Postoperative results and complication prediction scoring of immediate allograft-free implant reconstruction surgeries
Complication prediction after breast reconstruction surgery
Authors
Abstract
Aim The aim of this study is to investigate the factors affecting the development of postoperative early complications in patients who underwent immediate implant reconstruction without the use of an allograft for breast cancer.
Methods Female patients who were above the age of 18 and underwent mastectomy and immediately allograft-free implant reconstruction surgeries were included in the research. The study focused on the causes of early complications that occurred within the first 30 days of the patient’s follow-up.
Results A total of 129 breasts were investigated in this study. The postoperative early complication rate was 25.6%. Smoking, malignant pathology, presence of microcalcification, high breast volume, receiving neoadjuvant chemotherapy, and HER-2 negativity for malignant patients were all significant predictors in the development of postoperative early complications. The probability of developing complications is significantly higher in those with 4 or more factor positivity.
Conclusion Correct patient selection is important for skin-sparing surgery and immediate implant reconstruction without the use of allografts, with oncological safety and low cost, and a scoring system is proposed for the first time in this study. Being able to predict postoperative complications in patients at increased risk prevents prolonged hospital stays and delays in adjuvant treatments.
Keywords
Introduction
Breast cancer is a leading cause of malignancy worldwide and the fifth leading cause of cancer-related death 1. A branch of prophylactic treatments for breast cancer is surgical treatments that can be performed with different techniques. Although breast-conserving surgery is the preferred procedure for breast cancer treatment, mastectomies are still a common practice. In recent years, it has been widely recommended, possibly due to successful breast reconstructions 2.
Breast reconstructions can be performed simultaneously or first cancer surgery and then reconstruction surgery with or without nipple-sparing surgery, subpectoral or pre pectoral placement, using allograft or without allograft.. Reconstructions with flaps made using the patient’s tissue (ext. latissimus dorsi flap, deep inferior epigastric artery perforator flap, transverse rectus abdominis muscle flap) or reconstructions using allogeneic materials (implants) or both 3.
Skin-sparing surgery with immediate implant reconstruction is one of the surgical treatment options for breast cancer, and the oncological results of these procedures are successful 4. In immediate implant reconstructions without allografts, early postoperative complication rates were found to be between 19% and 22.1% 5. The use of allografts in reconstruction allows for improved cosmetic results, and there is still controversial data on reducing complications, but it increases the cost, and it is not always possible to obtain these allografts 6. Even without an allograft, these surgeries can be performed safely with the appropriate patient selection.
This study aims to evaluate the postoperative follow-up of patients who underwent immediate subpectoral implant placement without the use of allografts for breast cancer or in patients who underwent prophylactic skin-sparing mastectomy.
Materials and Methods
The study includes mastectomy and immediately allograft- free implant reconstruction surgeries performed in our breast surgery clinic between September 2012 and December 2017. Female patients over the age of 18 who underwent therapeutic or prophylactic skin-sparing mastectomy and immediate reconstruction with a subpectoral placed prosthesis without the use of concomitant allograft were included in the study.
The age of the patient, smoking status, presence of diabetes, indications of surgery (malignancy, prophylaxis), breast volume, breast density, receiving neoadjuvant chemotherapy, surgery type, multifocal-unifocal, lymph node management (axillary dissection absent or present), tumor pathology, receptor status, tumor size, lymph node involvement, chemotherapy and radiotherapy information were evaluated. Family history, the presence of lobular carcinoma in situ, and diffused microcalcification were all indications for prophylactic mastectomy. The presence of associated lobular carcinoma in situ, family history, the aim of building a successful surgical margin, the occurrence of diffused microcalcification, or the patient’s request were all reasons for preferring mastectomy over breast-conserving surgery in patients with malignant diagnoses.
Early postoperative complications were evaluated as seroma, ecchymosis, wound evisceration, and wound necrosis occurring in the first 30 days. Postoperative late complications were evaluated as prosthesis replacement or prosthesis removal because of prolonged early postoperative complications and late wound evisceration-revision surgery after the first 30 days. Surgery Technique
All of the patients in the study had similar surgical procedures and follow-up protocols. All of the patients had skin-sparing surgery. If approved by the surgeon, nipple-sparing surgery was recommended due to the tumor’s location, the suitability of the breast tissue, and the patient’s request. Patients with malignant lymph nodes had sentinel lymph node biopsy, while those with positive lymph nodes had axillary lymph node dissection. The implants were routinely put under the pectoral muscle. Anatomically designed, fixed-volume implants ranging from 185 cc to 650 cc in size were used. All patients had two drains, one in the axillary region and one in the mastectomy lodge. The drains were withdrawn on the second postoperative day at the earliest if the serous drainage was less than 30 cc in one day.
