The diagnostic and prognostic value of BUN/albumin and BUN/creatinine ratios in patients with gastrointestinal bleeding presenting to the emergency department
Prognostic value of BUN/albumin and BUN/creatinine ratios in gib
Authors
Abstract
Aim This study aimed to investigate the diagnostic value of blood urea nitrogen-to-albumin (B/A) and blood urea nitrogen-to-creatinine (B/Cr) ratios in predicting in-hospital mortality, active bleeding, and differentiating gastrointestinal bleeding (GIB) types in patients presenting to the emergency department.
Methods This retrospective study was conducted in a tertiary care hospital between June 1, 2019, and June 30, 2024. Patients over 18 years old diagnosed with GIB and undergoing endoscopy/colonoscopy were included. Demographic, laboratory, and clinical outcomes were analyzed. The B/A and B/ Cr ratios were calculated and evaluated for their prognostic significance using ROC curve analysis.
Results A total of 864 patients were included. Active bleeding was observed in 16.3%, and in-hospital mortality occurred in 7.1% of patients. The threshold values for mortality prediction were determined as 10.15 for the B/A ratio and 28.53 for the B/Cr ratio. The B/A ratio showed a high prognostic value for mortality (AUC: 0.822) and active bleeding (AUC: 0.720), while the B/Cr ratio was particularly effective in differentiating upper GIB.
Conclusion The findings suggest that B/A and B/Cr ratios may provide useful prognostic information in GIB patients. The B/A ratio appears to be particularly relevant for predicting mortality and active bleeding, while the B/Cr ratio could assist in distinguishing upper GIB.
Keywords
Introduction
Acute gastrointestinal bleeding (GIB) is a serious clinical condition frequently encountered in emergency departments (EDs), and it can significantly increase mortality rates if not managed promptly. GIB is broadly classified into two main categories: upper gastrointestinal bleeding (UGIB) and lower gastrointestinal bleeding (LGIB). UGIB typically presents with symptoms such as hematemesis, melena, and shock, whereas LGIB is commonly characterized by hematochezia 1,2,3. The reported mortality rates for UGIB range from 4.5% to 10%, while LGIB, which is associated with lower mortality rates, ranges between 1.9% and 2.3% 4,5,6. These types of bleeding can lead to complications such as hemodynamic instability and organ failure, underscoring the critical importance of accurate and rapid diagnosis 2,3,4. These conditions require immediate clinical intervention, and timely and accurate prognostic assessment plays a crucial role in developing treatment strategies, preventing complications, and reducing mortality. Blood urea nitrogen (BUN) is a primary byproduct of protein metabolism and serves as a significant parameter reflecting the relationship between renal function, protein metabolism, and nutritional status. BUN levels increase in the presence of reduced glomerular filtration rates. Albumin, on the other hand, is an indirect marker of nutritional status and plays various physiological roles, including antioxidant and anti-inflammatory functions. In addition, it is a marker of liver function and inflammatory response and plays a crucial role in acute diseases 7,8,9,10. The combination of these two parameters yields the BUN/Albumin (B/A) ratio, which is a non-invasive and easily accessible metric providing a comprehensive assessment of both renal function and nutritional status. Previous studies have demonstrated that the B/A ratio is an effective predictor of mortality in various conditions such as sepsis, pneumonia, chronic obstructive pulmonary disease, and chronic heart failure 9,10.
Similarly, the blood urea nitrogen/creatinine (B/Cr) ratio is another parameter frequently utilized in the literature, particularly to differentiate GIB types and provide prognostic insights 7,8,11,12. However, the relationship between these ratios and in-hospital mortality, active bleeding, and GIB types in patients presenting to the emergency department remains unclear.
The aim of this study is to evaluate the association of B/A and B/Cr ratios with in-hospital mortality, active bleeding, and GIB types in patients presenting to the emergency department with gastrointestinal bleeding.
