Prognostic relevance of biochemical markers integrated with simplified pulmonary embolism severity index in acute pulmonary embolism
sPESI-linked biomarkers in PE prognosis
Authors
Abstract
Aim This prospective investigation evaluated the prognostic performance of pro-B-type natriuretic peptide (pro-BNP) and complementary biochemical markers in predicting 30-day mortality among patients with acute pulmonary embolism (APE), stratified by the simplified Pulmonary Embolism Severity Index (sPESI).
Methods Eighty-seven consecutive patients with radiologically confirmed APE via computed tomography pulmonary angiography were prospectively enrolled between June 2020 and May 2021. Patients were stratified into low-risk (sPESI = 0, n = 44) and high-risk (sPESI ≥ 1, n = 43) categories. Biochemical markers, including pro-BNP, D-dimer, lactate, troponin, neutrophil-to-lymphocyte ratio (NLR), and platelet-to-lymphocyte ratio (PLR), were systematically analysed for association with 30-day all-cause mortality. Predictive performance was assessed using point-biserial correlation and receiver operating characteristic curve analysis.
Results The cohort demonstrated a mean age of 65.0 ± 15.1 years with 57.5% female predominance and 12.5% 30-day mortality. Pro-BNP exhibited superior discriminatory capacity (AUC = 0.854, r < su b> pb < /sub >= 0.446, p < 0.001), with non-survivors demonstrating 14-fold elevation compared to survivors (7194 vs. 526 pg/mL, p = 0.001). Significant pro-BNP gradients were observed across sPESI categories (1029 vs. 372 pg/mL, p = 0.027). While D-dimer and lactate correlated with disease severity, neither predicted mortality. Troponin, NLR, and PLR demonstrated no prognostic value.
Conclusion Pro-BNP substantially outperformed conventional clinical scoring and alternative biomarkers in mortality prediction, providing a quantitative assessment of right ventricular compromise beyond categorical risk stratification. Integration of pro-BNP into routine prognostic protocols may optimize patient triage and therapeutic decision-making in acute pulmonary embolism management.
Keywords
Introduction
Acute pulmonary embolism (APE) remains one of the most challenging cardiovascular emergencies encountered in clinical practice. Its unpredictable course—ranging from silent presentation to sudden hemodynamic collapse—combined with substantial mortality rates, continues to place considerable strain on healthcare systems worldwide 1. The cornerstone of effective management lies in early and accurate risk stratification, which directly influences critical therapeutic decisions, including anticoagulation alone, systemic thrombolytic therapy, or mechanical intervention. Clinical scoring tools like the simplified Pulmonary Embolism Severity Index (sPESI) have proven valuable in identifying low-risk patients suitable for outpatient care 2. Yet clinicians frequently encounter a troubling scenario: patients who appear clinically stable but harbour subclinical right ventricular compromise that escapes detection by clinical scores alone. This prognostic uncertainty has been repeatedly documented in hemodynamically stable cohorts, underscoring the limitations of relying exclusively on clinical parameters 3,4.
Biomarkers have emerged as powerful adjuncts in bridging this gap. By quantifying the physiological derangements triggered by embolic obstruction—particularly right ventricular strain and myocardial injury—they provide objective data that complements clinical assessment. Natriuretic peptides (BNP and NT-proBNP) have demonstrated consistent prognostic value, reflecting the degree of acute pressure overload imposed on the right ventricle 5,6. D-dimer levels, beyond their diagnostic utility, may correlate with clot burden and ongoing thrombotic activity, while elevated lactate signals inadequate tissue perfusion and portends worse outcomes 7,8. Cardiac troponin, though widely studied as a marker of myocardial damage, yields conflicting evidence regarding its predictive capacity specifically in normotensive APE patients 9. More recently, attention has turned toward inflammation- based hematological indices. The neutrophil-to-lymphocyte ratio (NLR) and platelet-to-lymphocyte ratio (PLR) represent easily accessible parameters that may reflect the systemic inflammatory burden and have shown associations with short- term mortality and clinical severity in APE populations 10,11. Imaging remains indispensable. Computed tomography, pulmonary angiography, and echocardiography not only confirm diagnosis but also reveal critical structural and functional abnormalities —such as right ventricular dilatation or significant thrombus load— that carry independent prognostic weight 12,13. Electrocardiographic findings, though limited in diagnostic sensitivity, may occasionally provide critical prognostic insights; rare presentations such as precordial ST- segment elevation in APE, while easily confused with acute myocardial infarction, have been associated with more severe hemodynamic compromise and adverse outcomes 14. The integration of these imaging findings with biochemical data represents a multimodal approach that may enhance risk prediction beyond what either modality achieves in isolation. Against this backdrop, this study was designed to investigate whether the integration of selected biomarkers—particularly NT-proBNP—into the established sPESI clinical scoring system could meaningfully enhance prognostic accuracy and refine risk stratification in patients with acute pulmonary embolism.
