. However, further studies with larger sample sizes and longer follow-up periods are needed to confirm these findings and establish standardized treatment protocols.
Keywords
Introduction
In an immature tooth, treating pulpal necrosis is challenging for both the patient and dentist. In addition, the presence of thin dentine walls and non-closure of the apex complicates the endodontic treatment [1].
Apexification with calcium hydroxide (Ca(OH)2) is the traditional treatment option for immature necrotic teeth which aims to create an apical hard tissue barrier. Despite its widespread use, the apexification technique with Ca(OH)2 requires a long treatment period with multiple visits. This situation poses a challenge for patients to comply with treatment [2]. In addition, the unpredictable root apex closure time and the increased possibility of root fracture due to the thin and fragile roots have raised doubts about this treatment protocol [3, 4]. Regenerative endodontic treatments (RETs) can be an alternative treatment approach in necrotic immature permanent teeth with impaired structured integrity, with the potential to allow the progress of root development [5].
RET requires comprehensive root canal sterilization, achievable through irrigation solutions and intracanal medications. The use of a variety of intracanal medications has been advocated in RET, including Ca(OH)2, triple antibiotic paste (TAP), and double antibiotic paste (DAP) [1, 6]. Reports on Ca(OH)2 treatment are increasing due to the success of Ca(OH)2, used in revascularization in disinfecting root canals and promoting the proliferation of SCAP [1, 6, 7].
These case series illustrate the outcomes of a two-year follow- up of the revascularization procedure in immature necrotic permanent teeth treated with Ca(OH)2 medicament.
Materials and Methods
Case Inclusion
Data were obtained from children treated with RET who were followed for two years from June 2019 to January 2022 at the Department of Pediatric Dentistry, Inonu University. Patients’ genders, ages, dental histories, number of the treated teeth, and the presence/ absence of periapical radiolucency in treated teeth were recorded. After that, treatment and follow-up times, the details of the clinical protocol, and any variations were also saved.
Initial and follow-up periapical radiographs of the patients were obtained from the Planmeca Romexis (Helsinki, Finland, 2015) program. The radiography angle was standardized by using the same machine and the same performer (M.B.S.). Examination and treatment notes were extracted from the database system used by faculty (METASOFT DentAssist Version 3.0.172).
The study group consisted of teeth of paediatric patients aged 7-10 years, who applied to our clinic for the restorative and endodontic treatment of immature permanent teeth. All treatments were performed at the clinic from June 2019 to January 2020 by a pediatric dentist (M.B.S.) under the supervision of two pediatric dentists (B.D., H.A.) with more than 5 years of experience in pediatric dentistry.
In the study group, pulp necrosis was diagnosed with clinical and radiographic examinations. On clinical examination, the teeth showed sensitivity to percussion and palpation, ranging from minor to severe. Periodontal examination revealed physiological mobility around the teeth, and a normal probing depth (<3 mm).
None of the teeth responded to either the cold or the electric pulp test (EPT). Adjacent and opposite teeth reacted positively to both tests. No fistula tract and swelling were determined in the buccal mucosa. Periapical radiographs were evaluated, showing immature apices and wide canals with parallel walls. RET was planned for the affected teeth considering incomplete root development with a wide-open apex. Parental consent was obtained and treatment was initiated in the same session.
Teeth with the following criteria were included in the study:
Inclusion Criteria
1. Single or multi-rooted teeth followed up for 2 years after RETs,
2. RETs using Ca(OH)2 as intracanal medicament and blood clot as a scaffold were included.
3. Complete pre-and post-treatment records.
Exclusion Criteria
1. Patients using different capping materials other than MTA
2. Teeth with different types of intra-canal medications for RETs,
3. Incomplete medical or radiographic records,
4. Patients without regular follow-up for 2 years.
Revascularization Protocol
The RET protocol of The American Association of Endodontists (AAE) was applied to all teeth included in the study (Available at: https://www.aae.org/specialty/wp-/content/uploads/ sites/2/2021/08/ClinicalConsiderationApprovedByREC062921. pdf). All cases were treated in two sessions. The tooth was anesthetized with 2% lidocaine with 1:100,000 epinephrine. Then, an access cavity was created in isolation with a rubber dam. The access cavity was opened, and the pulp chamber was entered. The canal was passively irrigated with 20 mL of 1.5% NaOCl with a 27-gauge open-ended needle placed 1-2 mm below the canal opening and then dried with a paper point (Dentsply Maillefer). Then, Ca(OH)2 powder was mixed with sterile water (Merck, Darmstadt, Germany) at a ratio of 3:1. Ca(OH)2 paste was placed in the canal 3 mm shorter than the working length using a lentulo spiral. The access cavity was closed with Cavit (3M Espe, St Paul, MN). Patients were recalled 4 weeks later.