Materials and Methods
Study Design
This retrospective observational study was conducted in the emergency department (ED) of a tertiary care hospital. Our study was designed in accordance with the Standards for Reporting of Diagnostic Accuracy Studies (STARD) statement 13.
Data Collection
Data were collected from electronic medical records and patient files. A retrospective review of the clinical and demographic characteristics of the patients, including endoscopy and colonoscopy results, was conducted by two independent emergency medicine specialists with a minimum of three years of experience. In cases where discrepancies arose between the two researchers, the data were reviewed by the principal investigator, and a final decision was made.
Study Population
Between June 1, 2019, and June 30, 2024, we analyzed the consecutive database of all patients who presented to the emergency department (ED) with gastrointestinal bleeding (GIB) and underwent endoscopy and/or colonoscopy performed by the gastroenterology department. Patients aged 18 years or older who presented to the ED with GIB, underwent blood biochemistry analysis within the first 30 minutes of ED admission, were hospitalized for endoscopy and/or colonoscopy, and had complete medical records included in the study. Patients who underwent endoscopy and/or colonoscopy within the first 24 hours after presentation with suspected gastrointestinal bleeding were included. Exclusion criteria were pregnancy, absence of endoscopy/colonoscopy, chronic renal failure, known gastrointestinal malignancy, admission for reasons other than GIB, transfer from another center, and incomplete data. Chronic renal failure was defined as an eGFR <60 mL/min/1.73 m2 for at least three months or a documented history of chronic renal failure in medical records, in accordance with KDIGO guidelines. Patients in the hospital database were classified using the International Statistical Classification of Diseases, Tenth Revision (ICD-10) codes (K25, K25.4, K26, K26.4, K27, K27.4, K28, K28.4, K92.1). Demographic data, comorbidities, medications, vital signs at presentation, laboratory results, endoscopy/colonoscopy findings, hospitalization details, and in- hospital mortality status were recorded. The presence of upper or lower GIB and active bleeding was determined based on endoscopy and colonoscopy findings. B/A and B/Cr ratios were calculated from the patient’s blood biochemistry results, and their associations with in-hospital mortality, active bleeding, and upper/lower GIB were evaluated.
In this study, in-hospital mortality and active bleeding were examined as criteria for poor prognosis. In-hospital mortality was defined as death occurring during hospitalization, regardless of the duration of the stay. Active bleeding was defined as ongoing hemorrhage observed during endoscopic or colonoscopic examination.
Statistical Analysis
All data obtained during the study and recorded in the study form were analyzed using IBM SPSS 20.0 statistical software (Chicago, IL, USA). The normality of the distribution for discrete and continuous numerical variables was assessed using the Kolmogorov-Smirnov test. Descriptive statistics were presented as the median (IQR25-75) for continuous variables and as counts (percentages) for categorical variables. Categorical variables were analyzed using the Chi-square test, while continuous variables were evaluated using the Mann-Whitney U test.
Receiver operating characteristic (ROC) curves were generated to determine the threshold values of B/A and B/Cr ratios for predicting in-hospital mortality, active bleeding, and distinguishing upper/lower GIB, and the area under the curve (AUC) was calculated 14. Results with a p-value of <0.05 were considered statistically significant.
Ethical Approval
This study was approved by the Ethics Committee of Ankara Atatürk Sanatorium Training and Research Hospital (Date: 2025-01-08, No: 2024-BÇEK/204).
Results
A total of 1126 patients diagnosed with GIB were evaluated during the study period. Of these, 864 patients with complete data were included in the study (Figure 1).
The demographic and clinical characteristics of the patients are presented in Table 1. Of the patients, 66.2% were male, with a median age of 64 years (IQR 25-75, 49-74). Laboratory findings revealed a median B/A ratio of 7.4 and a median B/Cr ratio of 24.7. Based on endoscopic and colonoscopic evaluations, active bleeding was observed in 16.3% of patients, while 84.5% were diagnosed with UGIB and 15.5% with LGIB. Additionally, 20% of the patients required admission to the intensive care unit, and the in-hospital mortality rate was 7.1%.
