The relationship of trunk and hamstring muscle thicknesses with balance and trunk control in patients with acute stroke
The relationship of muscle thicknesses with balance and trunk control
Authors
Abstract
Aim To investigate the relationship of the trunk and hamstring muscle thickness with balance and trunk control using ultrasonography in patients with acute stroke.
Materials and Methods Trunk and hamstring muscle thickness (MT) was measured using ultrasonography. The Trunk Impairment Scale (TIS), functional reach test (FRT), forward and lateral functional reaching in a sitting position, and the Berg Balance Scale (BBS) were used to evaluate trunk balance.
Results Twenty-two patients diagnosed with acute ischemic stroke were included in the study. Significant associations were observed between the following: the thickness of the EO (an abdominal muscle) and paretic side thickness of total abdominal muscles and the BBS, stretches, and the TIS (p=0.039 r=0.442); paretic side thickness of the RA and TrA muscles and the TIS and the BBS (p=0.037 r=0.488); paretic side thickness of the LM muscle and the stretches and the BBS (p=0.049 r=0.424). Among the hamstring muscles, the thickness of the BF muscle’s paretic and non-paretic sides showed a significant correlation with the TIS, the BBS, and the stretches (p=0.037 r=0.447).
Discussion There was a relationship between the trunk muscles RA, TrA, EO, IO, and LM with only the paretic side regarding trunk control and balance in stroke patients. However, in the BF muscle, one of the hamstring muscles, this relationship was found to be on both the paretic and non-paretic sides. While designing rehabilitation programs, we think that it is important to consider this bilateral relationship of the hamstring muscle group with balance and trunk and to include this muscle group in trunk training.
Keywords
Introduction
Stroke is the second leading cause of death worldwide. Postural control and balance ability decrease due to sensory disorders, motor disorders, muscle weakness, and asymmetry resulting from any damage occurring in the central nervous system after stroke [1, 2]. In addition, important structural and metabolic changes occur in skeletal muscles after stroke. Structural adaptive changes in the muscle tissue begin 4 hours after cerebral infarction. These changes may lead to a decrease in the number of motor units related to the impaired synaptic transmission of motor neurons innervating the muscles [3].
Trunk muscles are important both in stabilizing the body in a static state and in maintaining dynamic balance during all functional movements. Changes in trunk position and the weakness of trunk muscles after stroke are important causes of balance disorders in stroke patients [4, 5]. The body parts that control trunk movements on the support surface are the lower extremities. In particular, a relationship is observed between hip extensor, knee extensor, knee flexor, and ankle plane flexor muscle groups and balance [6]. Activating abdominal muscles in stroke patients improves balance and walking ability by increasing muscle thickness [7]. Studies show the relationship between ultrasound, which is commonly used in the literature and reliable in stroke patients, and balance and trunk tests, which are widely used in the clinic and are insufficient in both trunk and lower extremity muscles. This study aimed to determine the relationship between balance and trunk control problems in stroke patients with trunk and hamstring muscle architecture.
Materials and Methods
Participants
Between February 2018 and July 2018, 22 patients diagnosed with ischemic stroke in the Neurology Department of Süleyman Demirel University, Faculty of Medicine, and hospitalized in the Neurology clinic of the hospital were included in the study. This study was single-center, prospective, cross-sectional, and non-blind. Patients who had a stroke for the first time, with acute post-stroke hemiparesis (or plegia), with a static sitting and standing balance for at least 10 seconds, and with a mini- mental state score of at least 24 and above were included. Evaluations were made 3 days after hospitalization. During all tests, one person made the evaluations while the other person ensured the safety of the patient against the risk of falling.
Ultrasonographic evaluation: A high-quality diagnostic B-mode ultrasound device (Aplio 500; Toshiba Medical Systems Corporation, Tochigi-ken, Japan) with a linear transducer in the range of 4-18 MHz was used for measurements. All evaluations were performed bilaterally on the paretic and non-paretic sides, accompanied by the same specialist radiologist and the same physiotherapist. English et al. stated that muscle ultrasound is a reliable method in patients with acute stroke [8].
