The role of inflammation in pregnancy loss: Changes in systemic immune- inflammation index in patients with missed abortion
Systemic inflammation in missed abortion
Authors
Abstract
Aim A missed abortion occurs when there is a lack of uterine expulsion and cessation of the fetal heartbeat within the first 20 weeks of pregnancy. This retrospective study aimed to assess the predictive value of the Systemic Immune-Inflammation Index (SII), neutrophil-to-lymphocyte ratio (NLR), and platelet- to-lymphocyte ratio (PLR) for missed abortion by analyzing the complete blood count (CBC) parameters in affected women.
Methods This retrospective analysis involved 108 pregnant women diagnosed with missed abortions. CBC results collected at the time of diagnosis and during routine check-ups before the diagnosis were analyzed. White blood cell (WBC), platelet, neutrophil, and lymphocyte counts were recorded, and PLR, NLR, and SII (Neutrophil x Platelet/Lymphocyte) values were calculated. Statistical analyses were conducted to assess differences between these time points.
Results NLR and SII values were significantly elevated at the time of missed abortion diagnosis (p < 0.05). However, no statistically notable difference in PLR values (p > 0.05) existed.
Conclusion These findings indicate that inflammation is a key factor in the pathophysiology of missed abortion. This study provides valuable insights into the temporal effects of inflammation by comparing inflammatory markers before and at the time of diagnosis within the same patient cohort. This study could aid in the creation of new approaches for preventing and managing pregnancy loss.
Keywords
Introduction
Missed abortion is a type of loss that occurs in the early stages of pregnancy and is characterized by the lack of spontaneous expulsion from the uterus, despite the intrauterine death of the embryo or fetus. Although the etiology of early pregnancy loss remains incompletely understood, it is thought that various factors, including genetic anomalies, placental insufficiency, endocrine factors, immunological processes, and inflammation are believed to contribute to the development of this condition 1.
During pregnancy, the delicate balance between proinflammatory and anti-inflammatory effects is critical for optimal maternal and fetal health. T helper cells play a crucial role in the complex interaction between fetal and maternal tissues during embryonic implantation, inducing the release of various growth factors and cytokines that support the healthy development of the embryo and placenta during this phase 2. This contributes to normal placental development and the maintenance of fetal health. With the initiation of the placentation, trophoblast cells modulate the immune system, establishing immune tolerance at the maternal-fetal interface. Compared to healthy pregnancies, differences in the levels of various proinflammatory and anti-inflammatory cytokines have been detected in cases of pregnancy loss 3. However, the use of these markers in routine clinical practice remains limited.
SII (Systemic Immune-Inflammatory Index), NLR (Neutrophil/Lymphocyte Ratio), and PLR (Platelet/Lymphocyte Ratio) are cost-effective and easily accessible biomarkers that reflect inflammatory response and immune system activation. These parameters are utilized to assess the diagnosis, outcome, and treatment effectiveness of various conditions. Systemic inflammatory markers, including SII, NLR, and PLR, have emerged as crucial biomarkers for both diagnosis and prognosis in a range of conditions, including malignancies 4,5, cardiovascular diseases 6, and inflammatory diseases 7. Elevated levels of these markers are often indicative of poor prognosis in several solid tumors, such as colorectal 8, breast 9, lung 10, and gastric 11 cancers. Furthermore, inflammation plays a significant role in the progression of hematological malignancies 12. Specifically, SII has been identified as an independent predictor of mortality in patients with peripheral arterial disease 13. Likewise, elevated SII values have been linked to increased mortality risk in COVID-19 patients 14.
