Spinal anesthesia in cesarean delivery: the effect of sitting positions on hypotension and block characteristics
Spinal anesthesia in different sitting positions during cesarean sections
Authors
Abstract
Aim The position of pregnant may affect the incidence of maternal hypotension and characteristics of sensory block. The aim of this prospective study was to investigate the effects of two different sitting positions of pregnant women on the incidence and the onset of hypotension and on the onset of sensory block in pregnant women undergoing spinal anesthesia for elective cesarean delivery.
Materials and Methods A total of 93 patients were randomized into two groups: traditional sitting position (Group I; n = 47) and the group with legs extended parallel to the table (Group II; n = 46). The number of intrathecal applications, maximum level of sensory and motor block, time to sensory block at the level of T6, hemodynamic parameters, use of ephedrine and incidence of side effects were recorded at measurement time points.
Results The number of intrathecal applications, the time it took for the sensory block to reach the T6 dermatome level, the maximum sensory and motor block levels, the frequency of hypotension, the time it took for the first hypotension to develop, the amount of ephedrine used, and the arising complications did not significantly differ between the groups. Group I was shown to have a statistically significant longer transition time than Group II (p < 0.05) from the sitting position to the supine position.
Discussion This study reveals that the sitting position of the pregnant woman has no relationship with maternal hypotension and block characters. Between the groups, the transition from the sitting position to the supine position was found to be shorter than the position in which the legs were extended parallel to the table.
Keywords
Introduction
Spinal anesthesia is preferred in obstetric surgery due to minimal placental transfer (reducing neonatal respiratory depression), no maternal aspiration risk, ease of application, rapid onset, and lower drug use [1, 2, 3, 4]. Maternal hypotension from a sympathetic block is spinal anesthesia’s most common side effect, risking nausea, vomiting, reduced uterine blood flow, fetal acidosis, and neonatal depression [5, 6]. Preventing prolonged hypotension is crucial.
To prevent hypotension during spinal anesthesia in cesarean sections, methods include uterine left deviation, preoperative fluid loading, vasopressors, and regulating injection rate [7, 8, 9]. However, no single method has proven superior in effectiveness. Limited studies have explored spinal anesthesia in various positions to prevent maternal hypotension during cesarean sections. Unlike previous research, our study compares the effects of two different sitting positions during spinal anesthesia on maternal hypotension, vasoconstrictor use, and sensory block levels.
Materials and Methods
The study included 100 ASA II category patients aged 18-40, undergoing their first cesarean section. Pregnant women who did not meet the inclusion criteria and had contraindications for spinal anesthesia were excluded from the study. Exclusions included pregnant women with placental anomalies, hypertension, cardiac, metabolic, vascular, hepatic, or renal diseases, hemodynamic instability, spinal deformities, severe mental retardation, body weight < 50 kg or > 110 kg, height < 140 cm or > 180 cm, drug use affecting metabolic/acid-base balance, those declining spinal anesthesia, and emergency casesAll patients received IV Ringer’s lactate (10 ml/kg), ranitidine (1 mg/kg) and ondansetron (4 mg) before spinal anesthesia. Routine monitoring (ECG, SpO₂, NIBP) was performed, and baseline values were recorded.
The L4-5 site was disinfected with povidone iodine. Patients were randomized into two groups: traditional sitting Figure 1 (Group I, n = 50) and legs parallel to the table Figure 2 Group II, n = 50). Spinal anesthesia was performed at L4-5 using a 25 G Quincke needle (cephalad direction) with 2.2 ml of hyperbaric 0.5% bupivacaine injected over 20 seconds, timed using the Pro Metronome app.
After intrathecal injection, patients were placed supine with a 15-degree left tilt. The anesthesiologist, blinded to position, monitored and collected data. Sensory and motor blocks were assessed every 2 minutes for 15 minutes, then every 5 minutes for 30 minutes. Surgery started at T6 sensory block; patients not reaching T6 within 10 minutes were excluded and given general anesthesia.