Materials and Methods
Study Design and Participants
This prospective cohort study was carried out at Necmettin Erbakan University between June 2020 and May 2021. Individuals admitted to the emergency or pulmonary departments with confirmed acute pulmonary embolism (APE) via computed tomography pulmonary angiography (CTPA) were considered for inclusion. Patients were excluded if they were younger than 18 years old, pregnant, had chronic embolism, or lacked sufficient laboratory data.
Data Collection
Data on patient demographics, medical history, and sPESI scoring parameters were retrieved from electronic medical records. At the time of hospital admission, the following biochemical markers were assessed: proBNP, D-dimer, lactate, troponin, neutrophil-to-lymphocyte ratio (NLR), and platelet-to- lymphocyte ratio (PLR). Additionally, Doppler ultrasound was used to evaluate the presence of deep vein thrombosis (DVT). The main clinical endpoint was defined as mortality within 30 days following diagnosis.
Statistical Analysis
Statistical evaluations were conducted using SPSS version 18.0. All continuous variables are presented as median (interquartile range) unless otherwise specified. Statistical comparisons employed Mann-Whitney U tests for continuous variables and Fisher’s exact or chi-square tests for categorical variables, with p < 0.05 considered statistically significant. Predictive performance was assessed using point-biserial correlation and area under the receiver operating characteristic curve (AUC) analysis.
Ethical Approval
This study was approved by the Necmettin Erbakan University Non-Drug and Medical Device Research Ethics Committee (Date: 2020-06-06, No: 2020/2577).
Results
Study Population and Baseline Characteristics
A total of 87 patients with confirmed acute pulmonary embolism were enrolled in this prospective cohort study during the period from June 2020 to May 2021. The mean age of the study population was 65.0 ± 15.1 years (median: 67 years, IQR: 54- 76 years), with a slight female predominance (57.5% female, n = 50; 42.5% male, n = 37; female-to-male ratio: 1.35:1). The mean body mass index (BMI) was 28.1 ± 6.9 kg/m2, with the majority of patients classified as overweight (37.9%, n = 33) or obese (33.4%, n = 29). The 30-day all-cause mortality rate was 12.6% (n = 11), with a mean time to death of 22.5 ± 7.8 days among non-survivors (Table 1).
Simplified Pulmonary Embolism Severity Index (s-PESI)
Distribution and Risk Stratification
The study population was evenly distributed between low-risk (s-PESI = 0: 50.0%, n = 44) and high-risk (s-PESI ≥ 1: 48.9%, n = 43) categories (Table 1). Mortality rates demonstrated a clinically significant trend toward higher risk in the s-PESI ≥ 1 group: 6.8% (3 / 44) in the s-PESI 0 group versus 18.6% (8 / 43) in the s-PESI ≥ 1 group, representing a 2.7-fold increase in mortality risk (Figure 1B). Although this difference did not reach statistical significance (χ2 = 1.772, p = 0.183), likely due to the limited sample size, the observed mortality gradient is consistent with established risk stratification models.
