Does the coronal and sagittal posture affect the risk of falling in older adults with pain?
Postural alignment and falls in older adults
Authors
Abstract
Aim Fall risk in older adults is linked to poor posture and pain, often focusing on sagittal alignment. This study examines the combined impact of coronal and sagittal posture on fall risk in individuals with mechanical chronic neck, low back, and knee pain.
Methods This prospective cross-sectional study included 146 adults aged ≥65 with pain, selected from 479 screened. Participants were categorized as fallers or non-fallers. Data collected included posture (sagittal, coronal, total) assessed using the New York Posture Rating Scale (NYPRS), pain duration, demographics, comorbidities, number of medications, Timed Up and Go test, Berg Balance Scale (BBS), Four-Step Square Test, and number of falls.
Results Of the 146 participants, 58% had a history of falls, and 71% were females. Neck pain was reported by 28% of participants, knee pain by 39%, and low back pain by 33%. Multivariate logistic regression analysis showed that BBS and total posture score were independently associated with falls (odds ratio 0.8 and 0.9, respectively). This indicated that for every one-unit increase in the BBS and total posture score, the odds of a fall decreased by about 20% and 10%, respectively.
Conclusion The study results indicated that assessing the total posture, not just the sagittal posture, is crucial when evaluating the risk of falls in older adults. Furthermore, the BBS proved particularly valuable in assessing the risk of falls among older adults experiencing chronic mechanical neck, low back, and knee pain.
Keywords
Introduction
As people age, the risk of falling increases. Several significant factors contribute to this risk, including loss of balance, gender, comorbidity, older age, cognitive impairment, polypharmacy, and pain 1,2.
In addition to the various factors influencing falls in older adults, research on postural changes highlights balance deficits and fall risks in older adults. Most of these studies have focused on regional posture changes. It was reported that the forward head shift commonly observed in kyphosis in older adults significantly impacts the body’s center of gravity and contributes to postural instability. It has also been reported that hyperkyphosis increases the risk of falling, especially in older ages, and that there is a gender difference in the relationship between falls and kyphosis [3–5]. Trunk inclination angle, sagittal vertical axis, lumbar lordosis, and hip extension mobility were found to be associated with the risk of falling 6,7. To our knowledge, there is currently no study examining how changes in total posture (TP), both coronal posture (CP) and sagittal posture (SP), affect falls in older adults who experience chronic mechanical pain in the neck, lower back, and knees.
Recent studies suggest that people experiencing chronic pain tend to have weaker balance compared to those without pain. Individuals dealing with both neck and foot pain exhibit even weaker balance than those without pain in those areas. However, when comparing the balance of individuals with back and neck pain, no significant difference was found. It is suggested that pain, along with muscle weakness and limited joint range of motion, impairs dynamic postural stability, increasing the risk of falling 8. The addition of chronic neck pain to the balance weakening associated with aging further exacerbates balance issues 9. Additionally, studies report that changes in walking patterns in older adults with knee pain increase their risk of falling 10. It has also been reported that the risk of falling increases in cases where chronic low back pain is accompanied by hip osteoarthritis 11. Based on our literature review, there is a lack of studies comparing the risk of falls among older adults with pain in different regions, such as the low back, neck, or knee.
Therefore, this study aims to investigate the relationship between fall and pain region, age, gender, education, occupation, marital status, comorbidity, balance, polypharmacy, CP, and SP in older adults.
Materials and Methods
Participants
The research was conducted on patients who presented to the Physical Medicine and Rehabilitation outpatient clinic between November 2023 and April 2024. The inclusion criteria were defined as: (a) ≥ 65 years old, (b) cognitively intact, (c) able to ambulate independently, (d) independent in activities of daily living, and (f) chronic pain in the neck, back, and knees lasting more than three months. The exclusion criteria were:
(a) having visual and hearing problems; (b) medication use with adverse effects on balance; (c) having any serious neurological, cardiopulmonary, or orthopedic disorders; (d) having musculoskeletal surgery; (e) orthostatic hypotension; (f) history of syncope; and (g) temporary loss of consciousness after a fall and injury. 479 older adults were assessed for eligibility. 28% of older individuals did not volunteer to participate in the study, and others had some problems related to exclusion criteria. One hundred forty-six older adults participated in this study.
