Evaluation of lumbar plexus block success in lower extremity surgeries using near infrared spectroscopy (NIRS)
Evaluation of lumber plexus block success
Authors
Abstract
Aim Near Infrared Spectroscopy (NIRS) can determine regional oxygen saturation (rSO2). Studies have shown that rSO2 values increase following a successful peripheral nerve block. This study aimed to evaluate the effectiveness of NIRS in determining the success of lumbar and sacral plexus blocks.
Methods Sixty-five patients undergoing lumbar and sacral plexus blocks for lower extremity orthopedic surgery were included. The primary outcome was rSO2 values measured in both lower extremities using NIRS (preoperative and post-block at 5, 10, 15, 20, 25, and 30 minutes). Secondary outcomes included the pinprick test (at 5, 10, 15, 20, 25, and 30 minutes), as well as SPI, Response Entropy (RE), and State Entropy (SE) measurements recorded before the block and at 5, 10, 15, 20, 25, 30, 60, 90, and 120 minutes post-block, along with anesthesia duration.
Results At all time points, both the rSO2 values and their percentage increases were significantly higher on the blocked extremity compared to the unblocked side (p < 0.001). Cut-off values for predicting successful peripheral block based on the initial rSO2 values were: 6.25% at 5 minutes; 8.75% at 10 minutes; 8.97% at 15 minutes; 10.14% at 20 minutes; 10.14% at 25 minutes; and 10% at 30 minutes.
Conclusion rSO2 measurements using NIRS demonstrated high sensitivity, specificity, and predictive value for determining block success.
Keywords
Introduction
Peripheral nerve blocks, alongside spinal and epidural anesthesia techniques, are frequently employed for lower extremity surgeries. Their ability to reduce cardiovascular depression, maintain spontaneous respiration, and provide effective postoperative analgesia has contributed to their increased usage 1. Despite this, block failure rates for regional anesthesia can range between 6% and 20%, even among experienced practitioners, depending on the technique and type of surgery 2.
Several methods exist for assessing block success, but there is no definitive consensus on the most effective technique 3. A successful peripheral nerve block typically results in a sequential sympathetic, sensory, and motor block 3. Commonly used methods to assess block success include evaluating temperature sensation, pain, light touch, and motor movement within the relevant dermatome (e.g., pinprick test, Bromage scale). However, these traditional tests are subjective and can vary significantly between assessors 3,4. The demand for more objective, quantifiable data has encouraged exploration of alternative approaches. NIRS is a non-invasive technology that measures regional tissue oxygenation 5. Studies have indicated that rSO2 values increase after a successful peripheral nerve block 6,7.
The hypothesis of this study was that rSO2 values would rise on the side where the block was applied. To test this, we conducted bilateral lower extremity rSO2 measurements in patients undergoing combined lumbar and sacral plexus blocks for orthopedic procedures. The effectiveness of these measurements was compared against the pinprick test.
Materials and Methods
Patients aged 18–90 years scheduled for femoral neck fracture repair or hip prosthesis between November and December 2023 were eligible, provided they were classified as ASA I–III and gave informed consent for lumbar and sacral plexus blocks. Exclusion criteria: Contraindications for lumbar and sacral plexus block were body mass index (BMI) > 40 kg/square meter (kg/m2), local infection findings in the block area, peripheral neuropathy, hemoglobinopathy or peripheral vascular disease, allergy to local anesthetics, and presence of contraindications for lumbar and sacral plexus block.
Study Protocol
Detailed information about the anesthesia method to be applied and the study to be conducted was provided to patients who were to undergo elective surgery. Written informed consent documents were prepared for patients who accepted the study and were signed by the patients. After standard electrocardiogram monitoring, peripheral oxygen saturation (SpO2), and noninvasive blood pressure monitoring were performed in the operating room, vascular access was established with two 18-to 20-gauge intravenous catheters. A crystalloid infusion was administered at 2-3 milliliters (ml)/kg per hour. Entropy sensors were applied to the forehead for RE and SE monitoring (Datex-Ohmeda® E-Entropy Module, GE). Patients received IV midazolam (0.01–0.02 mg/kg) and fentanyl (0.5–1 mcg/kg) for premedication. Two NIRS sensors (INVOS™ 5100C®, Covidien) were placed at a level approximately equal to the midline on the musculus quadriceps femoris of each leg after skin cleaning with alcohol. Baseline values for rSO2, SPI, RE, and SE were recorded before the block.