Biochemical Biomarkers and Mortality Association
Pro-B-Type Natriuretic Peptide (Pro-BNP)
Pro-BNP emerged as the most powerful independent predictor of 30-day mortality in our cohort. Of the 82 patients (94.2%) with available Pro-BNP measurements (Table 1), the overall median was 655 pg/mL (IQR: 136-2281 pg/mL, range: 10-34,169 pg/ mL). A highly significant difference was observed between survivors and non-survivors: median Pro-BNP levels were 526 pg/mL (IQR: 124-1666 pg/mL) in survivors versus 7194 pg/ mL (IQR: 3684-10,995 pg/mL) in non-survivors, representing an approximately 14-fold difference (Mann-Whitney U test: p = 0.0010) (Table 2, Figure 1A).
The discriminatory ability of Pro-BNP for 30-day mortality was excellent, with an area under the receiver operating characteristic curve (AUC) of 0.854 (95% CI not calculated due to sample size) and a point-biserial correlation coefficient of r_pb = 0.446 (p < 0.001) (Table 3). Furthermore, Pro-BNP levels demonstrated strong correlation with disease severity, as evidenced by significantly higher values in the s-PESI ≥ 1 group (median: 1029 pg/mL, IQR: 322-5506 pg/mL) compared to the s-PESI 0 group (median: 372 pg/mL, IQR: 71-1688 pg/ mL; Mann-Whitney U test: p = 0.027) (Table 2, Figure 1C).
D-Dimer
D-dimer levels were available for 98.8% (n = 86) of patients (Table 1), with a median of 1307 ng/mL (IQR: 900-3205 ng/ mL, range: 128-26,413 ng/mL). While D-dimer levels did not significantly differ between survivors (median: 1266 ng/mL, IQR: 917-3306 ng/mL) and non-survivors (median: 1504 ng/ mL, IQR: 852-2798 ng/mL; p = 0.850) (Table 2), a significant association was observed with disease severity. Patients in the s-PESI ≥ 1 group exhibited substantially higher D-dimer levels (median: 1954 ng/mL, IQR: 1000-5234 ng/mL) compared to the s-PESI 0 group (median: 1071 ng/mL, IQR: 762-2274 ng/mL; Mann-Whitney U test: p = 0.018) (Table 2).
Lactate
Serum lactate was measured in 97.7% (n = 85) of patients (Table 1), yielding a median of 1.70 mmol/L (IQR: 1.20-2.10 mmol/L, range: 0.50-5.50 mmol/L). Although lactate levels showed a trend toward elevation in non-survivors (median: 1.70 mmol/L, IQR: 1.65-1.90 mmol/L) compared to survivors (median: 1.50 mmol/L, IQR: 1.10-2.10 mmol/L), this difference did not achieve statistical significance (p = 0.248). However, lactate demonstrated a significant correlation with disease severity, with higher levels in the s-PESI ≥ 1 group (median: 1.80 mmol/L, IQR: 1.30-2.30 mmol/L) versus the s-PESI 0 group (median: 1.30 mmol/L, IQR: 1.10-1.92 mmol/L; Mann-Whitney U test: p = 0.020) (Table 2).
Troponin
Troponin measurements were available for only 32.2% (n = 28) of patients (Table 1), limiting the interpretability of these findings. Among patients with available data, the median troponin was 0.169 ng/mL (IQR: 0.131-0.275 ng/mL, range: 0.105-1.530 ng/mL). No significant differences were observed between survivors and non-survivors (p = 0.652) or across s-PESI categories (p = 0.890) (Table 2).
Correlation Analysis of Biomarkers
Spearman correlation analysis revealed two significant associations among the evaluated biomarkers. A moderate positive correlation was identified between age and Pro-BNP levels (r = 0.554, p < 0.001, n = 82), suggesting that elevated Pro-BNP in pulmonary embolism may partially reflect age- related cardiovascular changes. Additionally, NLR and PLR demonstrated moderate correlation (r = 0.566, p < 0.001, n = 87), consistent with their shared basis in systemic inflammatory responses.