The comparison of B/A and B/Cr ratios concerning mortality, active bleeding, and GIB types is presented in Table 2. The B/A and B/Cr ratios were found to be significantly higher in deceased patients (all p < 0.001). Similarly, both ratios were higher in patients with active bleeding compared to those without active bleeding (all p < 0.001). When comparing upper and lower GIB, both ratios were higher in patients with UGIB (B/A: p = 0.003; B/Cr: p < 0.001).
The evaluation of B/A and B/Cr ratios by ROC analysis for mortality, active bleeding, and upper-lower GIB is shown in Figure 2. The ROC analyses demonstrated that both ratios are effective in determining significant threshold values for mortality, active bleeding, and UGIB. The B/A and B/Cr ratios achieved higher sensitivity and specificity values for predicting mortality and active bleeding.
The prognostic values of B/A and B/Cr ratio levels for predicting mortality, active bleeding, and UGIB are presented in Table 3. The optimal cutoff values for the ratios were calculated using the Youden index. The B/A ratio demonstrated a high prognostic value for predicting mortality, with an AUC of 0.822 (95% CI: 0.771-0.873, p<0.001), achieving 72.1% sensitivity and 80.33% specificity at the best cutoff value of 10.15. Conversely, the B/ Cr ratio showed a lower AUC of 0.694 (95% CI: 0.640-0.748, p<0.001) for mortality prediction, with 64.51% sensitivity and 72.13% specificity at the optimal cutoff value of 28.53.
For predicting active bleeding, the B/A ratio exhibited a significant prognostic value with an AUC of 0.720 (95% CI: 0.673-0.767, p<0.001), while the B/Cr ratio achieved similar results with an AUC of 0.690 (95% CI: 0.644-0.736, p<0.001). Regarding UGIB prediction, the B/A ratio had the lowest AUC of 0.580 (95% CI: 0.527-0.633, p=0.003), whereas the B/Cr ratio demonstrated slightly better prognostic performance with an AUC of 0.612 (95% CI: 0.558-0.667, p<0.001).
Overall, the B/A ratio showed higher accuracy in predicting mortality and active bleeding, while the B/Cr ratio offered better sensitivity for UGIB differentiation.
Discussion
In this study, the prognostic values of the B/A and B/Cr ratios in predicting in-hospital mortality, active bleeding, and upper/ lower GIB types in patients with GIB were evaluated. The results demonstrated that both ratios are effective in predicting poor prognosis. However, the B/A ratio emerged as a superior prognostic tool, offering higher sensitivity and specificity, particularly in predicting mortality and active bleeding, compared to the B/Cr ratio. Conversely, the B/Cr ratio was shown to have a greater prognostic value in predicting UGIB. Dehydration, malnutrition, and renal dysfunction are key determinants of poor prognosis in patients with GIB. Blood loss can lead to hypovolemia and dehydration, which increase renal reabsorption of urea, resulting in elevated BUN levels. While serum BUN levels reflect renal function and protein metabolism, albumin levels represent several physiological conditions, including nutritional status, antioxidant capacity, and inflammatory response. The B/A ratio combines these two parameters, providing a simple and non-invasive measure to comprehensively evaluate both renal function and nutritional status 15,16. Studies have shown that the B/A ratio is an effective biomarker for predicting both mortality and disease severity in conditions such as sepsis, pneumonia, chronic obstructive pulmonary disease, chronic heart failure, and community-acquired pneumonia. Additionally, the B/A ratio has been highlighted in the literature as a valuable parameter for predicting adverse outcomes, including in- hospital complications, multiple organ failure, and ICU admission requirements 9,10,15,16,17,18. Beyond gastrointestinal bleeding, the prognostic utility of the B/A ratio has also been demonstrated in other acute pathologies. For example, Efgan et al. compared the B/A ratio with the BISAP score in patients diagnosed with acute pancreatitis and found that the B/A ratio was as effective as the BISAP score in identifying high-risk patients, with an AUC of 0.757 and an optimal cutoff value of 4.60. As the B/A ratio increased, the risk of severe pancreatitis significantly increased as well (OR: 