At the second appointment, signs and symptoms which include pain, swelling, sinus, or fistula had completely disappeared. Anesthesia was achieved with 3% mepivacaine (Citanest; AstraZeneca, London, UK) without vasoconstrictor, isolation was achieved with rubber dam. The temporary restoration was removed. 20 ml of 17% EDTA (Formula e Ac ~aoTM, Sao Paulo, Brazil) solution was performed for 5 minutes in irrigation and dried with paper points. Apical bleeding was induced using #15 K-files. It was initiated by rotating a pre-curved K-file 2 mm beyond the apical foramen to ensure the complete filling of the canal with blood up to the level of the cementoenamel junction. After blood clot formation, RetroMTA (BioMTA, Seul, Kore) prepared according to the manufacturer’s instructions was applied onto the blood clot. Then, a wet cotton pellet was placed over the RetroMTA and sealed with Cavit (3M Espe, St Paul, MN). The temporary restoration was removed one day later and RetroMTA hardness was provided. Glass ionomer cement (GIC) with 2 mm thickness(Fuji; Fuji Corporation, Osaka, Japan) was placed over the RetroMTA. Finally, the tooth was restored with composite resin. Radiographic and clinical controls were performed at 6 weeks, 3 months, 6 months, 1 year, and 2 years.
Evaluation of Healing
The achievement of primary, secondary, and tertiary goals primarily gauges the success of Regenerative Endodontic Procedures:
1. Primary goal: The absence of symptoms and the presence of evidence indicating bone regeneration.
2. Secondary goal: Increased root wall thickness and/or increased root length (desirable, but perhaps not essential)
3. Tertiary goal: Positive response to vitality testing (which if achieved, could indicate a more organized vital pulp tissue) (Available at: https://www.aae.org/ specialty/wp-content/uploads/sites/2/2021/08/ ClinicalConsiderationsApprovedByREC062921.pdf).
This study’s primary goal is to eliminate symptoms on clinical and radiographic examination and bone healing although there is no consensus on how healing occurs. A secondary but not essential aim is to increase root length and thickness (Available at: https:// www.aae.org/specialty/wp/content/uploads/sites/2/2021/08/ ClinicalConsiderationsApprovedByREC062921.pdf). The clinical outcomes were evaluated using radiographic healing of apical periodontitis, clinical signs, radiographic signs and symptoms of ongoing root development. Teeth that met goals 1 and 2 were considered successful. The third goal was not evaluated in this study.
Calibration
The only pediatric dentist specializing in this field performed the RET procedure. Two pediatric dentists (M.B.S., B.D.) and one research assistant (H.A.) in pediatric dentistry experienced with the revascularization procedure were given a detailed description of the outcome criteria used for radiographic evaluation in this study. The radiographs representing each outcome category for normalization were shown. All periapical radiographs were projected onto a large screen in a dark room and viewed randomly. After discussion, when all those who evaluated the images (M.B.S., S.D., P.D.) reached a consensus, a specific healing category was assigned to each radiograph. The Kappa test was performed for inter-rater agreement and consistency of evaluations.
Ethical Approval
This study was approved by the Ethics Committee of Inonu University Non-Interventional Clinical Research (Date: 2021- 11-16, No:2609).
Results
According to Kappa test, all three observers are in agreement with each other, and the agreement value is 1.0. The radiographic evaluation agreement is in the range of 0.7-1.0. Accordingly, no statistically significant difference was found between observers.