During spinal anesthesia, the number of attempts, time to supine position, time to T6 sensory block, maximum sensory block level, time to maximum sensory and motor block (Bromage 3), and patients with sensory block above T4 were recorded. Motor block was assessed using the Bromage scale (0: raise leg; 1: unable to raise leg, flex knee; 2: unable to flex knee, flex ankle; 3: unable to flex knee and ankle). Systolic blood pressure (sBP) was recorded before and after spinal anesthesia. A decrease in systolic arterial pressure below 90 mmHg and/or a more than 30% decrease in baseline blood pressure was considered hypotension. In the case of hypotension, hypotension was treated with a 5 mg bolus of ephedrine each time until the systolic arterial pressure returned to normal limits (> 90 mmHg and > 70% basal value). When the heart rate was < 50 beats/min, it was considered bradycardia, and 0.5 mg IV atropine was administered. The total amount of ephedrine and atropine used was recorded.
When the sample size was calculated with a 95% confidence interval and 80% power using the ephedrine requirement determined in the study by Manouchehrian et al., it was found that 45 patients should be included in each group [10]. Considering data loss, 50 for each group and 100 patients in total were included in the study.
Statistical Analysis
Data were analyzed using SPSS 23.0. Descriptive statistics included numbers, percentages, means, and standard deviations. Normality was assessed using the Kolmogorov-Smirnov test. Group comparisons used the t-test for normally distributed data and the Mann-Whitney U test for non-normal data. Categorical data were compared using the chi-square test. A p-value < 0.05 was considered statistically significant.
Ethical Approval
This study was approved by the Ethics Committee of Karadeniz Technical University (Date: 2021-09-17, No: 2021-33).
Results
The study included 100 patients (Group I: 50, Group II: 50). Seven patients were excluded: 3 due to inadequate sensory block (T6), 3 due to unrelieved pain, and 1 due to hypotension from bleeding. The final analysis involved 93 patients (Group I: 47, Group II: 46). Demographic data showed no significant differences between groups (p > 0.05). Comparison of intrathecal applications, time to T6 sensory block, Bromage Score 3 duration, time to T4 sensory block, and complications (nausea, vomiting, respiratory distress) showed no significant differences between groups (p > 0.05). However, Group I had a significantly longer transition time from sitting to supine than Group II (p < 0.05) (Table 2). When the incidence of hypotension, the time to first hypotension after intrathecal bupivacaine administration, and the need for atropine and ephedrine were compared between the groups (Table 3), no statistically significant difference was observed between both groups (p > 0.05).
Discussion
In this prospective, double-blind, randomized study, we found no difference in procedure success, maternal hypotension, sensory block level, or complications between traditional sitting and sitting with legs parallel to the table. However, transitioning to supine was faster in the legs-parallel position.
Reducing lumbar lordosis before spinal anesthesia is crucial for success. Many studies have explored optimal patient positions to minimize interventions and complications like paresthesia. It has been reported that the rate of paresthesia is lower in the traditional sitting position compared to the lateral decubitus position and the success of the procedure is higher [11, 12]. In light of these findings, in our study, we aimed to compare the traditional sitting position with the position in which the legs are extended parallel to the table in terms of the success of spinal anesthesia. Two studies in the literature showed that different sitting positions did not significantly affect the success of spinal anesthesia [13, 14]. Similarly, in our study, there was no statistically significant difference in the number of spinal anesthesia attempts between these two different sitting positions. However, it was observed that pregnant women who underwent spinal anesthesia with their feet extended parallel to the table transitioned to the surgical position faster.
The severity of maternal hypotension due to spinal anesthesia varies between 25% and 75% depending on the height of the block and whether prophylactic methods are used or not [15]. İt has been shown that the maternal position may be effective in the intrathecal spread of local anesthetic solution and the development of hypotension [16]. In the literature, the effect of spinal anesthesia in the right lateral position and traditional sitting position on the character of the block and hemodynamic changes in the cesarean section has been frequently investigated to date, but we have not encountered a study in the literature investigating the effect of two different sitting positions as in our study.
A study comparing traditional sitting and lateral positions found lower blood pressure at 6 and 8 minutes and higher ephedrine use in the sitting position. Sensory and motor blocks onset faster in the lateral position. [17]. In the sitting position, gravity may hinder the cephalad spread of local anesthetic, potentially delaying sensory block onset. In our study, both groups were in the sitting position, so the intrathecal spread of the local anesthetic was similar and unaffected by gravity. Thus, no significant difference was observed between groups in sensory block time or level.