Demographic Factors and Clinical Outcomes
Age-Stratified Analysis
Mortality rates across age categories were relatively uniform: < 50 years: 11.1% (2/18); 50-65 years: 14.3% (3 / 21); 66-80 years: 11.4% (4 / 35); > 80 years: 15.4% (2 / 13). This lack of a significant age-related mortality gradient (univariate analysis: p = 0.923) contrasts with the strong correlation between age and Pro-BNP, suggesting that age may influence outcomes indirectly through its association with biomarker elevations rather than as an independent risk factor (Table 3).
Discussion
This prospective investigation demonstrates that pro-BNP substantially outperforms conventional risk stratification tools and other biomarkers in predicting 30-day mortality among patients with acute pulmonary embolism. The marked elevation observed in non-survivors, combined with very good discriminatory ability, positions this biomarker as a valuable complement to clinical assessment. These findings align with accumulating evidence regarding the prognostic superiority of natriuretic peptides in acute PE.
Recent large-scale studies have consistently validated NT- proBNP as a prognostic marker in this setting. Singh et al. documented reliable identification of patients at heightened mortality risk, while Becattini et al. assembled data from over 5,000 low-risk PE patients and demonstrated that right ventricular dysfunction assessed by natriuretic peptides carried nearly five-fold increased short-term mortality 15,16. What distinguishes our work is the demonstration that pro-BNP maintains prognostic value across the entire risk spectrum. We observed significant concentration gradients between sPESI risk categories, suggesting this biomarker quantifies right ventricular strain beyond categorical risk grouping alone.
The physiological basis centers on acute right ventricular pressure overload. When pulmonary obstruction reaches critical thresholds, increased wall tension triggers cardiomyocyte release of natriuretic peptides as a compensatory mechanism 5,11. Pro-BNP elevation therefore, reflects hemodynamic compromise severity, underscoring why cardiac dysfunction dominates short-term prognosis compared to markers of thrombus burden or tissue hypoperfusion.
Our findings regarding D-dimer and lactate proved unexpected. Despite a significant elevation in high-risk patients, neither biomarker distinguished survivors from non-survivors. While these results diverge from Keller et al.’s work on D-dimer and thrombus burden, they align with the emerging consensus that D-dimer serves primarily diagnostic rather than prognostic purposes 9. D-dimer reflects thrombus size and fibrinolysis but does not necessarily correlate with hemodynamic impact. Similarly, lactate’s non-specific nature and susceptibility to confounding by sepsis, shock, and organ dysfunction likely limit its standalone prognostic utility 10.
The troponin results warrant careful interpretation, given incomplete data capture in our cohort. While we found no mortality association, this contrasts with established literature demonstrating troponin’s utility in identifying right ventricular injury 7,8. Nithianandan et al.’s systematic review reported that elevated troponin T carried a six-fold increased mortality risk 17. The discrepancy likely reflects limited sample size and temporal variability in presentation timing, as troponin typically peaks 12-48 hours post-embolism. Our findings should not be interpreted as evidence against troponin’s prognostic value.
The complete absence of prognostic signal from inflammatory indices—NLR and PLR—represents perhaps our most surprising observation. This contrasts sharply with recent large-scale studies. Siddiqui and colleagues found that elevated NLR independently predicted mortality in over 10,000 RIETE registry patients, while Babes et al. demonstrated that NLR enhanced PESI and ESC risk classification performance 18,19. Furthermore, Zhu et al. recently validated the Naples prognostic score, which incorporates inflammatory markers, including NLR, as a reliable predictor of 30-day mortality in acute PE 20. The explanation for our divergent findings may lie in population-level differences. Our median NLR remained below prognostic thresholds identified in these larger studies, potentially limiting statistical power. Additionally, ethnic or regional variations in inflammatory responses may contribute to heterogeneous performance across populations 21,22. These observations suggest that while inflammatory markers show promise internationally, their utility requires validation in diverse patient cohorts.