Measures
Participants were asked about their birth year, gender, occupation, marital status, medications, Charlson Comorbidity Index (CCI), and duration of neck, back, and knee pain 12. Fall history was assessed by asking if they had fallen in the past year and how many times. Those with more than two falls were defined as the “faller group”; others were the “non-faller group”. All participants completed the Timed Up and Go (TUG), Berg Balance Scale (BBS), Four-Step Square Test (FSST), and New York Posture Rating Scale (NYPRS).
In the TUG, participants rose from a chair, walked 3 meters, returned, and sat down. It was done twice with a 10-minute rest; the better time was recorded 13.
The Turkish BBS consists of 14 items scored 0–4. Scores of 0–20 indicate poor balance, 21–40 moderate, and 41–56 good balance 14.
In the FSST, participants stepped into four numbered squares in a set sequence. It was repeated twice, and the best score was noted 15.
Posture was assessed using the NYPRS 13 body parts from lateral and posterior views as 5 (normal), 3 (slight deviation), or 1 (pronounced deviation), reported as CP, SP, TP scores 16.
Data Analysis
Using G*Power 3.1.9, a minimum of 42 participants per group was calculated (effect size = 0.8, α = 0.05, power = 95%) and increased to 60 per group to account for potential data loss. Normality was assessed using the Kolmogorov-Smirnov and Shapiro-Wilk tests. Due to non-normal distribution, the Mann- Whitney U test was used for continuous variables and the chi- square test for categorical variables to compare fallers and non-fallers.
Univariate binary logistic regression was performed to examine the association between fall status (1 = faller, 2 = non-faller) and various predictors, including non-correlated continuous variables (age, CCI, TUG, FSST, BBS, CP, SP, TP, pain duration, medication number) and categorical variables (pain region, gender, education, occupation, marital status). Odds ratios (OR) with 95% confidence intervals (CI) and p-values were calculated. Multicollinearity was assessed using the variance inflation factor (VIF), and values close to 1 indicated no significant multicollinearity. A final multivariate model was adjusted for age, gender, marital status, CCI, TUG, FSST, BBS, CP, SP, and TP. The analysis included 146 participants (85 fallers [58.22%], 61 non-fallers [41.78%]). A p-value < 0.05 was considered statistically significant. All analyses were conducted using SAS v9.4 (SAS Institute, Cary, NC).
Ethical Approval
This study was approved by the Clinical Research Ethics Committee of Antalya Training and Research Hospital (Date: 2023-12-10, No:14/7).
Results
The faller group was predominantly female (64%), while the non-faller group was mostly male (56%) (p < 0.05). The proportion of older adults living alone in the group of fallers (74%) was higher compared to the non-faller group (26%) (p < 0.05). There was no difference between the groups in terms of TUG, FSST, medication number, pain region, education level, and occupation (p > 0.05). In the faller group, participants were older, had higher CCI scores, lower CP scores, lower SP scores, lower TP scores, lower BBS scores, and longer pain duration compared to the non-faller group (p < 0.05) (Table 1). The univariate logistic regression analysis was carried out to determine whether the association between the response and each term in the model is statistically significant (Table 2, Figure 1). The pain region, education, occupation, pain duration, and medication number were not significantly related to fall incidents. In the logistic analysis, the CCI was associated with falls (OR 1.9; 95% CI 1.3-2.8). This indicates that for every one unit increase in the CCI, the probability of a fall almost doubles. The BBS had a trend toward a significant association with falls (OR 0.8; 95% CI 0.8-0.9). For every one unit increase in the BBS, the odds of a fall decrease by about 20%. The odds of a fall are 2.3 times higher for females than males (OR 2.3; 95% CI 1.1- 4.7). The data indicate that married older adults have a 60% lower likelihood of experiencing a fall compared to those who are single (OR 0.4; 95% CI 0.2- 0.9). The probability of falling does not significantly change with the SP score (OR 0.9; 95% CI 0.9-1.0), age (OR 1.2; 95% CI 1.1-1.4), TUG (OR 1.1; 95% CI 1.0-1.1), CP score (OR 0.9; 95% CI 0.8-0.9), and FSST (OR 1.1; 95% CI 1.0-1.2).