Pregnancy is a complex process that induces transformations in maternal physiology and the immune system. These adaptations play a critical role in supporting embryo implantation and development, as well as maintaining maternal immune tolerance. However, this homeostatic balance may be disrupted in the presence of threatened abortion. Given the potential adverse effects of an increased inflammatory response on fetal development, it is believed that the risk of miscarriage may rise. However, it remains unclear whether miscarriage is a cause or a consequence of the inflammatory response. Regarding pregnancy-related complications, SII, NLR, and PLR are considered potential biomarkers for predicting obstetric conditions such as pre-eclampsia 15, preterm labor risk 16, and abortion 17. Therefore, biomarkers like SII, NLR, and PLR have significant clinical value in both assessing systemic inflammation and facilitating the early diagnosis and prediction of various diseases. Nevertheless, there is insufficient evidence on the association of these parameters with missed abortion. Evaluating the inflammatory response in women experiencing missed abortion may provide valuable insights into the etiopathogenesis of this condition and aid in developing clinical management strategies. This study aimed to investigate whether indicators such as SII, NLR, and PLR are associated with the development of missed abortion and to explore whether these parameters could be integrated into clinical practice.
Materials and Methods
This retrospective study analyzed data from 108 pregnant women diagnosed with missed abortions between 2021 and 2025.
The study included women aged 18 years and older who had been diagnosed with missed abortion between 7-12 weeks of gestation. Women who had a detectable fetal heartbeat at the first pregnancy control were asymptomatic and had no systemic diseases that could affect the blood count were included in the study. Pregnancies in which the fetal heartbeat disappeared during the follow-up period were analyzed. Patients with missing data, multiple pregnancies, a history of hematological or inflammatory disorders, active infections, thrombosis or anticoagulant use, fever of unknown origin, and recurrent miscarriages were not included in the study.
Complete blood count (CBC) results at the time of diagnosis and during routine examinations before diagnosis were analyzed. White blood cell (WBC), neutrophil, lymphocyte, and platelet counts, as well as inflammatory markers such as NLR (Neutrophil/Lymphocyte Ratio), PLR (Platelet/Lymphocyte Ratio), and SII (Neutrophil x Platelet/Lymphocyte), were calculated, and statistical analyses were performed.
Statistical Analyses
Statistical analyses were performed using the SPSS software (IBM SPSS Statistics 27). Frequency tables and descriptive statistics were used to interpret the findings. For measurement values that followed a normal distribution, parametric methods were applied. In accordance with parametric methods, the “Paired Sample” test (t-table value) was used to compare the measurement values of two dependent groups. For measurement values that did not follow a normal distribution, non-parametric methods were used. In accordance with non-parametric methods, the “Wilcoxon” test (Z-table value) was employed to compare the measurement values of two dependent groups.
Ethical Approval
The study was approved by the Ethics Committee of Kırıkkale University (Date: 2025-02-26, No: 2025.02.26).
Results
A total of 108 pregnant women participated in the study. SII, NLR, and PLR values were calculated from hemogram parameters at the time of diagnosis and prior to diagnosis in patients diagnosed with missed abortion. The distribution of these variables is presented in Table 1. The mean age of the patients was 30.00 ± 6.75 (years), the mean gestational week was 8.3 ± 1.2, and the mean parity was 1.19 ± 1.13. The study revealed a statistically significant difference between NLR, SII, WBC, neutrophil, and lymphocyte values before and at the time of diagnosis (p < 0.05). WBC, neutrophil, NLR, and SII values at the time of diagnosis were found to be significantly higher than pre-diagnosis values (p < 0.05). There was no statistically significant difference in hemoglobin, platelet, and PLR values before and at the time of diagnosis (p > 0.05). The results of the analyses are presented in Table 2.
Discussion
Although the etiopathogenesis of missed abortion has not been fully elucidated, it is believed that inflammation could have a significant impact in addition to genetic, endocrine, and immunological factors. Pregnancy is considered a unique immunological process and inflammatory events are known to play critical roles in different stages, such as implantation (inflammation), gestation (anti-inflammation), and delivery (inflammation). In this process, natural killer (NK) cells, activated by ovarian hormones, have important functions during pregnancy. Particularly in the first trimester, NK cells, which constitute a significant portion (50% to 70%) of decidual lymphocytes, secrete cytokines and chemokines that support tissue remodeling, trophoblast invasion, embryonic development, and placentation 18. Therefore, a dysfunction in the function of decidual NK (NK) cells may lead to inadequate trophoblast invasion, placentation defects, and consequently, missed abortion.