Statistics
All analyses were performed via SPSS version 21(SPSS Inc., Chicago, Illinois). Parametric data were analyzed by independent t-test, and non-parametric data were analyzed by Mann Whitney U Test. Data were presented as mean and standard deviation or median and range. Statistical significance was set at 0.05.
Ethical Approval
This study was approved by the Ethics Committee of Bilkent City Hospital, Ankara, Türkiye (Date: 2021-10-13, No: E2-21- 914).
Results
A total of 129 breasts were investigated in this study, which included 103 patients, 77 of whom had a unilateral mastectomy and 26 of whom had a bilateral mastectomy. The mean age was 44.02±8.33 years for all patients and 43.67 ± 8.69 for the ones with malignant breasts, while the rate of smoking was 24.8% and 21.7%, diabetes mellitus was 7.8% and 7.6%, and family history of malignancy was 17.1% and 10.9%, respectively. In 92 (71.3%) breasts, therapeutic mastectomy was performed due to malignant pathology, while prophylactic mastectomy was performed in 37 (28.7%) breasts. Tumor size was more than 2 cm in 62 breasts (67.4%). Axillary lymph node dissection was performed on 45 breasts (48.9%). Microcalcification was detected in 59 (45.7%) breasts. Patients of 26 (20.2%) breasts received preoperative neoadjuvant chemotherapy, and nipple- sparing surgery was preferred for 28 (21.7%) breasts. Tumor location was periareolar in 32 breasts (24.8%) (Table 1).
The overall complication rate was 32.6%. Early postoperative complication (Figure 1) rate was 25.6% for all breasts, 31.5% for malign breasts, and late complications rates were 11.6% and 9.8%, respectively. Six breasts (4.7%) with early complications had complications in the late period.
The factors that were significant for the development of early complications were smoking (p=0.024 for all and p=0.044 for malign), malignant pathology (p=0.015), presence of microcalcification (p=0.005 for all and p=0.020 for malign), high breast volume (p=0.037 for all and 0.017 for malign), receiving neoadjuvant chemotherapy (p=0.007 for all and p=0.08 for malign), HER-2 negativity for malignant breasts (p=0.049) and axillary lymph node dissection for malignant breasts (p=0.031) (Table 2).
Multivariate regression analysis showed a correlation between the early postoperative complications and 6 parameters in all and malignant breasts, including breast volume (p=0.041 and 0.013, respectively), smoking (p=0.006 and 0.012, respectively), presence of microcalcification (p=0.013 and 0.017, respectively), neoadjuvant chemotherapy (p=0.019 and 0.027, respectively), malignant pathology (p=0.045 for all) and HER-2 negativity (p=0.025 for malignant). Patients were given 1 point for each positive parameter and scored between 0 and 6. ROC curve was made for breast volume, and 1 point was given to those with 4 and above (Table 3).
The probability of developing complications was found to be significantly higher in patients with a score of 4 and above (p<0.001, AUC: 0.794, specificity: 88.50%, sensitivity: 57.7%). The average hospital stay was 7.12 ± 3.02 days. The hospital stay was 5.74±1.56 days for the patients without complications and 11.09 ±2.07 days for the patients with early complications, and hence, the hospital stay was statistically longer for patients with complications (p<0.001).
Discussion
Skin-sparing surgery and simultaneous reconstruction are frequently used in the treatment of breast cancer because of their oncologically safe and cosmetically satisfactory results 4. The cosmetic success of the surgery is higher, and the postoperative capsular contraction rate is lower when an allograft is used in breast reconstruction, but there is a higher risk of infection 6. Despite the possibility of postoperative complications, it is a frequently preferred application 6. However, the cost of the surgery is higher, and access to the material is not always possible. In implant reconstructions performed after mastectomy in our clinic, the implant is placed directly under the muscle in patients with small breast volume. The pectoralis major muscle is cut, and the support sutures are placed after the implant is placed in the formed pouch for medium and large breasts. In addition, it may be necessary to technically cut the pectoral muscle for successful cosmetic results and support the implants with a suture during the placement of the implants, which increases the risk of complications. It is important to choose the patient group carefully and correctly while performing surgery with limited opportunities.