Additional adjustments are made to control for variables such as age, gender, marital status, CCI, TUG, FSST, BBS, CP, SP, and TP to strengthen the association. However, in this multivariate analysis, including all characteristics with p < .20 in the univariate analysis, only the BBS and TP are independently associated with falls (OR 0.8; 95% CI 0.8-0.9 and OR 0.9; 95% CI: 0.8- 1.1, respectively). This indicates that for every one unit increase in the BBS and TP, the odds of a fall decrease by about 20% and 10%, respectively.
Discussion
In this study, faller group has a higher age and CCI, lower CP, SP, TP, BBS score, and longer pain duration. There is no difference between the groups in terms of TUG, FSST, number of medications, pain region, educational level, and occupation. Multivariate regression analysis indicates that only BBS and TP are independently associated with falls. This means that with a one-unit increase in the BBS and TP scores, the estimated probability of a fall decreases by approximately 20% and 10%, respectively.
In older adults, postural changes affecting the sagittal vertical axis, such as forward displacement, kyphosis, loss of lumbar lordosis, and limited hip extension, have been linked to increased fall risk 3,6,7 Some studies suggest that only hyperkyphosis, rather than kyphosis alone, is associated with falls. Although a definitive threshold is lacking, hyperkyphosis is often defined as a Cobb angle ≥50° in the standing position 5. One study reported that severe kyphotic posture increases fall risk in men, while no such association was found for mild kyphosis or in women 4. In addition to hyperkyphosis, loss of lumbar lordosis and changes in the ankle and foot alignment may also impair balance and increase fall risk in older adults 17. When assessing posture-related fall risk, it is important to consider not only SP but also CP and TP. However, studies on CP and TP changes remain limited. In our study, although CP, SP, and TP scores were lower in the faller group, only the TP score was independently associated with falls. Multicollinearity analysis revealed strong correlations between TP, CP, and SP scores, as indicated by high VIF values. Therefore, TP score may offer a more accurate assessment of fall risk than evaluating SP or CP scores separately.
Hirase et al. reported a strong link between chronic pain and increased body sway during static posture, which impairs dynamic stability and elevates fall risk 8. Gale et al. found that severe pain increases fall risk in men but not in women 18. While no significant differences in balance weakness have been identified across pain regions, it is suggested to be most common in those with low back pain, followed by neck, hip, knee, and foot pain 9. However, to our knowledge, no studies have directly compared fall risk across different pain regions. One study reported increased fall risk in individuals with neck pain, regardless of age. Additionally, older adults with bilateral stage 4 medial knee osteoarthritis (per Kellgren and Lawrence criteria) show impaired balance and higher fall risk 10. Chronic low back pain combined with hip osteoarthritis has also been associated with falls in older adults 11. In our study, no significant differences were observed between fallers and non- fallers in terms of pain region or duration, and no association was found between pain characteristics and falls.
Comorbidity is recognized as a modifiable risk factor for falls in individuals over 60 years of age 2,19. Diabetes and fear of falling are particularly strong predictors of fall risk in older adults with knee osteoarthritis 10. One study found that comorbidity and balance weakness predict fall risk in men, but not in women 18. Additionally, both the type and number of comorbidities significantly influence fall risk 1. Conditions such as arthritis, renal disease, cerebrovascular events, depression, incontinence, and respiratory diseases have been identified as independent risk factors. In our study, although comorbidity scores were higher in fallers, no significant association was found between comorbidity and falls, possibly due to differences in the types of comorbidities across groups.
Various tests are used to assess balance in older adults. While the One-Leg Stance test and BBS can distinguish between fallers and non-fallers, the TUG and Functional Reach tests cannot 20. The FSST has shown the ability to differentiate between non-fallers and multiple fallers, particularly in older adults who use assistive devices 21. However, opinions differ regarding the TUG test; some argue that relying on it alone may be misleading, and the commonly used 12.5-second cut-off has limited predictive value. Thus, the TUG test is recommended primarily for those at high risk of falling 13,22. In our study, the BBS was independently associated with falls, with each unit increase reducing fall probability by approximately 20%.