Since both patient groups were in the sitting position in our study, we hypothesized that there was no difference in aortocaval compression between the groups. We hypothesized that this did not lead to any difference in the progression of intrathecally administered local anesthetic in the cephalic direction. As a result, we observed that there was no significant difference between the groups in terms of the time to reach the maximum sensory block level and the adequate sensory block level.
In a study comparing the traditional sitting position with the lateral decubitus position, it was reported that the intraoperative ephedrine requirement was higher in the sitting position [10]. The reason for this may be that the sitting position decreases the cephalic spread of the local anesthetic agent, causing it to remain in the lumbar region for a longer time and to come into contact with the nerve fibers in this region for a longer time. This may have caused a deeper sympathetic block and thus increased the need for ephedrine by increasing the risk of hypotension. However, since both groups of patients were in a sitting position in our study, the effect of gravity on the spread of local anesthetic did not differ between the groups. Therefore, we think that the block was of similar depth and level in both groups. In conclusion, there was no significant difference in the frequency of hypotension between the groups.
In the sitting position, more venous pooling occurs in the lower extremities of patients, and recovery of venous return occurs later when the patient is in the supine position. Therefore, hypotension may be observed less in pregnant women undergoing spinal anesthesia in the lateral position [18]. We hypothesized that venous pooling would decrease and venous return would recover faster in the feet-parallel group, leading to lower hypotension incidence. However, no significant difference in hypotension incidence was observed between the two groups. This may be because venous return maintained sufficient cardiac output in both sitting positions until supine positioning. The finding of a higher frequency of hypotension in geriatric patients undergoing prostate surgery in the position where the feet were parallel to the table in the study by Afolyan et al differs from the results of our study [19]. The reason for this difference may be explained by increased intra-abdominal pressure in pregnant women, increased venous ponding due to aortocaval compression in the sitting position, and consequently decreased venous return to the heart.
In a study in which three different groups were compared in terms of maternal hypotension during cesarean section including the position in which the legs were parallel to the table, the traditional sitting position, and the left lateral decubitus position, no significant difference was found between the groups in terms of the frequency of maternal hypotension. However, in this study, the frequency of hypotension immediately after spinal anesthesia (when the patient was placed in a supine position) was evaluated [20]. Considering that hypotension after spinal anesthesia usually starts in 5-10 minutes and peaks in 15-20 minutes, the fact that the study evaluated hypotension immediately after spinal anesthesia reflects the frequency of hypotension in the early period, which may cause misleading results [21]. The onset time and severity of hypotension after spinal anesthesia depends on many factors including patient position, fluid replacement, dose of anesthetic agent, and hemodynamic reserve of the patient. Therefore, evaluation of hypotension in the later period may provide more reliable and clinically significant results. Although similar results were obtained in the present study, these results may be insufficient to reflect clinical practice because hypotension was evaluated in the early period.
High sensory block levels (≥ T5 or T4) during spinal anesthesia in cesarean sections increase hypotension risk, raising maternal and fetal complications. Hypotension is more common when the sensory block reaches T5 or T4 [22].
İntrathecal injection in the lateral position causes faster and higher sensory block levels than the sitting position, likely due to easier cephalad spread of hyperbaric bupivacaine with reduced gravity effects [23]. No studies have evaluated sensory block levels in different sitting positions. In our study, we did not observe a significant difference in the intrathecal spread of hyperbaric bupivacaine because both groups of patients were in the sitting position and we concluded that this did not affect the character of sensory block. This finding suggests that the sitting position is not an important factor in determining the spread of local anesthetic agents and thus the level of sensory block during spinal anesthesia. However, given the knowledge that lateral position leads to high levels of sensory block, it is clear that the effects of different positions on sensory block should be further investigated.
In this context, further investigation of the effects of positioning during spinal anesthesia on both the level of sensory block and the incidence of hypotension may make an important contribution to improving maternal and fetal outcomes.
Limitations
A limitation of our study is that the intrathecal injection site (L4-5) was not confirmed by ultrasound, creating uncertainty about the exact injection level. This may affect sensory block levels, hypotension development, and result interpretation.