38.3), supporting its role as an independent predictor of disease severity in acute inflammatory conditions beyond GIB 19. One study reported that the B/A ratio is an independent predictor of poor prognosis and in-hospital mortality in elderly patients with GIB. For in-hospital mortality, the optimal cutoff value for the B/A ratio was determined as 15.1, with a sensitivity of 72.2% and specificity of 76.2% (AUC: 0.770, 95% CI: 0.734–0.803) 16. In our study, the B/A ratio demonstrated a high prognostic value for predicting mortality, with an AUC of 0.822, an optimal cutoff value of 10.15, and sensitivity and specificity of 72.1% and 80.33%, respectively. These findings support the utility of the B/A ratio as a robust predictive tool for in-hospital mortality in GIB patients. Unlike previous studies focusing solely on elderly populations, our study encompassed a broader age group. This broader inclusion underscores the applicability of the B/A ratio across different age groups, supporting its validity as a prognostic marker independent of age.
Although the difference between B/A and B/Cr ratios in predicting active bleeding was less pronounced, both ratios demonstrated significant prognostic value. The B/A ratio showed higher accuracy in predicting active bleeding, with an AUC of 0.720 and an optimal cutoff value of 10.05. These findings suggest that the B/A ratio is a suitable tool for early assessment of the likelihood of active bleeding. The predictive potential of the B/A ratio for active bleeding may be associated with increased urea production resulting from the digestion of blood in the gastrointestinal system, as well as the decrease in serum albumin levels due to blood loss and inflammation.
The digestion of blood or protein in the gastrointestinal system leads to elevated BUN levels. In UGIB, the prolonged presence of blood in the gastrointestinal tract enhances metabolic and absorption processes, resulting in higher BUN levels. Conversely, LGIB, which is typically of colonic origin, exhibits lower BUN levels due to the limited absorptive capacity of the colon. Previous studies have shown that the B/Cr ratio is an effective indicator for distinguishing between upper and lower GIB, with significantly higher levels observed in UGIB 11,12,20. One study reported that a B/Cr ratio above 35 predicted UGIB with a sensitivity of 19.63% and a specificity of 90.16% 12. Another study found that a B/Cr ratio above 36 predicted UGIB with a sensitivity of 93% and a specificity of 27% 20. In our study, both ratios were found to be significant for differentiating between upper and lower GIB, with the B/Cr ratio showing slightly superior performance. For UGIB, the B/Cr ratio achieved an AUC of 0.612, with the optimal cutoff value determined as 20.09 using the Youden index, providing a sensitivity of 68.22% and a specificity of 53.73%. These findings suggest that the B/ Cr ratio could serve as a supportive tool, particularly for UGIB. Therefore, the B/Cr ratio may be beneficial for classifying GIB types, especially in cases where endoscopy or colonoscopy is delayed.
The ability to identify high-risk patients using easily accessible laboratory parameters holds significant importance in clinical practice. In patients with elevated B/A and B/Cr ratios, early initiation of aggressive resuscitation therapies, prioritization of endoscopic interventions, and appropriate allocation of intensive care resources can be ensured. Additionally, these ratios can guide decisions regarding hospital admission or outpatient management, optimizing resource utilization and improving patient outcomes.
Limitations
This study is retrospective and single-centered. Therefore, these findings need to be validated in larger populations and multi- center, prospective studies. Patients with chronic renal failure were excluded from the study, limiting the ability to evaluate the prognostic value of the B/Cr ratio in this specific patient group. Additionally, in patients with liver failure, the diagnostic and prognostic value of these ratios may be restricted due to low BUN levels. Furthermore, since serum albumin levels are typically reduced in liver failure patients, this could negatively impact the reliability and accuracy of the B/A ratio.