According to the literature, the total complication rate was found to be 20.5% to 31.4% 7,8,9. We found the total complication rate at 32.6%, similar to the literature. There are many publications in the literature showing a significant relationship between breast volume or size increase and postoperative complications 7,10,11. In our study, the mean breast volume was 1716.48 ± 969.35 cm3. It was measured as a 2019.38 ± 1086.71 cm3 in patients with complications and 1612.36± 908.53 cm3 in patients who did not develop complications, and it was statistically significant.
Smoking negatively affects wound healing, with decreased tissue oxygenation and decreased inflammatory response, and causes complications in breast reconstructions 12,13. In our study, smoking was statistically associated with early complications. Many studies reported an association between breast cancer and microcalcifications 14,15. However, the relationship between microcalcification and the complication rate has not been reported. In our study, a significant association was found between the early complications and the presence of microcalcification.
Reconstruction of the breast post neoadjuvant chemotherapy is mostly done applying implant-based procedures 16. Neoadjuvant chemotherapy impairs wound healing due to its cytotoxic effect 17. However, this cytotoxicity and negative effect on wound healing may disappear when the appropriate time passes before surgical treatment after neoadjuvant 18. In our study, neoadjuvant chemotherapy and early postoperative complications were significantly associated.
Joy et al. 19 found no significant relationship between axillary lymph node dissection and wound complications in implant- based reconstruction. In the study of Madsen et al. 20 on 270 breasts that underwent immediate implant reconstruction after mastectomy, axillary lymph node dissection was found to be an independent risk factor for complications. Verma et al. 21 reported a total of 20.6% complications in 467 breasts that underwent immediate breast reconstruction, while complications were observed in 36.4% of breasts that underwent axillary lymph node dissection, which was statistically significant. The cause of the complication appeared to be related to the increased development of seroma 22. We found a significant relationship between axillary dissection and early postoperative complications according to univariate analyses; however, it was not an independent risk factor for early complications.
Since the Ki-67 proliferation index result was not present in all patients, molecular subtyping could not be performed, so we compared breasts for receptor status. Studies analyzing the association of complications between pathological characteristics in malignant breasts showed no such relationship 11,22. In our study, the complication rate was strongly correlated with HER-2 negativity but not with ER or PR status for malignant breasts. Although HER-2 negativity was an independent risk factor for early complications, accompanying neoadjuvant chemotherapy may have affected these results. Local recurrence rates after breast-conserving surgery are 6.2% to 3.1% in the literature 23,24,25. In our study, the mean follow-up time was 73.21 months, and acceptable rates were seen.
According to the 6-point score system, which we recommend for the first time in the literature, the rate of developing early postoperative complications in patients with a score of 4 and above was found to be significantly higher.
Limitations
This study’s primary limitation is that it was performed retrospectively. Prospectively designed studies with a considerable patient population need to be conducted.
Conclusion
We showed that the complication rate was higher in high breast volume, smokers, microcalcification, neoadjuvant chemotherapy, malignant pathology, and HER-2 negativity with malignant breasts. High complication rates increase the length of hospital stay, resulting in increased costs and a delay in the initiation of possible adjuvant therapies. However, it is seen that there are acceptable local recurrence, metastasis, and death rates. Therefore, these surgeries are safe and feasible, especially in countries with limited access to the material, which costs less as no extra material is required.