From a clinical perspective, integrating pro-BNP into sPESI-based assessment offers a practical approach to refining risk stratification. The biomarker provides complementary information by quantifying right ventricular compromise within clinical risk strata. This becomes particularly relevant for low- risk patients who might otherwise be considered for outpatient management 3,4. Becattini et al.’s meta-analysis supports this concept, identifying a clinically low-risk subgroup with substantially elevated mortality when RVD is present 16. For intermediate-risk patients, pro-BNP might guide therapeutic decisions, though prospective validation is needed 13.
In summary, this investigation establishes pro-BNP as a highly effective prognostic marker in acute pulmonary embolism, considerably outperforming simplified PESI and other biochemical markers for mortality prediction. The disconnect between our null findings for inflammatory markers and positive results from international registries highlights the importance of population-specific validation 5,6,11. Incorporating pro- BNP into routine risk assessment protocols holds promise for optimizing patient triage and potentially guiding therapeutic decisions in this high-risk population 1,2.
Limitations
This investigation has several methodological considerations that warrant acknowledgement. Our cohort of 87 patients, while adequate for detecting robust pro-BNP associations, imposed constraints on statistical power for biomarkers with incomplete data capture, particularly troponin. The sample size may have been insufficient to detect associations for inflammatory indices, given that our median NLR values fell below prognostic thresholds identified in larger registries. The single-center design raises questions regarding generalizability to populations with different demographic profiles or healthcare systems. Follow-up was limited to 30 days, precluding assessment of longer-term outcomes, including recurrent thromboembolism. Biomarker measurements were performed solely at presentation, without serial sampling to capture dynamic trajectories.
Future work should employ multicenter validation studies with larger cohorts, comprehensive biomarker assessment, serial measurements, and extended follow-up to establish optimal clinical decision thresholds.
Conclusion
This study demonstrates that pro-BNP measurement provides substantial prognostic value in acute pulmonary embolism, considerably outperforming simplified PESI and other evaluated biomarkers. The marked differences between survivors and non-survivors, combined with consistent performance across risk categories, support natriuretic peptide assessment as a practical tool for refining patient stratification. For clinicians making triage decisions, these findings offer practical guidance: pro-BNP can identify patients with occult right ventricular compromise who may need closer monitoring despite appearing low risk by clinical criteria alone, or conversely, help identify those suitable for less intensive management when both clinical and biomarker assessments are reassuring.
Looking forward, integrating pro-BNP into routine assessment protocols could enhance the identification of patients requiring escalated care or those appropriate for shortened hospitalizations. However, the population-specific performance of inflammatory markers observed here underscores an important reality: biomarker thresholds may not universally apply across different populations. Future work should focus on multicenter validation studies, establish optimal pro-BNP cutoffs for clinical decisions, and determine whether biomarker-guided strategies improve patient outcomes. As acute PE management evolves toward individualized approaches, pro-BNP represents a readily available tool with considerable potential to inform clinical decisions and optimize care delivery.