Conclusion
In conclusion, this study has demonstrated that the B/A and B/Cr ratios are reliable tools with prognostic value in patients with GIB. Specifically, the B/A ratio has been shown to play a significant role in clinical decision-making processes, particularly for predicting mortality and active bleeding, while the B/Cr ratio may be important for predicting UGIB.
Figures
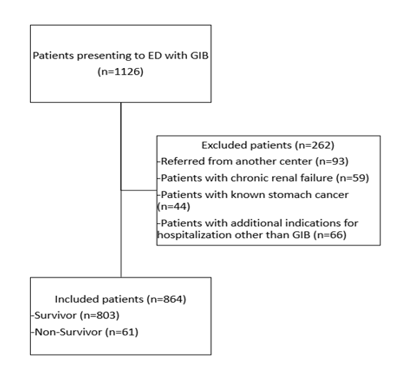
Figure 1. Flowchart of the patients

Figure 2. a. ROC analysis to determine B/A and B/Cr ratios threshold between non-survivor and survivor groups b. ROC analysis to determine B/A and B/Cr ratios threshold between those with and without active bleeding c. ROC analysis to determine B/A and B/Cr ratios threshold between upper and lower GIB
Tables
Table 1. Demographic and clinical characteristics of the patients
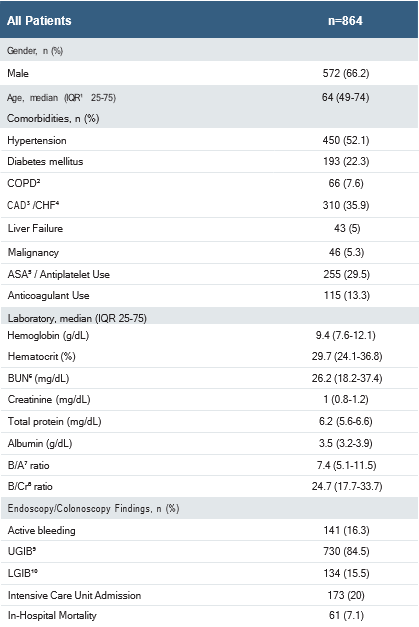
IQR¹: Inter Quartile Range, COPD²: Chronic Obstructive Pulmonary Disease, CAD³: Coronary Artery Disease, CHF⁴: Chronic Heart Failure, ASA⁵: Acetylsalicylic Acid, BUN⁶: Blood urea nitrogen, B/A⁷: Blood urea nitrogen-to-albumin, B/Cr⁸: Blood urea nitrogen-to-creatinine, UGIB⁹: Upper gastrointestinal bleeding, LGIB¹º: Lower gastrointestinal bleeding
Table 2. Comparison of B/A and B/Cr ratios by mortality, active bleeding, and GIB types
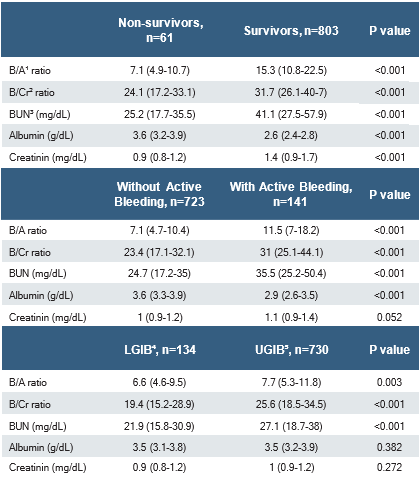
B/A¹: Blood urea nitrogen-to-albumin, B/Cr²: Blood urea nitrogen-to-creatinine, BUN³: Blood urea nitrogen, LGIB⁴: Lower gastrointestinal bleeding, UGIB⁵: Upper gastrointestinal bleeding
Table 3. The prognostic values for B/A and B/Cr ratio levels to the prediction of mortality, active bleeding, and UGIB
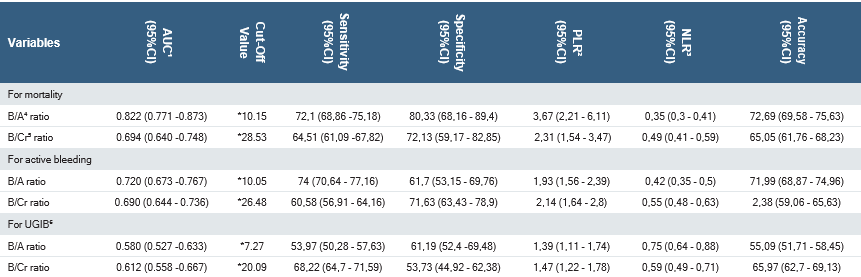
* The best cut-off value calculated according to the Youden index. AUC¹: Area under curve, PLR²: Positive likelihood ratio, NLR³: Negative likelihood ratio, B/A⁴: Blood urea nitrogen-to-albumin, B/Cr⁵: Blood urea nitrogen-to-creatinine, UGIB⁶: Upper gastrointestinal bleeding
References
-
Tokar JL, Higa JT. Acute Gastrointestinal Bleeding. Ann Intern Med. 2022;175(2):17-32.