Ultimately, our study only included elective cesarean sections. Emergency cases, which may lack adequate fluid intake and preoperative optimization, were excluded, as these factors could influence hypotension and sensory block levels with spinal anesthesia.
Conclusion
This study adds to the evidence on optimal spinal anesthesia positioning, finding no significant differences between traditional sitting and legs-parallel positions in success rate, sensory block, or hypotension. However, the legs-parallel position allowed a faster transition to supine, potentially aiding timely intervention in emergencies. Clinicians should continue to consider patient positioning as part of a comprehensive approach to managing spinal anesthesia, particularly in obstetric settings.
Figures
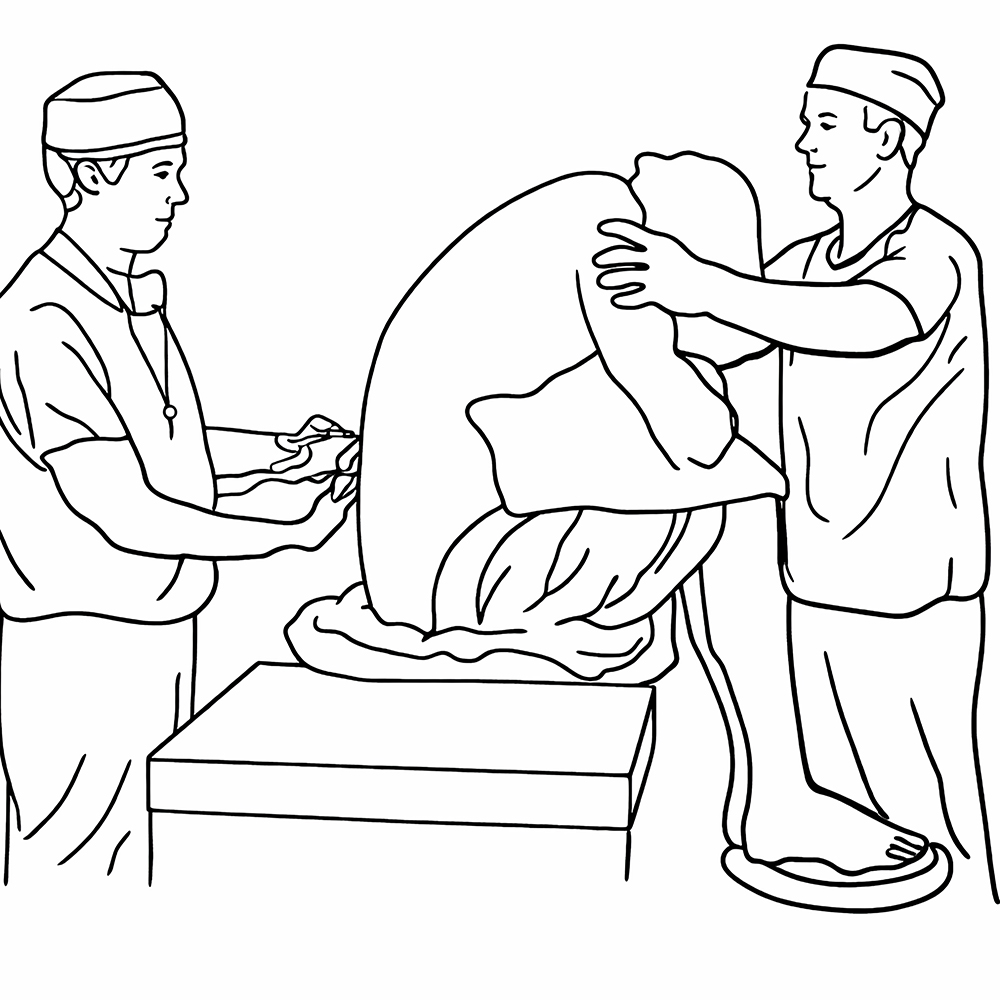
Figure 1
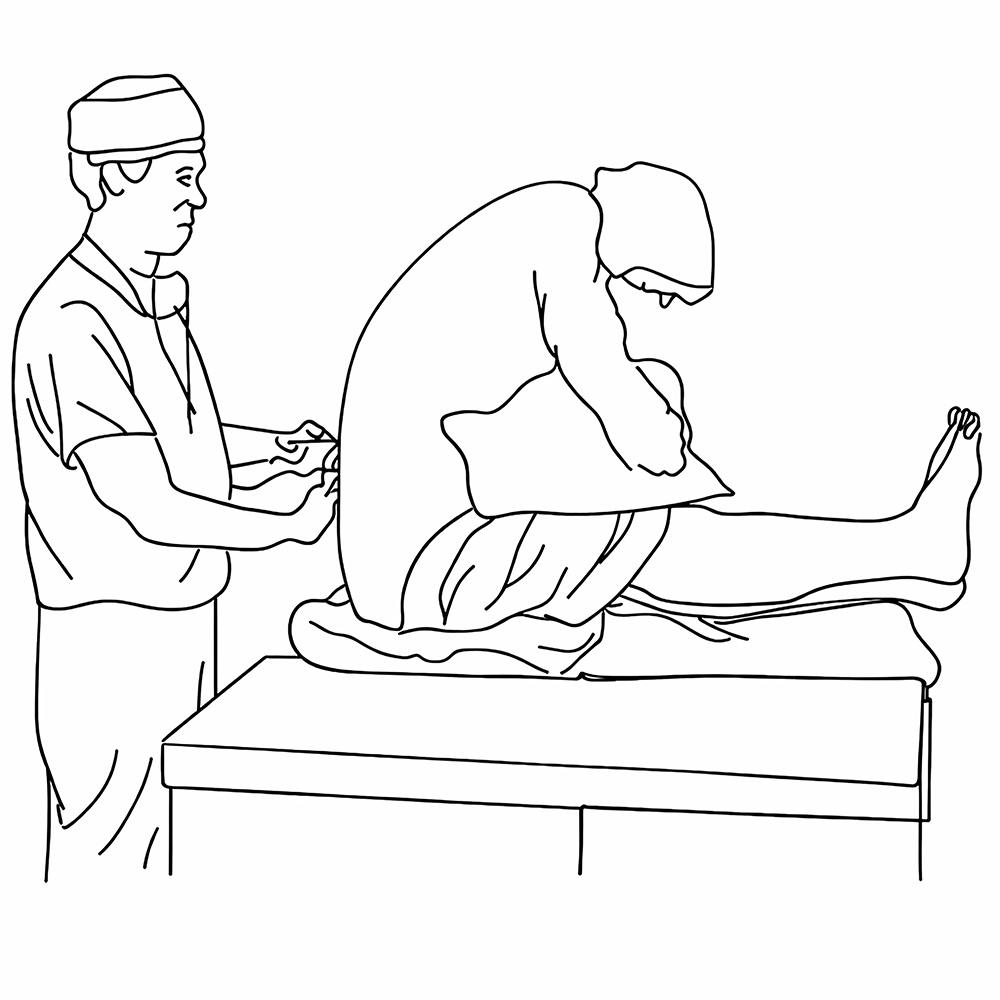
Figure 2
Tables
Table 1. Demographic data
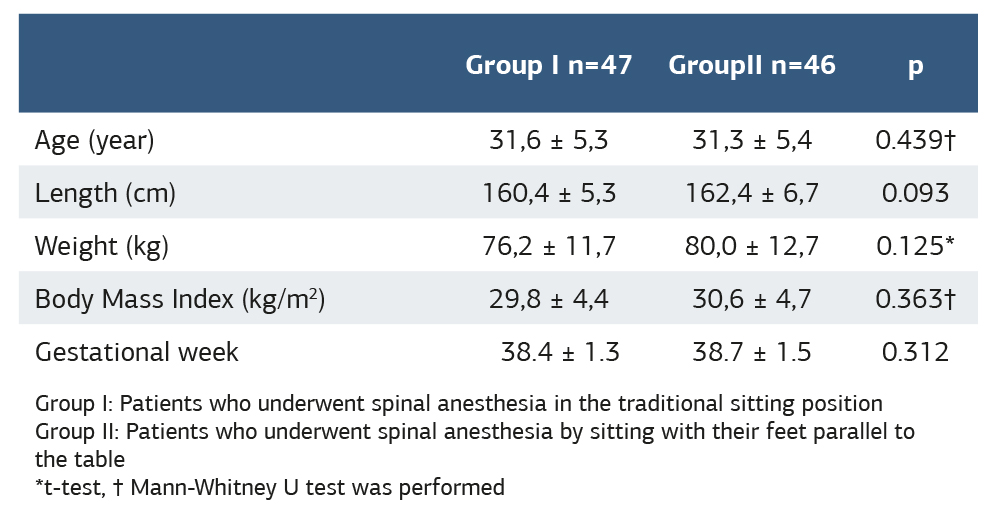
Group I: Patients who underwent spinal anesthesia in the traditional sitting position Group II: Patients who underwent spinal anesthesia by sitting with their feet parallel to the table *t-test, † Mann-Whitney U test was performed
Table 2. Anesthesia durations, block characteristics, and complications
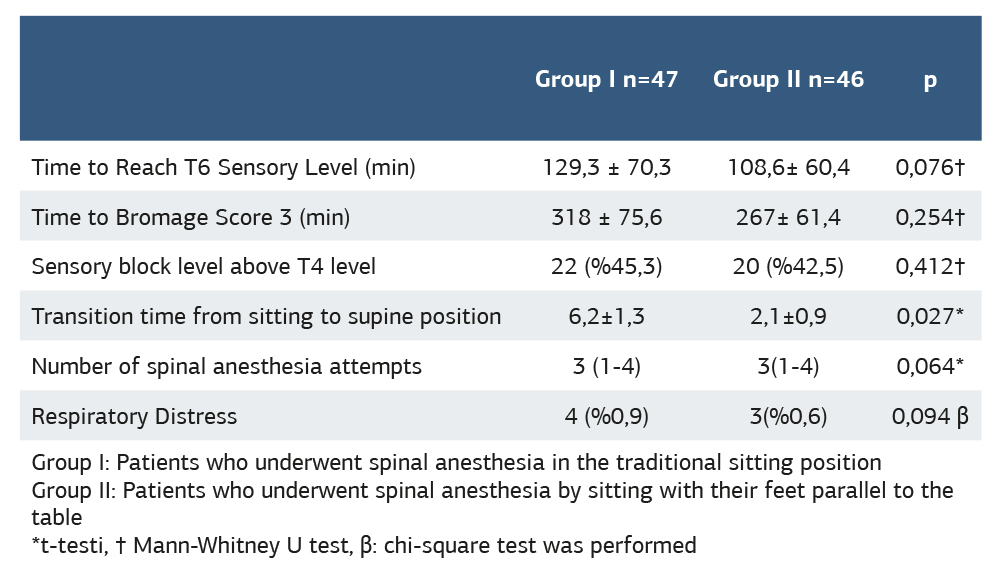