Figures

Figure 1. Early complications in breasts. a: Necrosis, b: Wound evisceration
Tables
Table 1. Patients’ clinical, surgical, pathological, and follow-up findings
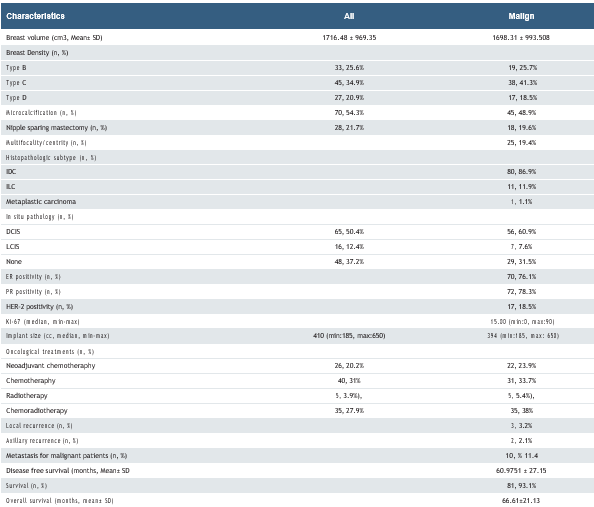
DCIS: ductal carcinoma in situ, LCIS: lobular carcinoma in situ, IDC: invasive ductal carcinoma, ILC: invasive lobular carcinoma, ER: estrogen receptor, PR: progesterone receptor
Table 2. Patient, surgical, and tumor characteristics by early postoperative complications
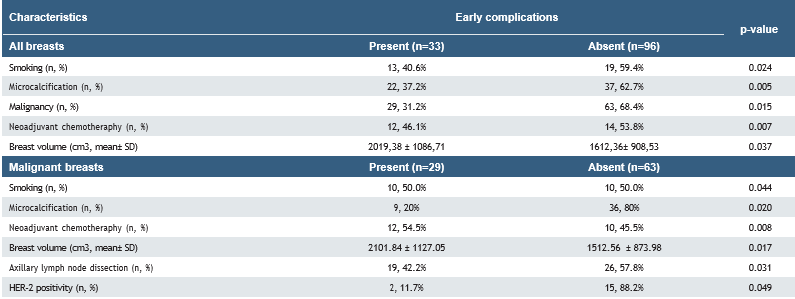
DCIS: ductal carcinoma in situ, LCIS: lobular carcinoma in situ, IDC: invasive ductal carcinoma, ILC: invasive lobular carcinoma, ER: estrogen receptor, PR: progesterone receptor.
Table 3. Scoring system for early complications of implant reconstruction surgery without emergency allograft
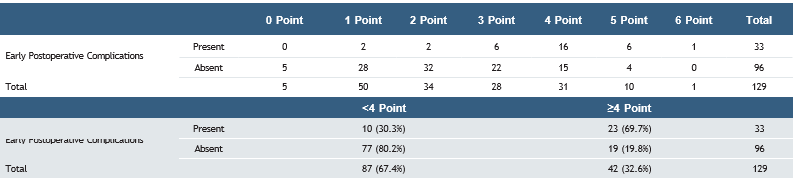
p<0.001; Positive likelihood ratio= 8.69; Negative likelihood ratio=0.511
References
-
Sung H, Ferlay J, Siegel RL, et al. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J Clin. 2021;71(3):209-49.
-
Kummerow KL, Du L, Penson DF, Shyr Y, Hooks MA. Nationwide trends in mastectomy for early-stage breast cancer. JAMA Surg. 2015;150(1):9–16.
-
Gerber B, Marx M, Untch M, Faridi A. Breast reconstruction following cancer treatment. Dtsch Arztebl Int. 2015;112(35-36):593-600.
-
Galimberti V, Vicini E, Corso G, et al. Nipple-sparing and skin-sparing mastectomy: Review of aims, oncological safety and contraindications. Breast. 2017;34Suppl1(Suppl 1):S82-S84.
-
Su CL, Yang JR, Kuo WL, Chen SC, Cheong DC, Huang JJ. Direct-to-implant breast reconstruction following nipple-sparing mastectomy: Predictive factors of adverse surgical outcomes in Asian patients. Arch Plast Surg. 2021;48(5):483-93.
-
Gravina PR, Pettit RW, Davis MJ, Winocour SJ, Selber JC. Evidence for the use of acellular dermal matrix in implant-based breast reconstruction. Semin Plast Surg. 2019;33(4):229-35.
-
Quilichini O, Barrou J, Bannier M, et al. Mastectomy with immediate breast reconstruction: Results of a mono-centric 4-year cohort. Ann Med Surg. 2021;61:172-9.
-
Muller T, Baratte A, Bruant-Rodier C, Bodin F, Mathelin C. Oncological safety of nipple-sparing prophylactic mastectomy: A review of the literature on 3716 cases. Ann Chir Plast Esthet. 2018;63(3):e6-e13.
-
Besler E, Harmancıoğlu Ö. Examination of the effects of celecoxib on postmastectomy seroma and wound healing. Med Bull Sisli Etfal Hosp. 2018; 52(3):212-9.
-
Frey JD, Salibian AA, Karp NS, Choi M. The impact of mastectomy weight on reconstructive trends and outcomes in nipple-sparing mastectomy. Plast Reconst Surg. 2018;141(6):795e–804e.
-
Ito H, Ueno T, Suga H, et al. Risk factors for skin flap necrosis in breast cancer patients treated with mastectomy followed by immediate breast reconstruction. World J Surg. 2019;43(3):846-52.
-
Sørensen LT. Wound healing and infection in surgery. The clinical impact of smoking and smoking cessation: A systematic review and meta-analysis. Arch Surg. 2012;147(4):373-83.