The researchers indicate that the risk of falling increases as people age, with advanced age being the primary factor linked to a higher risk of falling for both males and females 17,18,23. It has been reported that 25% of older adults aged 70 years experience falls, and this rate increases to 35% for those aged 75 years and older 24. In our study, although the faller group is older than the non-faller group, we did not find a relationship between age and falling. This can be due to the smaller number of older adults in the group of fallers. Specifically, 46% of the faller group falls within the 65-69 age range, 29% are aged 70- 79, and 7% are 80 or older.
Polypharmacy is commonly defined as the concurrent use of five or more medications 25. One study classified 5–6 medications per day as polypharmacy and ≥10 as hyperpolypharmacy. A higher medication load has been associated with increased fall risk 2. In this study, participants who are using medications that could increase the risk of falling are excluded. It is believed that the absence of a correlation between taking multiple medications and falling may be attributed to the fact that 16% of the non-falling group and only 7% of the falling group use five or more medications.
Although we do not find any relation between marital status and fall in this study, marital status appears to influence fall risk, with married older adults reportedly experiencing a lower risk 18.
Limitations
Although all participants were independent in daily activities and ambulation, this study has several limitations. First, although chronic pain was among the inclusion criteria, pain intensity was not measured using standardized tools such as the Visual Analog Scale (VAS) or Numeric Rating Scale (NRS). This lack of standardized assessment limits the ability to compare pain severity across different anatomical regions and may affect the interpretation of its relationship with posture and fall risk. Additionally, physical activity levels, which are known to be associated with chronic pain, were not evaluated. The study also lacks a longitudinal design, preventing causal inferences regarding posture and falls. Muscle strength and joint range of motion were assessed clinically without the use of objective measurements such as flexibility tests or dynamometry. Furthermore, although the overall sample size was acceptable and justified by a power analysis, the relatively small number of participants in certain subgroups, particularly those aged 80 years and older, may further limit the generalizability of the finding.
Conclusion
In conclusion, the study found that both balance and TP are linked to the risk of falls in older adults experiencing neck, low back, and knee pain. It suggests that for every one-point increase in the BBS and TP scores, the likelihood of experiencing a fall decreases by around 20% and 10%, respectively. The research highlights the need to take into account both TP and areas of pain when studying fall risk in older adults. It also recommends using the BBS for this group. The study underscores the importance of integrating these factors into personalized fall prevention strategies for older adults.
Figures
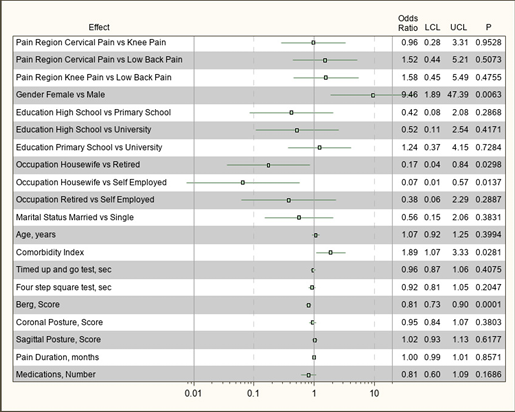
Figure 1. Forest plot for the Odds Ratios with 95% Confidence Intervals (LCL and UCL) and p- p-values of explanatory variables in univariate analysis
Tables
Table 1. Forest plot for the Odds Ratios with 95% Confidence Intervals (LCL and UCL) and p- p-values of explanatory variables in univariate analysis

Abbreviation: CCI-Charlson Comorbidity Index, TUG-Timed Up and Go, FSST-Four Step Square Test, BBS-Berg Balance Scale
Table 2. Results of univariate and multivariate logistic regression analysis
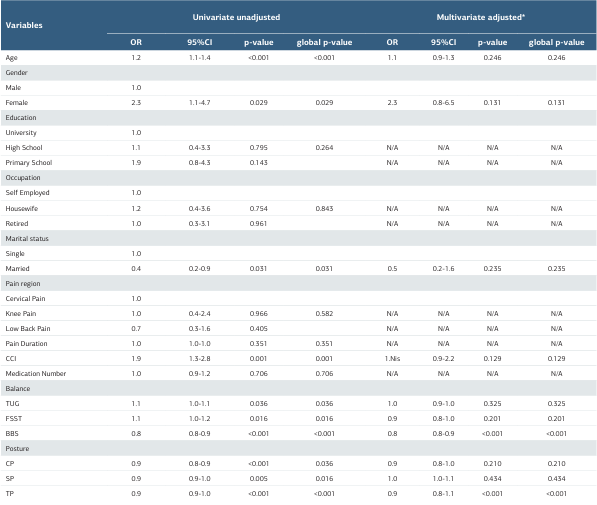
CI = Confidence Interval; OR = Odds Ratio; *Adjusted for age, gender, CCI-Charlson Comorbidity Index, TUG-Timed Up and Go, FSST-Four Step Square Test, BBS-Berg Balance Scale, CP-Coronal Posture, SP-Sagittal Posture, TP-Total Posture, and Marital Status
References
-
Yang X, Li L, Xie F, Wang Z. A prospective cohort study of the impact of chronic disease on fall injuries in middle-aged and older adults. Open Med (Wars). 2023;18(1):20230748. doi:10.1515/med-2023-0748.