Measurement of the Muscle Thickness
Transversus Abdominis and Internal and External Oblique: The measurement was made by positioning the probe on the midline between the anterior axillary line, where the middle fibers of TrA and OI can be viewed simultaneously, and the iliac crest and lower rib (Figure1a), [9].
Rectus Abdominis Muscle: The probe was placed 3 cm lateral to the umbilicus, and the measurement was taken at rest (Figure 1b), [10].
Lumbar Multifidus Muscle: With the patient positioned in the prone position, the probe was placed longitudinally in the midline of the L4 spinal process. Then, it was moved slightly laterally and angled medially to obtain an image of the L4-5 zygapophysis joint (Figure 1c), [11].
Hamstring Muscle: The distance between the lateral condyle of the femur and the greater trochanter was measured. A probe was placed to measure the midpoint of this distance [12].
Berg Balance Scale: In this 14-item test, which was made more difficult by reducing the support base, 4 points indicate the ability to complete the task independently, and 0 points indicate the inability to initiate the task [13].
Functional Reach Test: The test evaluates the limits of stability by measuring the maximum distance that the individual can reach forward in a fixed position. It was conducted 3 times, and the score was obtained by taking the average of the last two trials [14].
Forward and Lateral Functional Reach in Sitting Position: In the lateral reach test, the shoulder of the individual sitting on a chair without arm support was abducted by 90°, the elbow was in full extension, and the hand was in a fist position. Patients were asked to reach laterally as far as they could. The distance between the initial state and the final state was recorded. The mean of the last two measurements of the test, which was conducted 3 times, was recorded [15].
Trunk Impairment Scale: Static sitting balance, dynamic sitting balance, and trunk coordination were evaluated in the scale consisting of 17 parameters, and the parameters were scored between 0 and 3 [16].
Statistical Analysis
The IBM SPSS (Statistical Package for Social Sciences for Windows) Statistics 20.0 program was used in the statistical analysis, and any p-value less than 0.05 was accepted as statistically significant. Descriptive values are expressed as mean ± standard deviation. The Shapiro-Wilk test was used to examine the conformity of the data to the normal distribution. The Spearman correlation coefficient was used to examine the relationships between the measurements. According to the definition by Dancey and Reidy, the following classification was made for correlation coefficient (r): r = 0.1–0.3 weak correlation and r = 0.3−0.6 medium correlation [17]. The total sample size was 20 when the ‘power’ was set to 0.95 and the ‘probability of alpha error’ was 0.05 according to the correlation coefficient [4].
Ethical Approval
This research was conducted by the Declaration of Helsinki. This study was approved by the Ethics Committee of Suleyman Demirel University (Date: 2018-01-10, No: 8).
Results
Twenty-two patients were included in the study, and 40.9% of the patients were female. Mostly, the dominant side of the patients was affected (81.8%), and the right lobe was affected in 54.5% of the patients. The clinical characteristics of the individuals are presented in Table 1.
Relationship Between Trunk Muscles and Balance and Trunk Control in Patients with Acute Stroke
A statistically significant correlation was found between the paretic side RA muscle thickness of the patients and the BBS and the dynamic balance, coordination, and total score of the TIS (p=0.15 r=0.512, p=0.027 r=0.472, p=0.037 r=0.488, p=0.021 r=0.488). A statistically significant correlation was only found between the nonparetic side RA muscle thickness and the BBS (p=0.026 r=0.426). A statistically significant correlation was found between the patients’ paretic TrA muscle thickness and their scores in all categories of the BBS and the TIS (p=0.014 r=0.514, p<0.001 r=0.657, p=0.018 r=0.499, p=0.024 r=0.479, p=0.017 r=0.502). A statistically significant correlation was found between the nonparetic TrA muscle thickness and only the static score of the TIS (p=0.012 r=0.526). A statistically significant correlation was found between the paretic EO muscle thickness and the BBS, paretic and nonparetic lateral reach test results, and dynamic balance, coordination, and total score of the TIS (p=0.004 r=0.586, p=0.027 r=0.470, p=0.014 r=0.516, p=0.010 r=0.536, p=0.011 r=0.531, p=0.039 r=0.442, p=0.006 r=0.564). A statistically significant correlation was found between paretic and nonparetic IO muscle thickness and lateral reach on the nonparetic side (p=0.021 r=0.488, p=0.041 r=0.440). A statistically significant correlation was found between paretic side LM muscle thickness and the BBS and bilateral reaches of the patients (p=0.038 r=0.455, p=0.049 r=0.424, p=0.036 r=0.448). (Table 2).