-
Gaiani F, De’Angelis N, Kayali S, et al. Clinical approach to the patient with acute gastrointestinal bleeding. Acta Biomed. 2018;17;89(8-S):12-9.
-
Emektar E, Dağar S, Çorbacıoğlu ŞK, et al. Predictors of Mortality in Geriatric Patients with Upper Gastrointestinal Bleeding. Eurasian J Emerg Med. 2020;19(4):197-202.
-
Hearnshaw SA, Logan RF, Lowe D, Travis SP, Murphy MF, Palmer KR. Acute upper gastrointestinal bleeding in the UK: Patient characteristics, diagnoses and outcomes in the 2007 UK audit. Gut. 2011;60(10):1327-35.
-
Lanas A, García-Rodríguez LA, Polo-Tomás M, Ponce M, Alonso-Abreu I, PerezAisa MA, et al. Time trends and impact of upper and lower gastrointestinal bleeding and perforation in clinical practice. Am J Gastroenterol. 2009;104(7):1633-41.
-
Venkatesh PG, Njei B, Sanaka MR, Navaneethan U. Risk of comorbidities and outcomes in patients with lower gastrointestinal bleeding - a nationwide study. Int J Colorectal Dis. 2014;29(8):953-60.
-
Wang J, Ren H, Gu B, Zhang Y. Differential Analysis of Blood Routine Examination Parameters in Patients with Upper Gastrointestinal Bleeding and Lower Gastrointestinal Bleeding. Altern Ther Health Med. 2024;30(11):98-102.
-
Tomizawa M, Shinozaki F, Hasegawa R, et al. Laboratory test variables useful for distinguishing upper from lower gastrointestinal bleeding. World J Gastroenterol. 2015;21(20):6246-51.
-
Shi Y, Duan H, Liu J, et al. Blood urea nitrogen to serum albumin ratio is associated with all-cause mortality in patients with AKI: A cohort study. Front Nutr. 2024;11:1353956.
-
Lin Z, Zhao Y, Xiao L, Qi C, Chen Q, Li Y. Blood urea nitrogen to serum albumin ratio as a new prognostic indicator in critical patients with chronic heart failure. ESC Heart Fail. 2022;9(2):1360-9.
-
Machlab S, García-Iglesias P, Martínez-Bauer E, Campo R, Calvet X, Brullet E. Diagnostic utility of nasogastric tube aspiration and the ratio of blood urea nitrogen to creatinine for distinguishing upper and lower gastrointestinal tract bleeding. Emergencias. 2018;30(6):419-23.