-
Dokuzlar O, Koc Okudur S, Smith L, et al. Assessment of factors that increase risk of falling in older women by four different clinical methods. Aging Clin Exp Res. 2020;32(3):483-90. doi:10.1007/s40520-019-01220-8.
-
Nikolaou DA, Rizou S, Lyritis GP, Nikolaou V, Babis GC, Chronopoulos E. Change in kyphosis does not affect the risk of falling in postmenopausal osteopenic and osteoporotic women. J Musculoskelet Neuronal Interact. 2021;21(1):157-61.
-
Tominaga R, Fukuma S, Yamazaki S, et al. Relationship between kyphotic posture and falls in community-dwelling men and women: the locomotive syndrome and health outcome in Aizu cohort study. Spine (Phila Pa 1976). 2016;41(15):1232-8. doi:10.1097/BRS.0000000000001602.
-
Koelé MC, Lems WF, Willems HC. The clinical relevance of hyperkyphosis: A narrative review. Front Endocrinol (Lausanne). 2020;11:5. doi:10.3389/ fendo.2020.00005.
-
Nagai T, Miyagami M, Okano I, et al. Association of spinal alignment and abdominal circumference with sarcopenia status and fall risk in patients with osteoporosis: a retrospective study. Nutrients. 2023;15(11):2571. doi:10.3390/ nu15112571.
-
Ito H, Toyone T, Nagai T, Ishikawa K, Kuroda T, Inagaki K. Relationship between muscle mass of the lower limbs and falls caused by spinal misalignment in women aged 70 years. Clin Spine Surg. 2021;34(1):E19-25. doi:10.1097/ BSD.0000000000001009.
-
Hirase T, Okubo Y, Sturnieks DL, Lord SR. Pain is associated with poor balance in community-dwelling older adults: a systematic review and meta-analysis. J Am Med Dir Assoc. 2020;21(5):597-603.e8. doi:10.1016/j.jamda.2020.02.011.
-
Madsalae T, Thongprong T, Chinkulprasert C, Boonsinsukh R. Can the balance evaluation systems test be used to identify system-specific postural control impairments in older adults with chronic neck pain? Front Med (Lausanne). 2022;9:1012880. doi:10.3389/fmed.2022.1012880.
-
Rosadi R, Jankaew A, Wu PT, Kuo LC, Lin CF. Factors associated with falls in patients with knee osteoarthritis: a cross-sectional study. Medicine (Baltimore). 2022;101(48):e32146. doi:10.1097/MD.0000000000032146.
-
Knox PJ, Coyle PC, Pugliese JM, Pohlig RT, Sions JM, Hicks GE. Hip osteoarthritis signs and symptoms are associated with increased fall risk among community- dwelling older adults with chronic low back pain: a prospective study. Arthritis Res Ther. 2021;23(1):71. doi:10.1186/s13075-021-02455-5.
-
Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40(5):373-83. doi:10.1016/0021-9681(87)90171-8.
-
Ibeneme SC, Eze JC, Okonkwo UP, Ibeneme GC, Fortwengel G. Evaluating the discriminatory power of the velocity field diagram and timed-up-and-go test in determining the fall status of community-dwelling older adults: a cross-sectional observational study. BMC Geriatr. 2022;22(1):658. doi:10.1186/s12877-022- 03282-2.