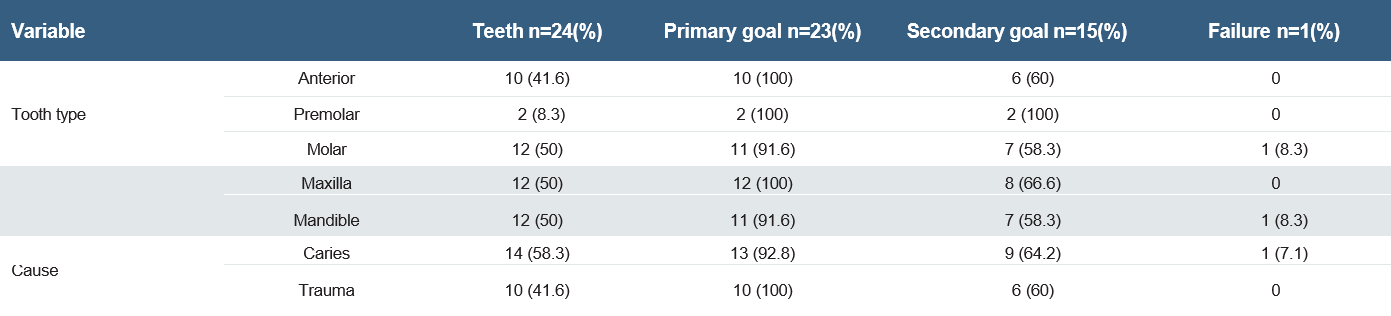
Initially, RET was applied to 54 teeth and follow-up was started. However, 30 of 54 patients did not have regular follow-up checks. As a result of the retrospective review of these cases, 24 children met the inclusion criteria. Of these 24 teeth, 10 teeth were anterior, 2 were premolars, and 12 were molars. Table 1 summarizes the causes, radiological and clinical characteristics, and treatment outcomes for teeth undergoing RETs. During the follow-up period, 23 (95.8%) of 24 patients met the primary goal. One molar tooth (4.1%) did not improve clinically and radiographically. Representative cases of each category (i.e., failure, secondary goal and primary goal) are presented in Figures 1, 2, and 3, respectively.
Caries and trauma accounted for 58.3% and 41.6% of cases in which RET was applied to immature necrotic teeth. While the secondary goal was achieved in 60% (n=6) of the teeth with a history of dental trauma, the primary goal was achieved in 100%. In the group with tooth decay, 7.1% (n=1) failure, 28.5% (n=64.2) met the secondary goal, and 92.8% (n=13) achieved the primary goal.
The success rate was 95.8% when we assessed the cases based on the clinical success criterion and the necessity for retreatment. The presence of signs and symptoms during treatment was also evaluated; when the regeneration process was initiated, 22 of 24 (91.6%) patients were symptomatic, 2 (8.3%) cases were asymptomatic, and there was no case without apical radiolucency. In the post-treatment and following controls, all of the teeth except one were asymptomatic and the periapical lesion was completely healed.
Discussion
Regeneration procedure has become a favourable alternative for the treatment of immature necrotic teeth, with promising clinical and radiographic results [8]. In RETs, promoting root maturation and thus preventing complications (such as root fracture) may be seen as one of its most important advantages. Inducing root formation makes it a better option over apexification. In this situation, it may be correct to say with numerous studies on regeneration that the outcome analysis should comprise both radiographic recovery of apical periodontitis and radiographic findings of further root maturation [8, 9].
Histological analysis of the treated teeth with RET has revealed the presence of newly formed tissues such as cementum, ectopic bone, and periodontal ligament, instead of dental pulp or pulp-like tissue [10, 11, 12]. In a recent case report, it was discovered that a tooth, that had undergone root-end surgery (RETs), showed healthy fibrous connective tissue containing blood vessels within the canal space. Moreover, the results of the immunohistochemical analysis demonstrated positive staining for vascular and neuronal markers, indicating the potential for partial regeneration of components of the pulp-dentin complex [13]. Although the aim of RET offered in this study are similar to those identified and acknowledged by the AAE, the success criteria differ. In this study, the success criteria was to eliminate clinical symptoms and apical radiolucency, regardless of thickening the root wall and/or increasing the root length, and 95.8% of the teeth met this criterion. When the cases are evaluated according to the AAE criteria, our data disclosure that 95.8% of the cases achieved the primary aim (improvement of symptoms) and 62.5% of the cases achieved the secondary aim (increase in root size). The tertiary aim wasn’t evaluated in the present study (positive response to vitality tests). This is one of the limitations of our study.