Relationship Between Hamstring Muscles and Balance And Trunk Control in Patients with Acute Stroke
A statistically significant correlation was found between the patient’s paretic BF muscle thickness and overall balance and trunk control (p<0.000 r=0.825, p=0.003 r=0.607, p=0.028 r=0.469, p<0.000 r=0.701, p=0.003 r=0.608, p=0.003 r=0.606, p<0.000 r=0.799, p<0.001 r=0.656, p<0.00o r=0.739). A statistically significant correlation was found between patients’ nonparetic BF muscle thickness and the BBS, FRT, paretic side and non-paretic side reach distances, and all parameters of the TIS (p<0.001 r=0.650, p=0.030 r=0.462, p=0.008 r=0.547, p=0.037 r=0.447, p=0.029 r=0.466, p<0.001 r=0.636, p=0.009 r=0.545, p=0.004 r=0.585). There was no significant relationship between SM and ST muscle thickness and balance parameters (p>0.05) (Table 3).
Discussion
This study was conducted to determine the relationship between trunk and hamstring muscle architecture and trunk control and balance in stroke patients. In patients with acute ischemic stroke, it was found that paretic side thickness of the trunk muscles RA, TrA, EO, and LM and both paretic and nonparetic side thickness of the hamstring muscles, especially BF muscle, were associated with balance and trunk control. Another main result was that the lower extremity muscles showed bilateral relations, while the trunk muscles showed only one-sided relations on the paretic side.
Trunk muscles play an important role in regulating posture and providing balance in movements against gravity, such as sitting and standing, and in movements for reaching [18]. Trunk muscles are very important in performing activities of daily living and ensuring functionality. Therefore, it is important to restore the strength of the trunk and lower extremity muscles to increase the level of independence in post-stroke patients and to adapt them to daily life more quickly.
Karatas et al. stated that the weakness of trunk muscles in unihemispheric stroke patients negatively affected balance, stability, and functionality [5]. The study by Kim et al. showed that BBS, TUG, and trunk control test results in patients with acute stroke were significantly different between the paretic and nonparetic sides [4]. Muscle weakness affects balance negatively, as stated in studies. TrA and IO muscles play an important role in stabilizing the lumbopelvic region and providing functional movement. The contribution of the superficial abdominal muscles (RA, EO, and partially IO) to spine stability is related to their ability to produce moments of flexion, lateral flexion, and rotation, and thus these muscles control external forces by the elongation of the spine in lateral flexion or rotation. TrA, on the other hand, acts as a stabilizer by making postural arrangements before taking action [19]. The TrA muscle, together with IO, increases the internal abdominal pressure and is the first muscle to contract in the lumbar region. Therefore, when movement occurs in the extremities or the trunk, TrA is important in stabilizing the trunk [20]. At the same time, the fact that the EO muscle thickness is associated with the function of lateral reaching towards the paretic and nonparetic side, unlike other muscles, is compatible with the literature.
It was seen in the present study that the TIS, which we used to evaluate trunk control, and the muscle thickness of the TrA, EO, and RA muscles were related. Yoon et al. administered a strengthening program for core muscles with two different training programs, and in both treatments, the TrA, IO, and EO muscle thickness increased, and improvements were observed in BBS as well as the TIS [21].
Trunk stability training has beneficial effects on abdominal muscles, balance, and mobility in stroke patients (7).
Park et al. observed improvements in EO and TrA muscle thickness in healthy individuals to whom they gave core stabilizer muscle strengthening exercises. It was stated that static and dynamic balance increased significantly in the group with changes in the TrA muscle [22]. In our study, it was seen that the TrA muscle, together with the EO muscle, was associated with all parameters of the TIS. In another study conducted on subacute stroke patients, it was found that posterior trunk muscles were significantly associated with trunk balance and ambulatory function after stroke, but there was no significant relationship between anterior trunk muscles and functional ability [23]. This inconsistency with our results suggests that the patients participating in this study were affected by the deteriorated central nervous system before changes in musculature occurred, as they were in the acute phase at the time of assessment.