-
Thorarinsson A, Fröjd V, Kölby L, Lidén M, Elander A, Mark H. Patient determinants as independent risk factors for postoperative complications of breast reconstruction. Gland Surg. 2017;6(4):355-67.
-
Azam S, Eriksson M, Sjölander A, et al. Mammographic microcalcifications and risk of breast cancer. Br J Cancer. 2021;125(5):759–65.
-
Alsheh Ali M, Czene K, Hall P, Humphreys K. Association of microcalcification clusters with short-term invasive breast cancer risk and breast cancer risk factors. Sci Rep. 2019;9(1):14604.
-
Citgez B, Yigit B, Yetkin SG. Management of the axilla and the breast after neoadjuvant chemotherapy in patients with breast cancer: A systematic review. Med Bull Sisli Etfal Hosp. 2021;55(2):156-61.
-
Frey JD, Choi M, Karp NS. The effect of neoadjuvant chemotherapy compared to adjuvant chemotherapy in healing after nipple-sparing mastectomy. Plast Reconstr Surg. 2017;139(1):10e-19e.
-
Bartholomew AJ, Dervishaj OA, Sosin M, et al. Neoadjuvant chemotherapy and nipple-sparing mastectomy: Timing and postoperative complications. Ann Surg Oncol. 2019;26(9):2768-72.
-
Joy MT, Rich MD, Moyer KE. Axillary lymphadenectomy and wound complications in implant-based breast reconstruction. Ann Plast Surg. 2018;81(3):280–3.
-
Madsen RJ, Esmonde NO, Ramsey KL, Hansen JE. Axillary lymph node dissection is a risk factor for major complications after immediate breast reconstruction. Ann Plastic Surg. 2016:77(5):513–6.
-
Verma R, Klein G, Dagum A, Khan S, Bui DT. The effect of axillary lymph node sampling during mastectomy on immediate alloplastic breast reconstruction complications. Plast Reconstr Surg Glob Open. 2019;7(5):e2224.
-
Siegel EL, Whiting J, Kim Y, Sun W, Laronga C, Lee MC. Effect of surgical complications on outcomes in breast cancer patients treated with mastectomy and immediate reconstruction. Breast Cancer Res Treat. 2021;188(3):641–8.
-
Lanitis S, Tekkis PP, Sgourakis G, Dimopoulos N, Al-Mufti R, Hadjiminas DJ. Comparison of skin-sparing mastectomy versus non-skin-sparing mastectomy for breast cancer: A meta-analysis of observational studies. Ann Surg. 2010;251(4):632-9.
-
Fujihara M, Yamasaki R, Ito M, et al. Risk factors of local recurrence following implant-based breast reconstruction in breast cancer patients. BMC Women’s Health. 2021;21(1):147.
-
Joo JH, Ki Y, Kim W, et al. Pattern of local recurrence after mastectomy and reconstruction in breast cancer patients: A systematic review. Gland Surg. 2021;10(6):2037-46.
Declarations
Scientific Responsibility Statement
The authors declare that they are responsible for the article’s scientific content including study design, data collection, analysis and interpretation, writing, some of the main line, or all of the preparation and scientific review of the contents and approval of the final version of the article.
Animal and Human Rights Statement
All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Funding
None
Conflict of Interest
The authors declare that there is no conflict of interest.
Ethics Declarations
This study was approved by the Ethics Committee of Bilkent City Hospital (Date: 2021-10-13, No: E2-21-914)
Data Availability
The data supporting the findings of this article are available from the corresponding author upon reasonable request, due to privacy and ethical restrictions. The corresponding author has committed to share the de-identified data with qualified researchers after confirmation of the necessary ethical or institutional approvals. Requests for data access should be directed to bmp.eqco@gmail.com
Additional Information
Publisher’s Note
Bayrakol MP remains neutral with regard to jurisdictional and institutional claims.
Rights and Permissions
About This Article
How to Cite This Article
Hikmet Pehlevan Özel, Nermin Damla Okay, İbrahim Ağaçkıran, Buket Altun Özdemır, Ebru Menekşe. Postoperative results and complication prediction scoring of immediate allograft-free implant reconstruction surgeries. Ann Clin Anal Med 2025; DOI: 10.4328/ACAM.22584
Publication History
- Received:
- January 27, 2025
- Accepted:
- March 3, 2025
- Published Online:
- April 11, 2025
- Printed:
- November 1, 2025