Figures
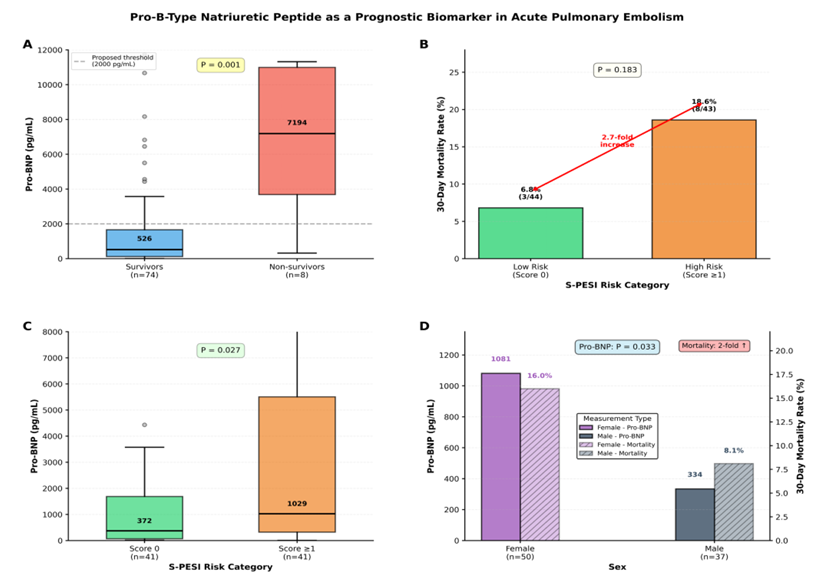
Figure 1. Pro-B-type natriuretic peptide (Pro-BNP) as a prognostic biomarker in acute pulmonary embolism, Pro-BNP levels were higher in 30-day non-survivors, in patients with higher S-PESI scores, and in female patients, who also had higher 30-day mortality Pro-BNP, pro-B-type natriuretic peptide; S-PESI, Simplified Pulmonary Embolism Severity Index
Tables
Table 1. Baseline demographics and clinical characteristics of the study population
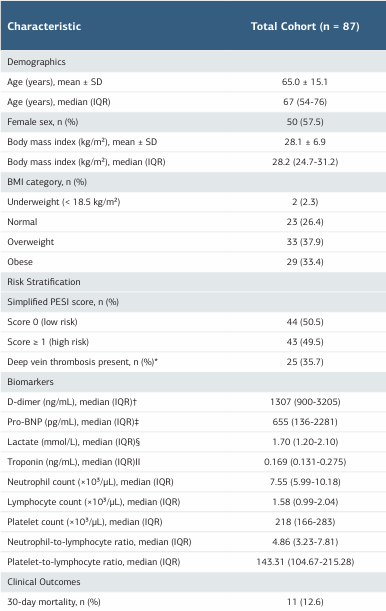
*DVT assessment was not performed or feasible in 17 patients (20.5%); percentages calculated among patients with available data (n = 70). †Available in 86 patients (98.8%). ‡Available in 82 patients (94.2%). §Available in 85 patients (97.7%). Available in 28 patients (32.1%). Abbreviations: BMI = body mass index; DVT = deep vein thrombosis; IQR = interquartile range; PESI = pulmonary embolism severity index; Pro-BNP = pro-B-type natriuretic pep- tide; SD =standard deviation.
Table 2. Biochemical biomarkers according to 30-day mortality status and s-pesi risk categories
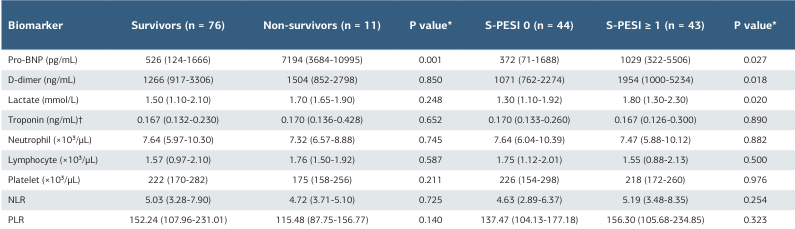
Data presented as median (interquartile range). *Mann-Whitney U test. Bold values indicate statistical significance (P < 0.05). †Troponin data available for only 28 patients (32.1%): survivors n = 21, non-survivors n = 7, S-PESI 0 n = 13, S-PESI ≥ 1 n = 15. Abbreviations: NLR = neutrophil-to-lymphocyte ratio; PLR = platelet-to-lymphocyte ratio; Pro-BNP = pro-B-type natriuretic peptide; S-PESI = simplified pulmonary embolism severity index.