One of the agents that play an important role in the recovery of RET are intracanal medicaments used to provide disinfection. TAP, DAP and Ca(OH)2 are used for this purpose. In this study, successful results were achieved by using Ca(OH)2 as an intracanal medication, similar to the findings in the study by Saoud and colleagues [14]. Ahmed et al [15] in the clinical study where they applied RET to 8 molars, they achieved a success rate of 57%. In this study, the success rate we achieved in molars was 91.6%. This difference may be due to the difference in intracanal medication used. In the study of Bukhari et al. [8] secondary goal was observed at the rate of 75%, while in the present study, the secondary goal was achieved in 62.5% of cases. This difference can be attributed to the fact that more anterior teeth were included in Bukhari’s study, the inner canal wall of the anterior teeth was wider, and it was easier to apply to the anterior tooth [8]. The majority of studies on RET are related to incisors and premolar teeth [16]. RET in molars is a difficult treatment to apply and follow as it requires disinfection of 3 or 4 canals and the formation of blood clots. In their study on RET, Tzanakis et al. [17] although there are case series on molars, it has been concluded that these are not sufficient to prove clinical success. In the current study, 12 molar teeth were evaluated. This is a good number considering the studies in the literature [8, 14, 18, 19].
Root development and healing of the periapical tissues may take longer in some cases. In the incomplete healing group, in all cases, the periapical pathology was completely healed; this satisfies at least 1 success criteria of treatment. In these RETs cases with two-year follow-up, complete healing occurred within the first 9 months [14]. In the study of Çehreli et al. [19], similar to this study, the cases were clinically asymptomatic for the first 3 months, showed complete radiographic recovery and an increase in root size was observed at 9 months. In cases where clinical symptoms and signs persist and/or increase in periradicular lesion size considered unsuccessful in RETs, a second RETs entry or apexification procedure should be started to preserve the patient’s natural tooth structure and restore function [8]. In one failure case detected in this study, apexification with MTA was performed.
In this study, all cases were followed for 2 years. Studies with 2-year follow-ups in the literature suggest that RET may be a suitable treatment option for immature teeth based on their results [20, 21, 22].
Some researchers have mathematically measured dentine thickness and root maturation modifications using computer programs [9, 19]. While electronic evaluation of root maturation holds significant value as a research tool, its feasibility for routine clinical application may be limited. Unlike Jeeruphan et al. [9], no mathematical representation of root maturation could be acquired in the present study. Similar to the study by Bukhari et al. [8], three categories were determined complete, incomplete healing, and non-healing. For this reason, in this study, the determination of apical healing and root formation was performed subjectively by three experienced pediatric dentists, although this method has its limitations. Additionally, due to the small sample size in this study, no further statistical analysis was performed.
Limitations
This study has several limitations
1. Small Sample Size: Limited cases prevented comprehensive statistical analysis.
2. Subjective Assessment: Apical healing and root formation were evaluated without objective digital measurements.
3. Lack of Mathematical Analysis: Root maturation and dentin thickness were not digitally measured.
4. Limited Success Criteria: Success was mainly defined by symptom resolution, without vitality testing.
Further studies with larger samples and longer follow-ups are needed.
Conclusion
The present study constitutes a case series demonstrating that biologically based therapeutic approaches may be of particular value in promoting apical closure and root development. Based on the results of this case series RET with Ca(OH)2 may be a suitable treatment option for immature teeth.