The pinprick test was performed using a 22 Gauge needle tip, with a binary scoring system (0 = pain or touch perceived; 1 = no sensation) (available at: http://dx.doi.org/10.7759/cureus.80211). Patients were handed over to the surgical team at the 30th minute following the block procedure.
Block Application
Patients were positioned laterally with the operative limb uppermost. After antiseptic preparation, a convex ultrasound probe (Esaote My Lab 30 Gold, Convex probe, 1-8 megahertz) was used for lumbar plexus block (shamrock technique) and sacral plexus block (parasacral parallel shift technique) placement. A 21-G, 100-mm nerve block needle and nerve stimulator (Stimuplex® HNS 12, B. Braun) guided the injections. Lumbar plexus blocks used 20–30 ml of 0.5% bupivacaine; sacral blocks used 15–20 ml of 0.5% bupivacaine.
The volume of bupivacaine used for each patient was determined based on individual factors, including patient weight, surgical site requirements, and ultrasound visualization quality. The goal was to ensure adequate anesthesia while minimizing potential toxicity.
Outcomes Measurements
Primary outcome: rSO2 values measured via NIRS at pre-block and at 5, 10, 15, 20, 25, and 30 minutes post-block.
Secondary outcomes: Pinprick scores at corresponding time points, SPI and Entropy values (RE/SE) before block and at 5, 10, 15, 20, 25, 30, 60, 90, and 120 minutes post-block, and total anesthesia time.
Block success was defined as a complete sensory and motor blockade in the surgical extremity within 30 minutes. In cases of incomplete blockade, supplemental nerve blocks were considered but were not performed in this study.
Statistical Analysis
The statistical analyses of the study were performed using SPSS 28, MedCalc 22.009 Demo and R-Studio 1.4.1103 package programs. Descriptive statistics of the quantitative variables included in the study are shown with mean, standard deviation, median, minimum and maximum values, and qualitative variables are shown with frequency and percentage. The conformity of quantitative variables to normal distribution was examined with the Shapiro Wilk test. If the quantitative variables showed normal distribution, the independent sample t test was used, and if they did not show normal distribution, the Mann Whitney U test was used. When evaluating the changes in repeated measurements of quantitative variables, if they showed normal distribution, the variance analysis in repeated measurements was used, and if they did not show normal distribution, the Friedman test was used. For significant changes in repeated measurements, subgroup comparisons were conducted using Bonferroni post-hoc tests. ROC analysis was performed to determine whether the “ rSO2 Percentage Change ” variables had a distinctiveness in predicting block success, and cut-off values were obtained for variables related to the Youden index. Yates chi-square, Fisher chi-square, and Fisher-Freeman-Halton chi-square tests were used to compare qualitative variables between groups. In all statistical analyses of the study, p-values less than 0.05 were considered statistically significant.
Power Analysis
In our pilot study conducted on 10 patients, we determined the mean rSO2 values as 75.6 ± 8.8. To detect an approximately 10% increase in rSO2 values, which is the primary outcome measure of this study, the required sample size was determined as 54 patients with 85% power (α = 0.05). Considering the possible losses, a total of 65 patients were planned to be included in the study. The G power program was used to calculate the sample size of the study.
Ethical Approval
This study was approved by the Ethics Committee of Bursa Yuksek Ihtisas Training and Research Hospital Ethics Committee (Date: 2022-06-15, No: 2011-KAEK-25 2022/06-05).
Results
Our study included 65 patients who underwent combined lumbar and sacral plexus block for lower extremity orthopedic surgery. Four patients were excluded from the study due to missing data and one patient was subsequently switched to a different anesthesia method. Statistical analysis was performed on the remaining 60 patients. Demographic and clinical data are shown in Table 1.
Values are presented as mean ± SD, median (minimum – maximum) or number (%). ASA-PS: American Society of Anesthesiologists physical status classification.
Of the patients enrolled in the study, only one required conversion to an alternative anesthetic technique after the block. No supplementary analgesia or sedation was needed intraoperatively in the other patients.
rSO2 values in the blocked extremity were significantly higher than in the unblocked extremity at all measurement times (p < 0.001) (Figure 1). It was found that the rSO2 change between the 0th and 30th minutes of the blocked extremities was statistically significant (p < 0.001). While all rSO2 value changes before and at the 20th minute of the change were significant (p < 0.05), no significant rSO2 change was found after the 20th minute (p > 0.05). When the percentage changes in the rSO2 values measured from the blocked and unblocked extremities were examined, it was found to be statistically significant, being higher on the blocked side (p < 0.001) (Table 2).