In this study, it was found that WBC, neutrophil, NLR and SII values among inflammatory markers were markedly higher in pregnant women with missed abortion, while PLR showed no statistically significant difference. The study results provide evidence for the potential role of inflammation in pregnancies ending in missed abortion. Previous research has typically compared missed abortion patients with healthy pregnant women. This study is one of the first to compare inflammatory markers before and at diagnosis in the same patient group. This approach provides valuable insights into understanding the effect of inflammation on the development of missed abortion over time.
Studies examining the relationship between inflammatory markers and pregnancy loss have increased in recent years. Neutrophils are an essential component of the inflammatory response, and their increase is considered an indicator of systemic inflammation. Similarly, hematological indices like SII and NLR indicate the extent of systemic inflammation. An increase in SII level typically correlates with an increase in platelet count, a decrease in lymphocyte count, and an increase in neutrophil count, all of which occur as part of the body’s immune response to inflammation. These parameters were found to be statistically significantly higher in the missed abortion group within our study, a finding that supports the hypothesis that inflammation may be involved in the development of this clinical condition.
According to Turgut et al., elevated SII values in early pregnancy may represent a valuable additional marker for predicting miscarriage in women with threatened miscarriage 19. A number of studies have consistently reported elevated NLR biomarker levels in women experiencing missed abortion compared to healthy pregnant controls 20,21,22. However, a review of the literature on missed abortion reveals differences in findings. For instance, studies by Ata and Liu found no significant difference in NLR between missed abortions and healthy pregnant patients 23,24. This heterogeneity is thought to arise because missed abortion can result from various etiological factors, and inflammatory responses and immune tolerance can change during pregnancy.
The fact that PLR values did not show a significant difference in our study suggests that inflammation in missed abortion is primarily neutrophil-mediated, with platelets not being significantly affected by the process. Although PLR has been reported in the literature as an important biomarker for determining inflammation and thrombotic processes, its relationship with pregnancy complications has not been consistently demonstrated. While an increase in PLR values was reported in cases of early pregnancy loss 21,23, no significant difference was observed in other studies 20,24. A systematic review and meta-analysis reported that NLR biomarker levels were significantly higher in women with recurrent pregnancy loss; however, no significant relationship was found between PLR and pregnancy loss 25. The unchanged PLR in our study may be due to platelets remaining stable and no significant change in lymphocyte count.
Further studies on the PLR biomarker in patients with a history of recurrent pregnancy loss (RPL) and mutations in the thrombophilia panel could offer significant benefits for risk stratification and the design of tailored treatment approaches for placental microthrombosis and impaired spiral artery remodeling. Therefore, additional studies in larger patient populations are required to gain a better understanding of the association between inflammatory markers and missed abortion, as well as their potential for clinical use.
Limitations
The study has some limitations. Due to the retrospective design, we could only establish a correlation between inflammation and missed abortion, and prospective studies are needed to determine a causal relationship.
Furthermore, because the participants’ examination frequency was not standardized, changes in CBC parameters occurred at different time intervals, which may have influenced the results. The contradictory findings in the literature, along with the results of our study, highlight that missed abortion is a complex and multifactorial condition. In particular, the heterogeneity in inflammatory markers emphasizes the role of different etiological factors and individual immune responses. In future studies, evaluating different inflammatory markers (e.g., cytokines, chemokines) in larger patient groups may help to elucidate the inflammatory processes associated with missed abortion more comprehensively. Furthermore, investigating the potential role of therapeutic strategies targeting inflammation (e.g., anti-inflammatory drugs, immunotherapy) in reducing the risk of missed abortion is also worthwhile. Such research may advance our understanding of pregnancy loss and facilitate the development of novel preventative and therapeutic interventions.
Conclusion
The main strength of our study is that both CBC measurements were obtained from the same cohort. This reduced variance by minimizing the influence of variables such as interindividual physiological differences, genetic predispositions, and environmental factors. For example, while each individual’s basal inflammation level may differ, consecutive measurements in the same individual eliminate this variability, thereby increasing statistical power.