Figures
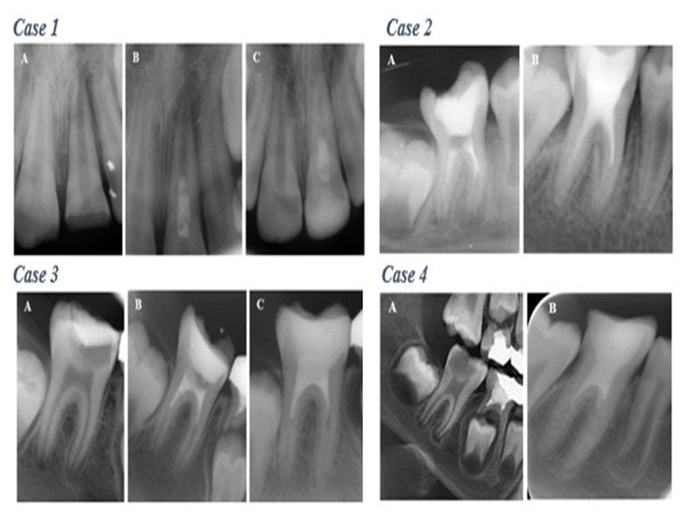
Figure 1. Complete healing category. Case 1. Maxillary right central incisor. Increased thickening of the canal walls and continued root maturation after revascularization; (A) Preoperative radiography. (B) Postoperative radiography. (C) Follow-up radiograph at 24 months. Case 2. Mandibular right first molar; (A) Preoperative radiography. (B) Follow-up radiograph at 24 months. Case 3. Mandibular right first molar; (A) Preoperative radiography. (B) Postoperative radiography. (C) Follow-up radiograph at 24 months. Case 4. Mandibular right first molar. (A) Preoperative radiography. (B) Follow-up radiograph at 24 months

Figure 2. Incomplete healing category. Case 1. Maxillary right central incisor. Size of apical radiolucency considerably improved but did not completely resolve with slight increase in the root length along mesial walls; (A) Preoperative radiography. (B) Follow-up radiograph at 3 months. (C) Follow-up radiograph at 30 months. Case 2. Mandibular right first molar. Size of apical radiolucency improved considerable with no further root growth in length or thickness; (A) Preoperative radiography. (B) Follow-up radiograph at 6 months. (C) Follow-up radiograph at 24 months

Figure 3. Failure category. Case 1. Mandibular left first molar. Failed case, patient was symptomatic 3 months after completing the treatment. (A) Operative radiography. (B) Follow-up radiograph at 3 months postoperatively
Tables
Table 1. Causes, radiological and clinical characteristics, and treatment outcomes for teeth undergoing regenerative endodontic treatments (RETs)
References
-
Antunes LS, Salles AG, Gomes CC, Andrade TB, Delmindo MP, Antunes LA. The effectiveness of pulp revascularization in root formation of necrotic immature permanent teeth: a systematic review. Acta Odontol Scand. 2016;74(3):161-9.
-
Sheehy EC, Roberts GJ. Use of calcium hydroxide for apical barrier formation and healing in non-vital immature permanent teeth: A review. Br Dent J. 1997;183(7):241-6.
-
Rafter M. Apexification: A review. Dent Traumatol. 2005;21(1):1-8.
-
Kahler SL, Shetty S, Andreasen FM, Kahler B. The effect of long-term dressing with calcium hydroxide on the fracture susceptibility of teeth. J Endod. 2018;44(3):464-469.
-
Murray PE, Garcia-Godoy F, Hargreaves KM. Regenerative endodontics: A review of current status and a call for action. J Endod. 2007;33(4):377-90.
-
Kharchi AS, Tagiyeva-Milne N, Kanagasingam S. Regenerative endodontic procedures, disinfectants and outcomes: A systematic review. Prim Dent J. 2020;9(4):65-84.
-
Ruparel NB, Teixeira FB, Ferraz CC, Diogenes A. Direct effect of intracanal medicaments on survival of stem cells of the apical papilla. J Endod. 2012: 38: 1372–5.
-
Bukhari S, Kohli MR, Setzer F, Karabucak B. Outcome of revascularization procedure: a retrospective case series. J Endod. 2016;42(12):1752-9.
-
Jeeruphan T, Jantarat J, Yanpiset K, Suwannapan L, Khewsawai P, Hargreaves KM. Mahidol study 1: Comparison of radiographic and survival outcomes of immature teeth treated with either regenerative endodontic or apexification methods: A retrospective study. J Endod. 2012;38(10):1330-6.
-
Zhou R, Wang Y, Chen Y, et al. Radiographic, histologic, and biomechanical evaluation of combined application of platelet-rich fibrin with blood clot in regenerative endodontics. J Endod. 2017;43,2034–40.