Group I: Patients who underwent spinal anesthesia in the traditional sitting position Group II: Patients who underwent spinal anesthesia by sitting with their feet parallel to the table *t-testi, † Mann-Whitney U test, β: chi-square test was performed
Table 3. Hemodynamic data and ephedrine use
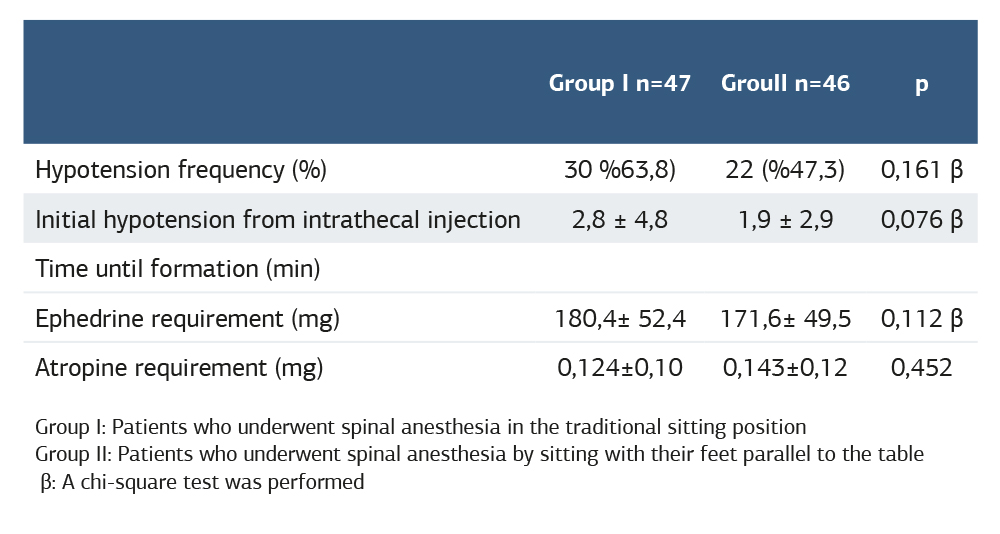
Group I: Patients who underwent spinal anesthesia in the traditional sitting position Group II: Patients who underwent spinal anesthesia by sitting with their feet parallel to the table β: A chi-square test was performed
References
-
Eltzschig HK, Lieberman ES, Camann WR. Regional anesthesia and analgesia for labor and delivery. N Engl J Med. 2003;348(4):319-32. doi: 10.1056/NEJMra021276.