Table 3. Univariate predictive performance of clinical and biochemical parameters for 30-day mortality
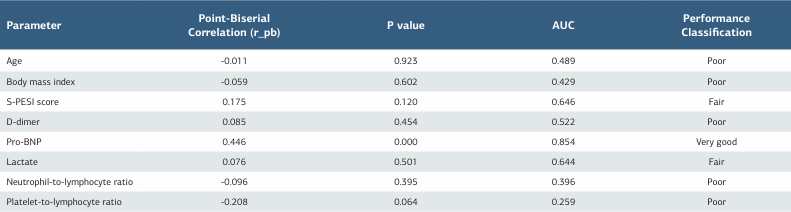
Analysis performed on complete case data (n = 80 patients with all predictors available; 30-day mortality: 10.0%, n = 8). AUC interpretation: 0.90-1.00 = excellent; 0.80-0.90 = very good; 0.70-0.80 = good; 0.60-0.70 = fair; < 0.60 = poor discriminatory ability. Bold values indicate statistical significance (P < 0.05). Abbreviations: AUC = area under the receiver operating characteristic curve; Pro-BNP = pro-B-type natriuretic peptide; S-PESI = simplified pulmonary embolism severity index.
References
-
Goldhaber SZ. Venous thromboembolism: Epidemiology and magnitude of the problem. Best Pract Res Clin Haematol. 2012;25(3):235-42. doi:10.1016/j. beha.2012.06.007.
-
hemodynamically stable pulmonary embolism: Clinical outcome and risk factors in a large prospective cohort study. Chest. 2007;131(2):517-23. doi:10.1378/ chest.05-2799.
-
Jimenez D, Aujesky D, Moores L, et al. Simplification of the pulmonary embolism severity index for prognostication in patients with acute symptomatic pulmonary embolism. Arch Intern Med. 2010;170(15):1383-9. doi:10.1001/archinternmed.2010.199.
-
Masotti L, Panigada G, Landini G, et al. Simplified PESI score and sex difference in prognosis. J Thromb Thrombolysis. 2016;41(4):606-12. doi:10.1007/s11239- 015-1260-0.
-
Klok FA, Mos IC, Huisman MV. Brain-type natriuretic peptide levels in the prediction of adverse outcome in patients with pulmonary embolism: A systematic review and meta-analysis. Am J Respir Crit Care Med. 2008;178(4):425-30. doi:10.1164/rccm.200803-459OC.
-
Cavallazzi R, Nair A, Vasu T, Marik PE. Natriuretic peptides in acute pulmonary embolism: A systematic review. Intensive Care Med. 2008;34(12):2147-56. doi:10.1007/s00134-008-1214-5.
-
Henzler T, Roeger S, Meyer M, et al. Pulmonary embolism: CT signs and cardiac biomarkers for predicting right ventricular dysfunction. Eur Respir J. 2012;39(4):919-26. doi:10.1183/09031936.00088711.
-
Jimenez D, Uresandi F, Otero R, et al. Troponin-based risk stratification of patients with acute nonmassive pulmonary embolism: Systematic review and metaanalysis. Chest. 2009;136(4):974-82. doi:10.1378/chest.09-0608.
-
Keller K, Beule J, Balzer JO, Dippold W, Kahles T, Münzel T. D-Dimer and thrombus burden in acute pulmonary embolism. Am J Emerg Med. 2018;36(9):1613-8. doi:10.1016/j.ajem.2018.01.048.
-
Vanni S, Socci F, Pepe G, et al. High plasma lactate levels are associated with increased risk of in-hospital mortality in acute pulmonary embolism. Acad Emerg Med. 2011;18(8):830-5. doi:10.1111/j.1553-2712.2011.01128.x.
-
Coutance G, Le Page O, Lo T, Hamon M. Prognostic value of brain natriuretic peptide in acute pulmonary embolism. Crit Care. 2008;12(4):R109. doi:10.1186/cc6996.
-
Pruszczyk P, Torbicki A, Kuch-Wocial A, et al. Diagnostic value of transoesophageal echocardiography in suspected haemodynamically significant pulmonary embolism. Heart. 2001;85(6):628-34. doi:10.1136/heart.85.6.628.
-
Sanchez O, Trinquart L, Colombet I, et al. Prognostic value of right ventricular dysfunction in patients with haemodynamically stable pulmonary embolism: A systematic review. Eur Heart J. 2008;29(12):1569-77. doi:10.1093/eurheartj/ ehn208.