To determine instability in the sagittal and frontal planes, Slijper et al. analyzed individuals while standing on a stable force platform and an unstable plank. According to the results of the analysis, there was an expected increase in the activity of the tibialis anterior, biceps femoris, erector spinae, and rectus abdominis when standing on an unstable surface [24].
One of the important outcomes of the present study is the necessity of focusing on bilateral approaches, which are thought to contribute to the training of the BF muscle, which plays an active role during sitting, standing up, and standing functions, which are the preparation stage for the patient before walking, in the creation of rehabilitation programs for the lower extremities. While there are no studies in the literature assessing the relationship between BF muscle thickness and functionality, studies are showing that the thickness of the quadriceps muscle, which is one of the lower extremity muscles, has an important role in providing functionality. Nozoe et al. investigated the relationship between daily step count, physical function, and quadriceps muscle thickness in patients with subacute stroke during hospitalization for rehabilitation. Muscle thickness was found to be associated with the level of physical function [25].
Limitations
One of the limitations of the study was that we could only reach patients in the acute phase, as it was a cross-sectional study. Studies with larger samples are needed to make generalizations. The other limitation of the study was the lack of a control group with which we can compare stroke patients with healthy individuals of similar age and characteristics because, in the literature, studies including healthy and stroke patients have reported that the unaffected side is weaker in stroke patients compared to healthy individuals. Therefore, there is a need for studies with a larger patient population and a control group consisting of healthy individuals.
Conclusion