Tables
Table 1. Demographic data of cases

Table 2. Comparison of study-related quantitative parameters of the patients before and during the diagnosis
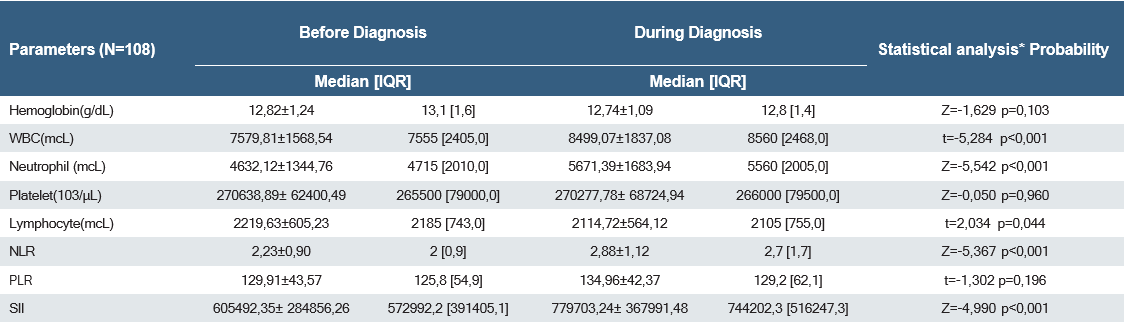
*‘Paired Sample’ test (t-table value) statistics were used to compare the measurement values of two dependent groups for normally distributed data. ‘Wilcoxon’ test (Z-table value) statistics were used to compare the measurement values of two dependent groups in non-normally distributed data
References
-
Turesheva A, Aimagambetova G, Ukybassova T, et al. Recurrent pregnancy loss etiology, risk factors, diagnosis, and management: fresh look into a full box. J Clin Med. 2023;12(12):4074.
-
Graham JJ, Longhi MS, Heneghan MA. T helper cell immunity in pregnancy and influence on autoimmune disease progression. J Autoimmun. 2021;121:102651.
-
Yang X, Tian Y, Zheng L, Luu T, Kwak-Kim J. The update immune-regulatory role of pro- and anti-inflammatory cytokines in recurrent pregnancy losses. Int J Mol Sci. 2022;24(1):132.
-
Mao H, Yang F. Prognostic significance of systemic immune-inflammation index in patients with ovarian cancer: a meta-analysis. Front Oncol. 2023;13:1193962.
-
Yang X, Wu C. Systemic immune-inflammation index and gastric cancer prognosis: a systematic review and meta-analysis. Exp Ther Med. 2024;27(3):122.
-
Ye Z, Hu T, Wang J, et al. Systemic immune-inflammation index as a potential biomarker of cardiovascular diseases: A systematic review and meta-analysis. Front Cardiovasc Med. 2022;9:933913.
-
Dervisevic A, Fajkic A, Jahic E, et al. Systemic immune-inflammation index in evaluation of inflammation in rheumatoid arthritis patients. Medeni Med J. 2024;39(3):183-91.
-
Passardi A, Scarpi E, Cavanna L, et al. Inflammatory indexes as predictors of prognosis and bevacizumab efficacy in patients with metastatic colorectal cancer. Oncotarget. 2016;7(22):33210-9.
-
Zhu M, Chen L, Kong X, et al. The systemic immune-inflammation index is an independent predictor of survival in breast cancer patients. Cancer Manag Res. 2022;14:775-820.
-
Küçük A, Öztep Ş, Yılmaz E, Topkan E. The effect of systemic immune- inflammation index on survival before concurrent chemoradiotherapy in patients diagnosed with limited-stage small cell lung cancer. Mersin Univ Saglık Bilim Derg. 2021;14(2):186-98.
-
Chen L, Yan Y, Zhu L, et al. Systemic immune-inflammation index as a useful prognostic indicator predicts survival in patients with advanced gastric cancer treated with neoadjuvant chemotherapy. Cancer Manag Res. 2017;9:849-67.
-
Hai T, Wu W, Ren K, Li N, Zou L. Prognostic significance of the systemic immune-inflammation index in patients with extranodal natural killer/T-cell lymphoma. Front Oncol. 2023;13:1273504.