-
Kayrak M, Arı H, Alihanoğlu Y, Yazıcı M, Özdemir K. Pulmoner embolinin tetiklediği miyokardiyal iskemi üzerine koroner yavaş akımın etkisi: ST elevasyonlu pulmoner emboli [ The effect of coronary slow flow on myocardial ischemia triggered by pulmonary embolism: ST-elevation pulmonary embolism]. Selçuk Üniv Tıp Derg. 2011;27(1):31-33.
-
Wang Q, Ma J, Jiang Z, et al. Prognostic value of neutrophil-to-lymphocyte ratio and platelet-to-lymphocyte ratio in acute pulmonary embolism: A systematic review and meta-analysis. Int Angiol. 2018;37(1):4-11. doi:10.23736/S0392-9590.17.03848-2.
-
Telo S, Kuluozturk M, Deveci F, Altinsoy B, Cimen P, Yildirim Z. The relationship between platelet-to-lymphocyte ratio and pulmonary embolism severity in acute pulmonary embolism. Int Angiol. 2019;38(1):4-9. doi:10.23736/S0392-9590.18.04028-2.
-
Singh G, Bamba H, Inban P, et al. The prognostic significance of pro-BNP and heart failure in acute pulmonary embolism: A systematic review. Dis Mon. 2024;70(10):101783. doi:10.1016/j.disamonth.2024.101783.
-
Becattini C, Maraziti G, Vinson DR, et al. Right ventricle assessment in patients with pulmonary embolism at low risk for death based on clinical models: an individual patient data meta-analysis. Eur Heart J. 2021;42(33):3190-9. doi:10.1093/eurheartj/ehab329.
-
Nithianandan H, Reilly A, Tritschler T, Wells P. Applying rigorous eligibility criteria to studies evaluating prognostic utility of serum biomarkers in pulmonary embolism: A systematic review and meta-analysis. Thromb Res. 2020;195:195-208. doi:10.1016/j.thromres.2020.07.037.
-
Siddiqui F, Tafur A, Hussain M, et al. The prognostic value of blood cellular indices in pulmonary embolism. Am J Hematol. 2024;99(9):1704-11. doi:10.1002/ ajh.27379.
-
Babes EE, Radu AF, Babeș VV, et al. The prognostic role of hematological markers in acute pulmonary embolism: Enhancing risk stratification. Medicina (Kaunas). 2025;61(6):1095. doi:10.3390/medicina61061095.
-
Zhu N, Lin S, Cao C. A novel prognostic prediction indicator in patients with acute pulmonary embolism: Naples prognostic score. Thromb J. 2023;21(1):114. doi:10.1186/s12959-023-00554-8.
Declarations
Scientific Responsibility Statement
The authors declare that they are responsible for the article’s scientific content, including study design, data collection, analysis and interpretation, writing, and some of the main line, or all of the preparation and scientific review of the contents, and approval of the final version of the article.
Animal and Human Rights Statement
All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Funding
None
Conflict of Interest
The authors declare that there is no conflict of interest.
Ethics Declarations
This study was approved by the Necmettin Erbakan University Non-Drug and Medical Device Research Ethics Committee (Date: 2020-06-06, No: 2020/2577)
Data Availability
The datasets used and/or analyzed during the current study are not publicly available due to patient privacy reasons but are available from the corresponding author on reasonable request.
Additional Information
Publisher’s Note
Bayrakol MP remains neutral with regard to jurisdictional and institutional claims.
Rights and Permissions
About This Article
How to Cite This Article
Abdurrahman Koc, Hulya Vatansev. Prognostic Relevance of Biochemical Markers Integrated with Simplified Pulmonary Embolism Severity Index in Acute Pulmonary Embolism. Ann Clin Anal Med 2025;16(12):893-898
Publication History
- Received:
- April 10, 2025
- Accepted:
- May 19, 2025
- Published Online:
- June 20, 2025
- Printed:
- December 1, 2025