-
Shimizu E, Ricucci D, Albert J, et al. Clinical, radiographic, and histological observation of a human immature permanent tooth with chronic apical abscess after revitalization treatment. J Endod. 2013;39, 1078–83.
-
Xu F, Qiao L, Zhao Y, et al. The potential application of concentrated growth factor in pulp regeneration: An in vitro and in vivo study. stem cell research & therapy. 2019;10, 1-16.
-
Austah O, Joon R, Fath WM, et al. Comprehensive characterization of 2 immature teeth treated with regenerative endodontic procedures. J Endod. 2018;44(12),1802-11.
-
Saoud TM, Martin G, Chen YH, et al.Treatment of mature permanent teeth with necrotic pulps and apical periodontitis using regenerative endodontic procedures: A case series. J Endod. 2016;42(1):57-65.
-
Ahmed YE, Ahmed GM, Ghoneim AG. Evaluation of postoperative pain and healing following regenerative endodontics using platelet-rich plasma versus conventional endodontic treatment in necrotic mature mandibular molars with chronic periapical periodontitis. A randomized clinical trial. Int Endod J. 2023;56(4):404-418.
-
Shetty H, Shetty S, Kakade A, Mali S, Shetty A, Neelakantan P. Three- dimensional qualitative and quantitative analyses of the effect of periradicular lesions on the outcome of regenerative endodontic procedures: A prospective clinical study. Clin Oral Investig. 2021;25(2):691-700.
-
Tzanetakis GN, Giannakoulas DG, Papanakou S, Gizani S, Lygidakis N. Regenerative endodontic therapy of immature permanent molars with pulp necrosis: A cases series and a literature review. Eur Arch Paediatr Dent. 2021;22(3):515-525.
-
Zhujiang A, Kim SG. Regenerative endodontic treatment of an immature necrotic molar with arrested root development by using recombinant human platelet-derived growth factor: A case report. J Endod. 2016;42(1):72-5.
-
Cehreli ZC, Erbas Unverdi G, Eymirli P, Mergen I, Arslan E, Esenturk G. Combined conventional and regenerative treatment in molars with coexistent closed and open apices: A case series. Aust Endod J. 2022;48(1):197-201.
-
Yoshpe M, Kaufman AY, Lin S, Ashkenazi M. Regenerative endodontics: A promising tool to promote periapical healing and root maturation of necrotic immature permanent molars with apical periodontitis using platelet-rich fibrin (PRF). Eur Arch Paediatr Dent. 2021;22(3):527-534.
-
Alasqah M, Khan SIR, Alfouzan K, Jamleh A. Regenerative endodontic management of an immature molar using calcium hydroxide and triple antibiotic paste: A two-year follow-up. Case Rep Dent. 2020;10:9025847.
-
Yoshpe M, Ruparel N, Einy S, Ganatra S, & Kaufman AY. Treatment of necrotic anterior and posterior teeth with regenerative endodontic procedures using PRF as a scaffold: a retrospective study. Applied Sciences. 2022;12(13):6774.
Declarations
Scientific Responsibility Statement
The authors declare that they are responsible for the article’s scientific content, including study design, data collection, analysis and interpretation, writing, and some of the main line, or all of the preparation and scientific review of the contents, and approval of the final version of the article.
Animal and Human Rights Statement
All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Funding
None
Conflict of Interest
The authors declare that there is no conflict of interest.
Ethics Declarations
This study was approved by the Ethics Committee of Inonu University Non- Interventional Clinical Research (Date: 2021-11-16, No: 2609)
Data Availability
The datasets used and/or analyzed during the current study are not publicly available due to patient privacy reasons but are available from the corresponding author on reasonable request.
Additional Information
Publisher’s Note
Bayrakol MP remains neutral with regard to jurisdictional and institutional claims.
Rights and Permissions
About This Article
How to Cite This Article
Merve Bilmez Selen, Beril Demircan, Sacide Duman, Pınar Demir, Hatice Aydogdu. Retrospective evaluation of pulp revascularization treatment in immature permanent teeth. Ann Clin Anal Med 2025;16(12):861-866
Publication History
- Received:
- February 17, 2025
- Accepted:
- April 15, 2025
- Published Online:
- April 27, 2025
- Printed:
- December 1, 2025