-
Sahin F, Yilmaz F, Ozmaden A, Kotevoglu N, Sahin T, Kuran B. Reliability and validity of the Turkish version of the Berg Balance Scale. J Geriatr Phys Ther. 2008;31(1):32-7. doi:10.1519/00139143-200831010-00006.
-
Moore M, Barker K. The validity and reliability of the four-square step test in different adult populations: a systematic review. Syst Rev. 2017;6(1):187. doi:10.1186/s13643-017-0577-5.
-
McRoberts LB, Cloud RM, Black CM. Evaluation of the New York Posture Rating Chart for assessing changes in postural alignment in a garment study. Cloth Text Res J. 2013;31(2):81-96. doi:10.1177/0887302X13480558.
-
Fernandes VLS, Ribeiro DM, Fernandes LC, Menezes RL de. Postural changes versus balance control and falls in community-living older adults: a systematic review. Fisioter Mov. 2018;31:e003125. doi:10.1590/1980-5918.031.AO25.
-
Gale CR, Westbury LD, Cooper C, Dennison EM. Risk factors for incident falls in older men and women: the English longitudinal study of ageing. BMC Geriatr. 2018;18(1):117. doi:10.1186/s12877-018-0806-3.
-
Montero-Odasso M, van der Velde N, Martin FC, et al. World guidelines for falls prevention and management for older adults: a global initiative. Age Ageing. 2022;51(9):afac205. doi:10.1093/ageing/afac205.
-
Demircioğlu A, Kezban Şahin Ü, Acaröz S. Discriminative ability of the four balance measures for previous fall experience in Turkish community-dwelling older adults. J Aging Phys Act. 2022;30(6):980-6. doi:10.1123/japa.2021-0415.
-
Cleary K, Skornyakov E. Predicting falls in older adults using the four square step test. Physiother Theory Pract. 2017;33(10):766-71. doi:10.1080/09593985.2017.1354951.
-
Wang J, Chen X, Sun X, et al. The Application of “timed up and go” test in fall screening of elderly people in Shanghai: a cross-sectional study. Iran J Public Health. 2021;50(12):2567-75. doi:10.18502/ijph.v50i12.7940.
-
Koelé MC, Willems HC, Swart KMA, et al. The association between hyperkyphosis and fall incidence among community-dwelling older adults. Osteoporos Int. 2022;33(2):403-11. doi:10.1007/s00198-021-06136-6.
-
Tinetti ME, Speechley M. Prevention of falls among the elderly. N Engl J Med. 1989;320(16):1055-9. doi:10.1056/NEJM198904203201606.
-
Masnoon N, Shakib S, Kalisch-Ellett L, Caughey GE. What is polypharmacy? A systematic review of definitions. BMC Geriatr. 2017;17(1):230. doi:10.1186/ s12877-017-0621-2.
Declarations
Scientific Responsibility Statement
The authors declare that they are responsible for the article’s scientific content, including study design, data collection, analysis and interpretation, writing, and some of the main line, or all of the preparation and scientific review of the contents, and approval of the final version of the article.
Animal and Human Rights Statement
All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Funding
None
Conflict of Interest
The authors declare that there is no conflict of interest.
Ethics Declarations
This study was approved by the Ethics Committee of Antalya Training and Research Hospital (Date: 2023-12-10, No:14/7)
Data Availability
The datasets used and/or analyzed during the current study are not publicly available due to patient privacy reasons but are available from the corresponding author on reasonable request.
Additional Information
Publisher’s Note
Bayrakol MP remains neutral with regard to jurisdictional and institutional claims.
Rights and Permissions
About This Article
How to Cite This Article
Gülşah Çelik, Naciye Füsun Toraman, Ali Akdağ, İbrahim Ethem Hindistan. Does the coronal and sagittal posture affect the risk of falling in older adults with pain? Ann Clin Anal Med 2026;17(1):33-38
Publication History
- Received:
- March 25, 2025
- Accepted:
- May 12, 2025
- Published Online:
- May 26, 2025
- Printed:
- January 1, 2026