-
Hawkins JL. Anesthesia-related maternal mortality. Clin Obstet Gynecol. 2003;46(3):679-87. doi:10.1097/00003081-200309000-00020.
-
Bucklin BA, Hawkins JL, Anderson JR, Ullrich FA. Obstetric anesthesia workforce survey: twenty-year update. Anesthesiology. 2005;103(3):645-53. doi:10.1097/00000542-200509000-00030.
-
Reynolds F. The effects of maternal labor analgesia on the fetus. Best Pract Res Clin Obstet Gynaecol. 2010;24(3):289-302. doi:10.1016/j.bpobgyn.2009.11.003.
-
Salinas FV, Sueda LA, Liu SS. Physiology of spinal anaesthesia and practical suggestions for successful spinal anaesthesia. Best Pract Res Clin Anaesthesiol. 2003;17(3):289–303. doi:10.1016/S1521-6896(02)00114-3.
-
Burns SM, Cowan CM, Wilkes RG. Prevention and management of hypotension during spinal anesthesia for elective Caesarean section: a survey of practice. Anesthesia. 2001;56(8):794-8. doi:10.1046/j.1365-2044.2001.02058-5.x.
-
Wang X, Xu JM, Zhou F, He L, Cui YL, Li ZJ. Maternal position and developmentof hypotension in patients undergoing cesarean section under combined spinal- epidural anesthesia of intrathecal hyperbaric ropivacaine. Med Sci Monit. 2015;21:52-8. doi:10.12659/MSM.892224.
-
Ngan Kee WD, Khaw KS, Ng FF. Prevention of hypotension during spinal anesthesia for cesarean delivery: an effective technique using combination phenylephrine infusion and crystalloid cohydration. Anesthesiology. 2005;103(4):744-50. doi:10.1097/00000542-200510000-00012.
-
TTugcugil E, Besir A. A comparison of the injection rate of local anesthetic during spinal anesthesia on the onset of sensory block and incidence of hypotension in caesarean section. Clin. Exp. Obstet. Gynecol. 2022;49(7):152. doi:10.31083/j.ceog4907152.
-
Manouchehrian N, Moradi A, Torkashvand L. Comparative study of effect of spinal anesthesia in sitting and lateral positions on the onset time of sensory block and hemodynamic condition in cesarean section: a randomized clinical Trial. Anesth Pain Med. 2021;11(1):e111483. doi:10.5812/aapm.111483.
-
Fernández Sdel R, Taboada M, Ulloa B, Rodríguez J, Masid A, Alvarez J. Needle-induced paresthesiae during single-shot spinal anesthesia: a comparison of sitting versus lateral decubitus position. Reg Anesth Pain Med. 2010;35(1):41-4. doi:10.1097/AAP.0b013e3181c757c8.
-
MM, Khan BA. A comparative study of effects of sitting and lateral positions on quality of block during induction of spinal anaesthesia in patients undergoing cesarean section. J Contemp Med Dent. 2015;3(1):93-4. doi:10.18049/jcmad/319a21.
-
Fisher KS, Arnholt AT, Douglas ME, Vandiver SL, Nguyen DH. A randomized trial of the traditional sitting position versus the hamstring stretch position for labor epidural needle placement. AnesthAnalg.2009;109(2):532-4. doi:10.1213/ane.0b013e3181ac6c79.