The sensitivity, specificity, negative predictive value and positive predictive value of rSO2 percentage changes in the extremities where block was applied in predicting block success are shown in Table 3. Percentage changes in rSO2 values in the extremities where block was applied were examined with the Youden index cut-off value between the pinprick test during the first 30 minutes, and the sensitivity and specificity values at the 25th minute after the block were found to be 10.00 ≤ with a cut-off value of 100.0% (CI [Confidence Interval] 87.2% - 100.0%) sensitivity and 100.0% (CI 89.4% - 100.0%) selectivity. The area under the curve (AUC = Area Under Curve) for the relevant cut-off point is 1.000 and is statistically significant (p < 0.001) (Figure 2 and Figure 3). No statistically significant difference was found between the patients' initial SPI, RE, SE values and the SPI, RE, SE values recorded after the block and during the operation
Discussion
This study demonstrates that NIRS-measured rSO2 values can accurately indicate block success. rSO2 increases were significantly higher on the blocked side, consistent with sympathetic blockade-induced perfusion changes.
When we look at the current definitions of regional anesthesia failure, it is seen that failure is mostly detected after surgical stimulation and anesthesiologists do not have objective data that can be used as a warning beforehand. Pinprick test, cold test and bromage scale are used to evaluate block success (available at: http://dx.doi.org/10.7759/cureus.80211). There are studies in the literature comparing these methods that provide subjective data with different methods that provide more quantitative data. For this purpose, it is stated in the literature that tools such as NIRS, perfusion index, and thermography are used to observe the effects of sympathetic block after regional anesthesia and before surgery begins (available at: http://dx.doi.org/10.7759/cureus.80211) 1,8. A study comparing pinprick and cold sensation tests to evaluate the success of USG-guided supraclavicular brachial plexus block showed that perfusion index predicted successful blocks with 100% sensitivity and 100% sensitivity and specificity at 10 minutes (available at: http://dx.doi.org/10.7759/cureus.80211). In this study, authors reported that perfusion index values are reliable early indicators of block success.
On the other hand, when peripheral nerve blockade is successful, sympathetic blockade and increased blood flow are reported in the literature (available at: http://dx.doi.org/10.7759/ cureus.80211). The changes in tissue oxygenation caused by this situation can be detected by tissue spectrophotometry. NIRS devices are devices that are available for this purpose and can be used in different body parts and areas 9. Karahan et al. also applied infraclavicular brachial plexus block to 40 patients in a study and evaluated the results with NIRS. In the study, the initial rSO2 values of the extremity that was blocked and the extremity that was not blocked were found to be similar, but it was observed that the rSO2 values of the blocked extremity were significantly higher in the measurements made from the 5th minute after the block. The rSO2 value, which was 83% at the beginning, was determined to be 89% at the end of the 30th minute, and they reported the rSO2 increase as 5.5% at the end of the 30th minute 1. 40 patients were included in another study cervical paravertebral, infraclavicular and femoral nerve blocks were applied. rSO2 values were observed with a NIRS device connected to the extremities with and without block. A significant increase in rSO2 values was detected in all extremities with block 7.
In the study conducted by Zou et al., in which a total of 48 patients who underwent lumbar plexus block, fascia iliaca block, and femoral nerve block were examined, rSO2 values of the middle and distal parts of the thigh were measured with the NIRS device. The specificity and sensitivity of these values were again compared with the pinprick. At the end of the 15th minute, it was found that the rSO2 value of the medial part of the thigh had 69.2% sensitivity and 100% specificity, while the pinprick test had 80% sensitivity and 80% specificity. Zou et al. determined a cut-off point for the rSO2 value of the medial part of the thigh at the 3rd, 6th, 9th, 12th and 15th minutes and stated that the rSO2 measurement was a reliable indicator of successful block 6.