-
Zia Ziabari SM, Rimaz S, Shafaghi A, Shakiba M, Pourkazemi Z, Karimzadeh E, et al. Blood Urea Nitrogen to Creatinine ratio in Differentiation of Upper and Lower Gastrointestinal Bleedings; a Diagnostic Accuracy Study. Arch Acad Emerg Med. 2019;7(1):e30.
-
Cohen JF, Korevaar DA, Altman DG, et al. STARD 2015 guidelines for reporting diagnostic accuracy studies: Explanation and elaboration. BMJ Open. 2016;6(11):e012799.
-
Çorbacıoğlu ŞK, Aksel G. Receiver operating characteristic curve analysis in diagnostic accuracy studies: A guide to interpreting the area under the curve Annals of Clinical and Analytical Medicine | 831 This study is retrospective and single-centered. Therefore, these Prognostic value of BUN/albumin and BUN/creatinine ratios in gib value. Turk J Emerg Med. 2023;23(4):195-8.
-
Bae SJ, Lee SH, Yun SJ, Kim K. Comparison of IVC diameter ratio, BUN/ creatinine ratio, and BUN/albumin ratio for risk prediction in emergency department patients. Am J Emerg Med. 2021;47:198-204.
-
Bae SJ, Kim K, Yun SJ, Lee SH. Predictive performance of blood urea nitrogen to serum albumin ratio in elderly patients with gastrointestinal bleeding. Am J Emerg Med. 2021;41:152-7.
-
Ugajin M, Yamaki K, Iwamura N, Yagi T, Asano T. Blood urea nitrogen to serum albumin ratio independently predicts mortality and severity of communityacquired pneumonia. Int J Gen Med. 2012;5:583-9.
-
Ryu S, Oh SK, Cho SU, et al. Utility of the blood urea nitrogen to serum albumin ratio as a prognostic factor of mortality in aspiration pneumonia patients. Am J Emerg Med. 2021;43:175-9.
-
Efgan MG, Payza U, Çınaroğlu OS, Güler EE, Kayalı A. “Comparison of the BUN/Albumin Ratio and BISAP Score in Predicting Severity of Acute Pancreatitis”. Cukurova Med J. 2023;48(3):1096-105.
-
Ernst AA, Haynes ML, Nick TG, Weiss SJ. Usefulness of the blood urea nitrogen/ creatinine ratio in gastrointestinal bleeding. Am J Emerg Med. 1999;17(1):70-2.
Declarations
Scientific Responsibility Statement
The authors declare that they are responsible for the article’s scientific content including study design, data collection, analysis and interpretation, writing, some of the main line, or all of the preparation and scientific review of the contents and approval of the final version of the article.
Animal and Human Rights Statement
All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Funding
None
Conflict of Interest
The authors declare that there is no conflict of interest.
Ethics Declarations
This study was approved by the Ethics Committee of Ankara Atatürk Sanatorium Training and Research Hospital (Date: 2025-01-08, No: 2024-BÇEK/204)
Data Availability
The data supporting the findings of this article are available from the corresponding author upon reasonable request, due to privacy and ethical restrictions. The corresponding author has committed to share the de-identified data with qualified researchers after confirmation of the necessary ethical or institutional approvals. Requests for data access should be directed to bmp.eqco@gmail.com
Additional Information
Publisher’s Note
Bayrakol MP remains neutral with regard to jurisdictional and institutional claims.
Rights and Permissions
About This Article
How to Cite This Article
Handan Özen Olcay, Emine Emektar, Zeynep Hafsa Tokgöz, Evrim Kahramanoğlu Aksoy, Yunsur Çevik. The diagnostic and prognostic value of BUN/albumin and BUN/creatinine ratios in patients with gastrointestinal bleeding presenting to the emergency department. Ann Clin Anal Med 2025;16(11):827-832
Publication History
- Received:
- March 11, 2025
- Accepted:
- January 27, 2025
- Published Online:
- April 22, 2025
- Printed:
- November 1, 2025