It was found in the present study that trunk control, and balance were related with the RA, TrA, EO, IO, and LM muscles only on the paretic side in stroke patients, while this relationship was with both the paretic and nonparetic side of the hamstring muscles. Studies supporting this relationship are available in the literature. It has also been stated that the training of these muscles has positive effects on balance and that these muscles have an important role in daily life activities. Balance disorders and muscle weakness in post-stroke patients may cause patients to be unable to carry out activities of daily living independently. We think that this bilateral relationship of the BF muscle, one of the hamstring muscles, with balance and the trunk should be taken into consideration, especially during the development of rehabilitation programs for trunk training.
Scientific Responsibility Statement: The authors declare that they are responsible for the article’s scientific content, including study design, data collection, analysis and interpretation, writing, some of the main line, or all of the preparation and scientific review of the contents, and approval of the final version of the article.
Figures
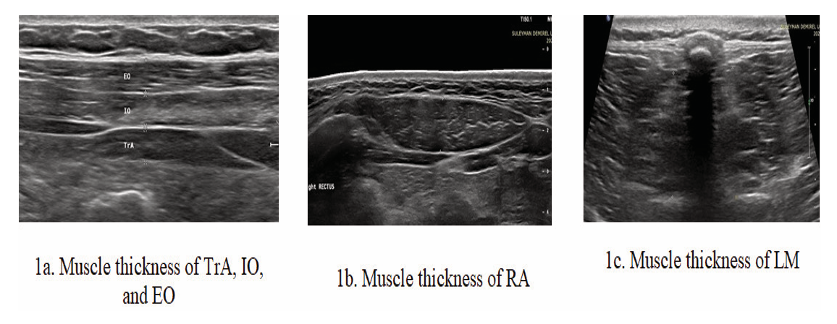
Figure 1. 1a. Muscle thickness of transversus abdominis and internal and external oblique, 1b. Muscle thickness of rectus abdominis, 1c. Muscle thickness of lumbar multifidus
Tables
Table 1. Clinical characteristics
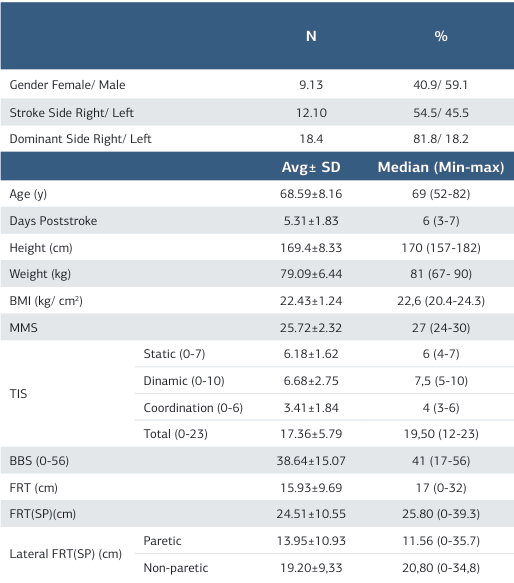
Avg: Average, SD: Standard Deviation, Min: Minimum, Max: Maximum, Cm: Centimeter, Kg: Kilogram, BMI: Body Mass Index, TIS: Trunk Impairment Scale, BBS: Berg Balance Scale, FRT: Functional Reach Test, SP: Sitting Position
Table 2. The relationship of the thickness of the abdominal and lumbar region muscles with balance and trunk control
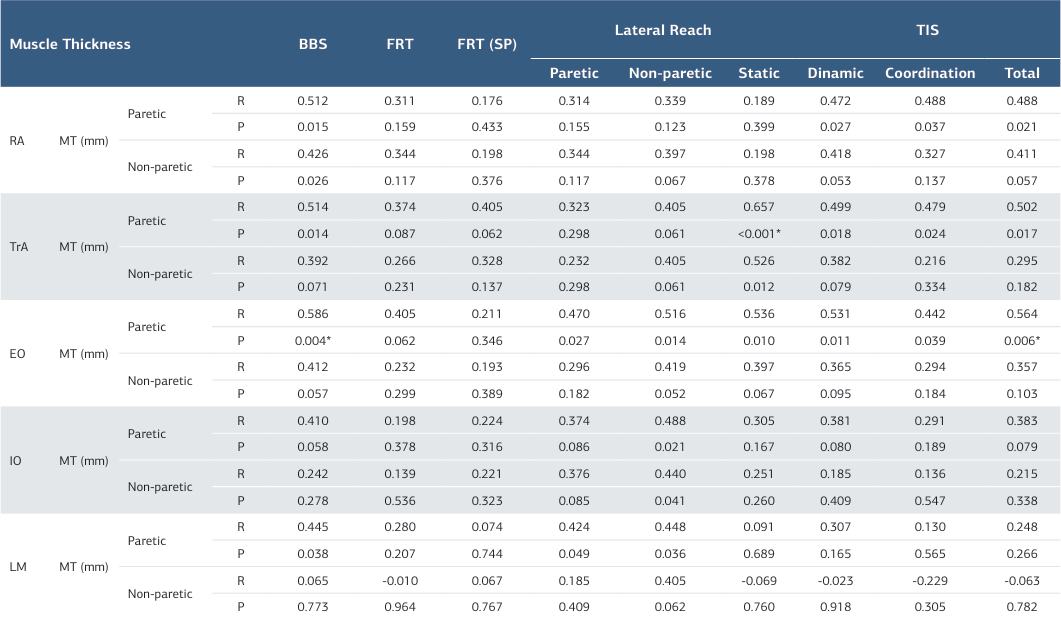
MT: Muscle Thickness, RA: Rectus Abdominis, TrA: Transversus Abdominis, EO: Eksternal Oblique, İO: İnternal Oblique, LM: Lumbal Multifidus, mm: Millimeter, BBS: Berg Balance Scale, FRT: Functional Reach Test, SP: Sitting Position, TIS: Trunk Impairment Scale, p<0,05 * :p<0,01, r: Spearman Correlation
Table 3. MT: Muscle Thickness, RA: Rectus Abdominis, TrA: Transversus Abdominis, EO: Eksternal Oblique, İO: İnternal Oblique, LM: Lumbal Multifidus, mm: Millimeter, BBS: Berg Balance Scale, FRT: Functional Reach Test, SP: Sitting Position, TIS: Trunk Impairment Scale, p<0,05 * :p<0,01, r: Spearman Correlation
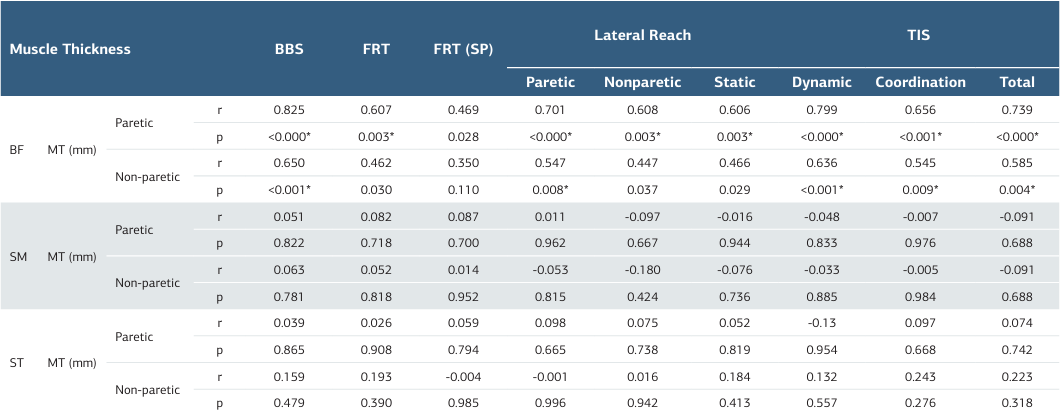
MT: Muscle Thickness, BF: Biceps Femoris, SM: Semimembranous, ST: Semitendinous, mm: Millimeter, BBS: Berg Balance Scale, FRT: Functional Reach Test, SP: Sitting Position, TIS: Trunk Impairment Scale, p<0,05*: p<0,01, r: Spearman Correlation