This study also examined SPI and entropy as objective pain indicators. There are studies conducted on patients who received general anesthesia and sedoanalgesia regarding the use of SPI for objectıve assessment of pain (available at: http://www.ncbi. nlm.nih.gov/pubmed/30198405) 10. In the study conducted by Hamunen et al. the mean SPI value was 66.8 ± 11.8 in 34 fully awake and healthy male volunteers during the period when the feeling of pain was minimal or absent ıt is seen as 11. In the study by Bossolasco et al. patients who underwent endoscopic intervention under sedation were divided into two groups according to the drugs given for sedation and SPI values were recorded. The mean SPI values for both groups were found to be 72.8 and 74.9 12. Entropy, which is another measurement method, has also been shared in the literature that it can be used in the objective assessment of pain. There are studies showing that the difference between RE and SE values can be used as an indicator of facial electromyography 13. In a meta- analysis, it was noted that the difference between RE and SE may exceed 10 units following nociceptive stimulation, and that a greater RE-SE difference could indicate an increased need for anesthetic depth. The authors also suggested that the RE- SE gap might be used as a parameter for pain monitoring 14. In our study results, the minimal changes and levels in SPI and Entropy follow-up values after block application support the accuracy of rSO2 measurements in showing block success.
Limitations
There are certain limitations in our study. The most important of these is that, although the patients were standardized, rSO2 measurements performed with NIRS may be affected by differences in subcutaneous fat tissue thickness and vascular structure at the measurement