-
Dural İE, Yalım Z, Aksu U, Özgeyik M, Gökaslan S, Yılmaz ÖF. Effect of systemic immune-inflammation index on mortality in patients wıth peripheral artery disease. Kocatepe Tip Derg. 2025;26(1):28-32.
-
Karaaslan T, & Karaaslan E. Predictive value of systemic immune- inflammation index in determining mortality in COVID-19 Patients. J Crit Care Med (Targu Mures). 2022;8(3):156-64.
-
Kapci M, Sener K, Cakir A, Altug E, Guven R, Avci A. Prognostic value of systemic immune-inflammation index in the diagnosis of preeclampsia. Heliyon. 2024;10(6):e28181.
-
Sert ZS & Bülbül R. Predictive value of systemic immune-inflammation index in patients with preterm labor. Cukurova Med J. 2022;47(2):697-703.
-
Soysal C, Sarı H, Işıkalan MM, et al. Role of the systemic immune- inflammation index in threatened abortion patients and predicting of abortion. J Obstet Gynaecol Res. 2023;49(7):1723-8.
-
Zhang X, Wei H. Role of decidual natural killer cells in human pregnancy and related pregnancy complications. Front Immunol. 2021;12:728291.
-
Turgut E, Yildirim M, Sakcak B, Ayhan SG, Tekin OM, Sahin D. Predicting miscarriage using systemic immune-inflammation index. J Obstet Gynaecol Res. 2022;48(3):587-92.
-
Kale İ, Helvacıoğlu Ç, Muğurtay TE. Evaluation of complete blood count parameters in the first trimester: an early indicator of miscarriage. J Clin Invest Surg. 2021;6(1):48-52.
-
Biyik I, Albayrak M, & Keskin F. Platelet to lymphocyte ratio and neutrophil to lymphocyte ratio in missed abortion. Rev Bras Ginecol Obstet. 2020;42(05):235- 9.
-
Uçkan K, Çeleğen İ, Baskiran Y, & Hanligil E. Can platelet mass index be used as a prognostic marker in the diagnosis of missed abortion patients? Eastern J Med. 2022;27(4):627-33.
-
Ata N, Kulhan M, Kulhan NG, Turkler C. Can neutrophil-lymphocyte and platelet-lymphocyte ratios predict threatened abortion and early pregnancy loss? Ginekol Pol. 2020;91(4):210-5.
-
Liu D, Huang X, Xu Z, Chen M, Wu M. Predictive value of NLR and PLR in missed miscarriage. J Clin Lab Anal. 2022;36(3):e24250.
-
Hantoushzadeh S, Gargar OK, Jafarabady K, et al. Diagnostic value of neutrophil-to-lymphocyte and platelet-to-lymphocyte ratio to predict recurrent pregnancy loss and abortion; a systematic review and meta-analysis. Immun Inflamm Dis. 2024;12(3):e1210.
Declarations
Scientific Responsibility Statement
The authors declare that they are responsible for the article’s scientific content, including study design, data collection, analysis and interpretation, writing, and some of the main line, or all of the preparation and scientific review of the contents, and approval of the final version of the article.
Animal and Human Rights Statement
All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Funding
None
Conflict of Interest
The authors declare that there is no conflict of interest.
Ethics Declarations
This study was approved by the Ethics Committee of Kırıkkale University (Date: 2025-02-26, No: 2025.02.26)
Data Availability
The data supporting the findings of this article are available from the corresponding author upon reasonable request, due to privacy and ethical restrictions. The corresponding author has committed to share the de-identified data with qualified researchers after confirmation of the necessary ethical or institutional approvals. Requests for data access should be directed to bmp.eqco@gmail.com
Additional Information
Publisher’s Note
Bayrakol MP remains neutral with regard to jurisdictional and institutional claims.
Rights and Permissions
About This Article
How to Cite This Article
Yagmur Soykan, The role of inflammation in pregnancy loss: Changes in systemic immune-inflammation index in patients with missed abortion Ann Clin Anal Med 2025; DOI: 10.4328/ACAM.22637
Publication History
- Received:
- March 8, 2025
- Accepted:
- April 15, 2025
- Published Online:
- April 25, 2025
- Printed:
- November 1, 2025