-
Soltani MS, Hassani M, Marashi SM. Comparing the squatting position and traditional sitting position for ease of spinal needle placement: a randomized clinical trial. Anesth Pain Med. 2014;4(2):e13969. doi:10.5812/aapm.13969.
-
Ginosar Y, Mirikatani E, Drover DR, Cohen SE, Riley ET. ED50 and ED95 of intrathecal hyperbaric bupivacaine coadministered with opioids for cesarean delivery. Anesthesiology. 2004;100(3):676-82. doi:10.1097/00000542-200403000-00031.
-
Hartwell BL, Aglio LS, Hauch MA, Datta S. Vertebral column length and spread of hyperbaric subarachnoid bupivacaine in the term parturient. Reg Anesth. 1991;16(1):17-9.
-
Rout CC, Rocke DA. Prevention of hypotension following spinal anesthesia for cesarean section. Int Anesthesiol Clin. 1994;32(2):117-35.
-
Afolayan JM, Areo PO, Adegun PT, Ogundipe KO, Filani AB. Comparison of ease of induction of spinal anaesthesia in sitting with legs parallel on the table versus traditional sitting position. Pan Afr Med J. 2017;28:223. doi:10.11604/pamj.2017.28.223.6992.
-
Simin A, Naghipour B, Farzin H, Saeede M, Pouya HM, Hojjat P. Effect of position during induction of spinal anesthesia for cesarean section on maternal hemodynamic: Randomised clinical trial. Journal of Clinical and Diagnostic Research. 2018;12(2):UC05–8. doi:10.7860/JCDR/2018/27753.11184.
-
Palacio Abizanda FJ, Reina MA, Fornet I, López A, López López MA, Morillas Sendín P. Parestesias y anestesia subaracnoidea en cesáreas: estudio comparativo según la posición de la paciente [Paresthesia and spinal anesthesia for cesarean section: comparison of patient positioning]. Rev Esp Anestesiol Reanim. 2009;56(1):21-6. doi:10.1016/S0034-9356(09)70316-0.
-
Fitzgerald JP, Fedoruk KA, Jadin SM, Carvalho B, Halpern SH. Prevention of hypotension after spinal anesthesia for cesarean section: a systematic review and network meta-analysis of randomized controlled trials. Anesthesia. 2020;75(1):109-21. doi:10.1111/anae.14841.
-
Somboonviboon W, Kyokong O, Charuluxananan S, Narasethakamol A. Incidence and risk factors of hypotension and bradycardia after spinal anesthesia for cesarean section. J Med Assoc Thai. 2008;91(2):181-7.
-
Kyokong O, Charuluxananan S, Sriprajittichai P, Poomseetong T, Naksin P. The incidence and risk factors of hypotension and bradycardia associated with spinal anesthesia. J Med Assoc Thai. 2006;89(Suppl 3):S58-64.
Declarations
Scientific Responsibility Statement
The authors declare that they are responsible for the article’s scientific content, including study design, data collection, analysis and interpretation, writing, and some of the main line, or all of the preparation and scientific review of the contents, and approval of the final version of the article.
Animal and Human Rights Statement
All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Funding
None
Conflict of Interest
The authors declare that there is no conflict of interest.
Ethics Declarations
This study was approved by the Ethics Committee of Karadeniz Technical University (Date: 2021-09-17, No: 2021-33)
Data Availability
The datasets used and/or analyzed during the current study are not publicly available due to patient privacy reasons but are available from the corresponding author on reasonable request.
Additional Information
Publisher’s Note
Bayrakol MP remains neutral with regard to jurisdictional and institutional claims.
Rights and Permissions
About This Article
How to Cite This Article
Ömer Furkan Özdemır, Ersagun Tuğcugil, Ahmet Beşir, Bengü Özdemir. Spinal anesthesia in cesarean delivery: the effect of sitting positions on hypotension and block characteristics. Ann Clin Anal Med 2026;17(2):115-119
Publication History
- Received:
- March 17, 2025
- Accepted:
- May 12, 2025
- Published Online:
- June 4, 2025
- Printed:
- February 1, 2026