References
-
Jung K, Kim Y, Chung Y, Hwang S. Weight-shift training improves trunk control, proprioception, and balance in patients with chronic hemiparetic stroke. Tohoku J Exp Med. 2014;232(3):195-9.
-
Feigin VL, Forouzanfar MH, Krishnamurthi R, et al. Global and regional burden of stroke during 1990-2010: findings from the Global Burden of Disease Study 2010. Lancet. 2014;383(9913):245-54.
-
Hafer-Macko CE, Ryan AS, Ivey FM, Macko RF. Skeletal muscle changes after hemiparetic stroke and potential beneficial effects of exercise intervention strategies. J Rehabil Res Dev. 2008;45(2):261-72.
-
Kim Y, Kim J, Nam H, et al. Ultrasound Imaging of the Trunk Muscles in Acute Stroke Patients and Relations With Balance Scales. Ann Rehabil Med. 2020;44(4):273-83.
-
Karatas M, Cetin N, Bayramoglu M, Dilek A. Trunk muscle strength in relation to balance and functional disability in unihemispheric stroke patients. Am J Phys Med Rehabil. 2004;83(2):81-7.
-
Kligyte I, Lundy-Ekman L, Medeiros JM. Relationship between lower extremity muscle strength and dynamic balance in people post-stroke. Med kaunas Lith 2003;39(2): 122-8.
-
Lee J, Jeon J, Lee D, Hong J, Yu J, Kim J. Effect of trunk stabilization exercise on abdominal muscle thickness, balance and gait abilities of patients with hemiplegic stroke: a randomized controlled trial. NeuroRehabilitation. 2020;47 (4):435–42.
-
English CK, Thoirs KA, Fisher L, McLennan H, Bernhardt J. Ultrasound Is a Reliable Measure of Muscle Thickness in Acute Stroke Patients, for Some, but Not All Anatomical Sites: A Study of the Intra-Rater Reliability of Muscle Thickness Measures in Acute Stroke Patients. Ultrasound Med Biol. 2012;38(3):368–76.
-
Teyhen DS, Gill NW, Whittaker JL, Henry SM, Hides JA, Hodges P. Rehabilitative ultrasound imaging of the abdominal muscles. J Orthop Sports Phys Ther. 2007;37(8):450-66.
-
Wilson A, Hides JA, Blizzard L, et al. Measuring ultrasound images of abdominal and lumbar multifidus muscles in older adults: A reliability study. Man Ther. 2015;23:114–9.
-
Stokes M, Rankin G, Newham DJ. Ultrasound imaging of lumbar multifidus muscle: normal reference ranges for measurements and practical guidance on the technique. Man Ther. 2005;10(2):116–26.
-
Abe T, Loenneke JP, Thiebaud RS. Ultrasound Assessment of Hamstring Muscle Size Using Posterior Thigh Muscle Thickness. Clin Physiol Funct Imaging. 2016;36(3): 206-10.
-
Berg K, Wood-Dauphinee S, Williams J. The Balance Scale: reliability assessment with elderly residents and patients with an acute stroke. Scand J Rehabil Med. 1995;27(1):27–36.
-
Duncan PW, Weiner DK, Chandler J SS. Functional reach: a new clinical measure of balance. Journal of Gerontology. 1990;45:192–7.
-
Thompson M, Medley A. Forward and Lateral Sitting Functional Reach in Younger, Middle-aged, and Older Adults. J Geriatr Phys Ther. 2007;30(2):43–8.
-
Verheyden G, Nieuwboer A, Mertin J, Preger R, Kiekens C, De Weerdt W. The Trunk Impairment Scale: A new tool to measure motor impairment of the trunk after stroke. Clin Rehabil. 2004;18(3):326–34.
-
Dancey CP, Reidy J. Statistics without Maths for Psychology, 7th Edition. London: Prentice Hall Pearson. 2007.p.173-76.
-
Karthikbabu S, Chakrapani M, Ganeshan S, Rakshith KC, Nafeez S, Prem V. A review on assessment and treatment of the trunk in stroke: A need or luxury. Neural Regen Res. 2012;7(25):1974–7.
-
Hodges PW. Is there a role for transversus abdominis in lumbopelvic stability ? Man Ther. 1999;4(2):74–86.
-
Cresswell AG, Oddsson L, Thorstensson A. The influence of sudden perturbations on trunk muscle activity and intra-abdominal pressure while standing. Exp Brain Res. 1994;98(2):336-41.
-
Yoon HS, Cha YJ, You JSH. Effects of dynamic core-postural chain stabilization on diaphragm movement, abdominal muscle thickness, and postural control in patients with subacute stroke: A randomized control trial. NeuroRehabilitation. 2020;46(3):381-9.
-
Park M, Yu J, Hong J, Kim J, Jung S, Lee D. Effect of core muscle thickness and static or dynamic balance on prone bridge exercise with sling by shoulder joint angle in healthy adults. J Phys Ther Sci. 2016;28(3):945–50.
-
Suh JH, Lee EC, Kim JS, Yoon SY. Association between trunk core muscle thickness and functional ability in subacute hemiplegic stroke patients: An exploratory cross-sectional study. Topics in Stroke Rehabilitation. 2021;29(3):163-72.
-
Slijper H, Latash M. The effects of instability and additional hand support on anticipatory postural adjustments in leg, trunk, and arm muscles during standing. Exp Brain Res. 2000;135(1):81–93.
-
Nozoe M, Kubo H, Furuichi A, et al. Physical Activity, Physical Function, and Quadriceps Muscle Thickness in Male Patients with Sub-Acute Stroke during Hospitalization: A Pilot Study. Eur Neurol. 2018;80(3-4):157–62.
Declarations
Scientific Responsibility Statement
The authors declare that they are responsible for the article’s scientific content, including study design, data collection, analysis and interpretation, writing, and some of the main line, or all of the preparation and scientific review of the contents, and approval of the final version of the article.
Animal and Human Rights Statement
All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Funding
None
Conflict of Interest
The authors declare that there is no conflict of interest.
Ethics Declarations
This study was approved by the Ethics Committee of Suleyman Demirel University (Date: 2018-01-10, No: 8)
Data Availability
The datasets used and/or analyzed during the current study are not publicly available due to patient privacy reasons but are available from the corresponding author on reasonable request.
Additional Information
Publisher’s Note
Bayrakol MP remains neutral with regard to jurisdictional and institutional claims.
Rights and Permissions
About This Article
How to Cite This Article
Zülal Bekar, Hatice Yakut, Veysel Atilla Yıldız, Süleyman Kutluhan. The relationship of trunk and hamstring muscle thicknesses with balance and trunk control in patients with acute stroke. Ann Clin Anal Med 2025;16(12):839-844
Publication History
- Received:
- May 31, 2025
- Accepted:
- December 16, 2025
- Published Online:
- August 28, 2025
- Printed:
- December 1, 2025