site [15]. Another important limitation is that our patient population is in an advanced age group, has relatively fragile characteristics, and may experience communication difficulties after premedication.
Conclusion
In conclusion, it was determined that the data obtained from the NIRS application in determining successful peripheral nerve blockade provided more accurate results in terms of sensitivity, specificity, positive and negative predictive value compared to the data obtained from the pinprick test. In this study, data on the use of NIRS technology in the evaluation of block success, especially in patients with advanced age and mental retardation, are presented. In order to apply our findings more generally and widely, comprehensive studies including larger and different patient groups are needed. Such studies are important to ensure the applicability of our findings to a wider patient population.
Figures
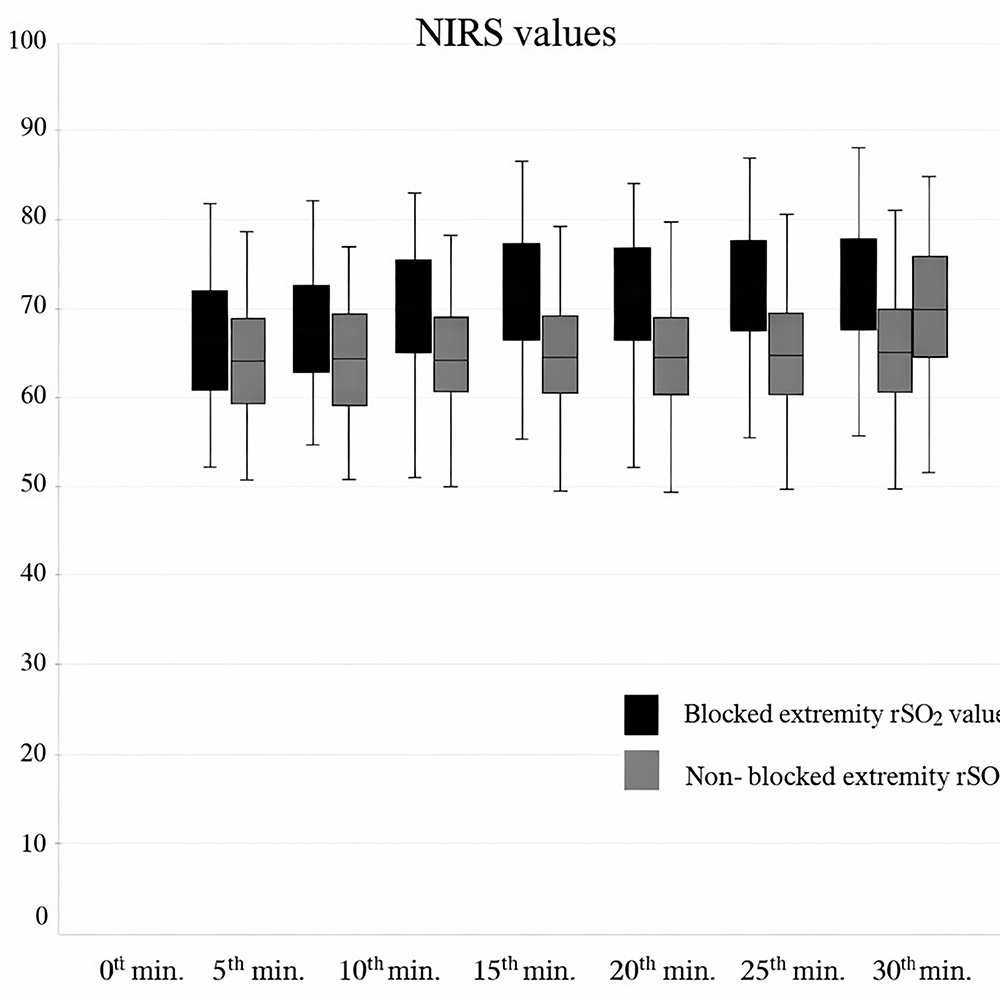
Figure 1. rSO2 values at measurement times
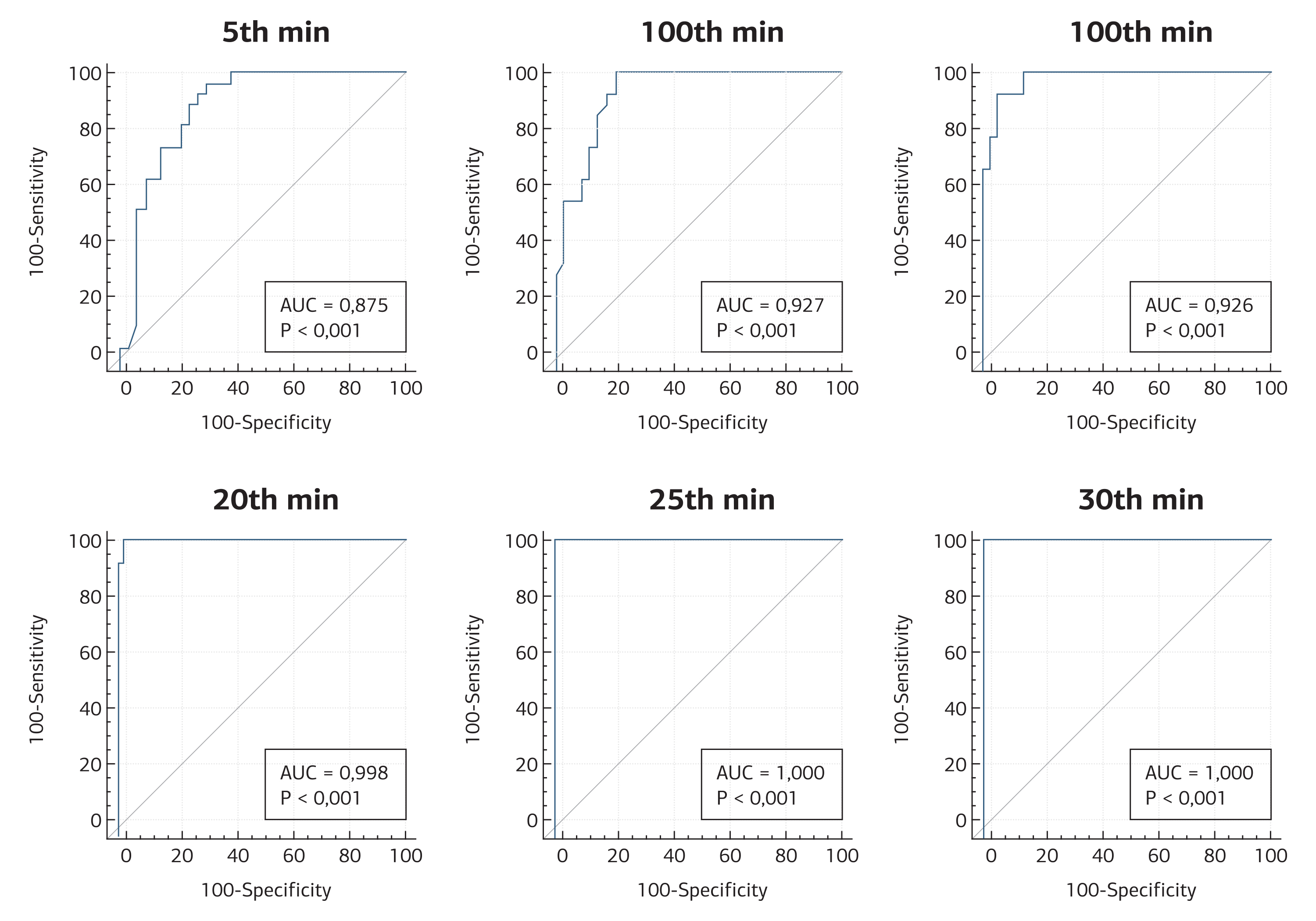
Figure 2. Receiver operating characteristic (ROC) analysis for cut-off value
Cut-off point values of rSO2 percentage changes in the extremities where the block was applied
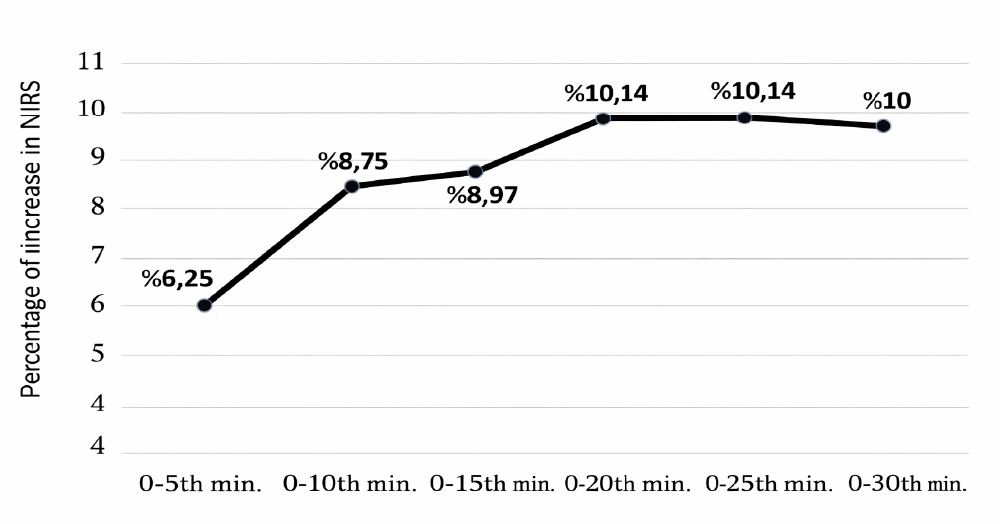
Figure 3
Tables
Table 1. Demographic, anesthesia and surgical data of patients
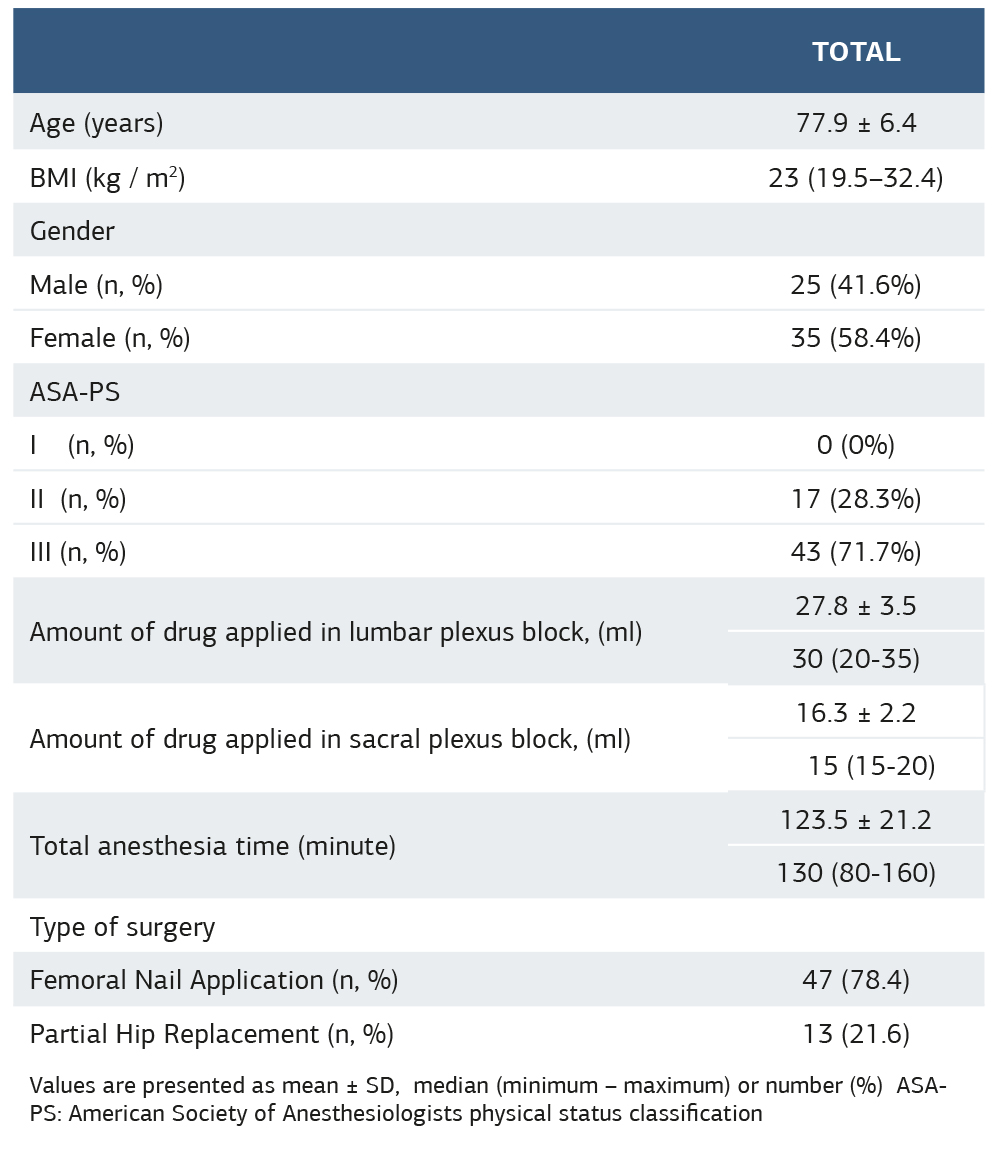
Values are presented as mean ± SD, median (minimum – maximum) or number (%) ASA- PS: American Society of Anesthesiologists physical status classification
Table 2. Comparison of percentage changes in rSO2 values in blocked extremities
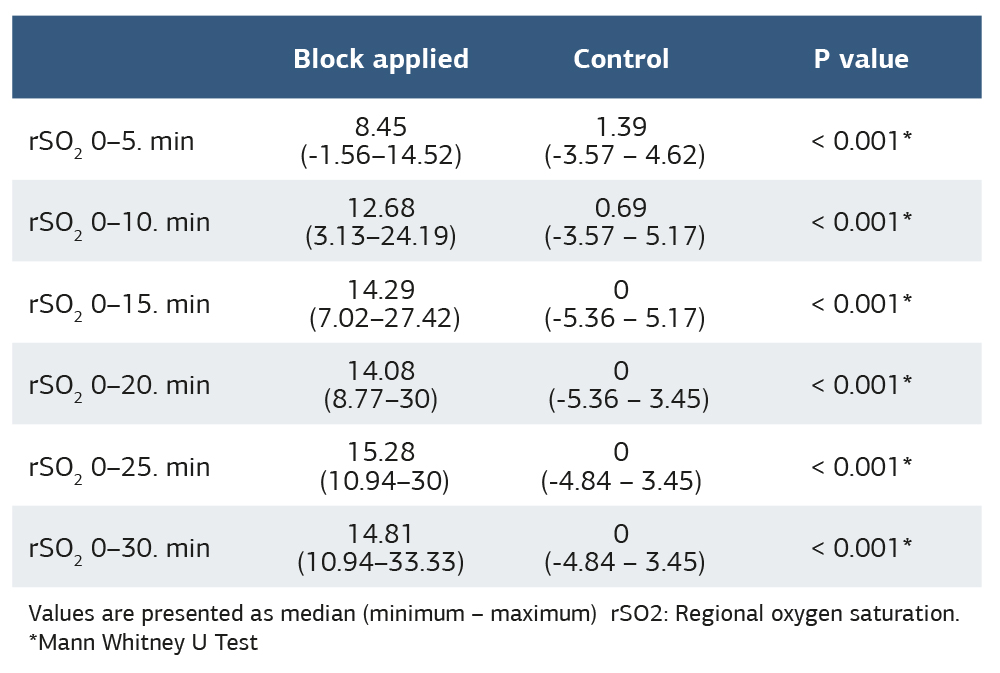
Values are presented as median (minimum – maximum) rSO2: Regional oxygen saturation. *Mann Whitney U Test
Table 3. rSO2 in predicting block success
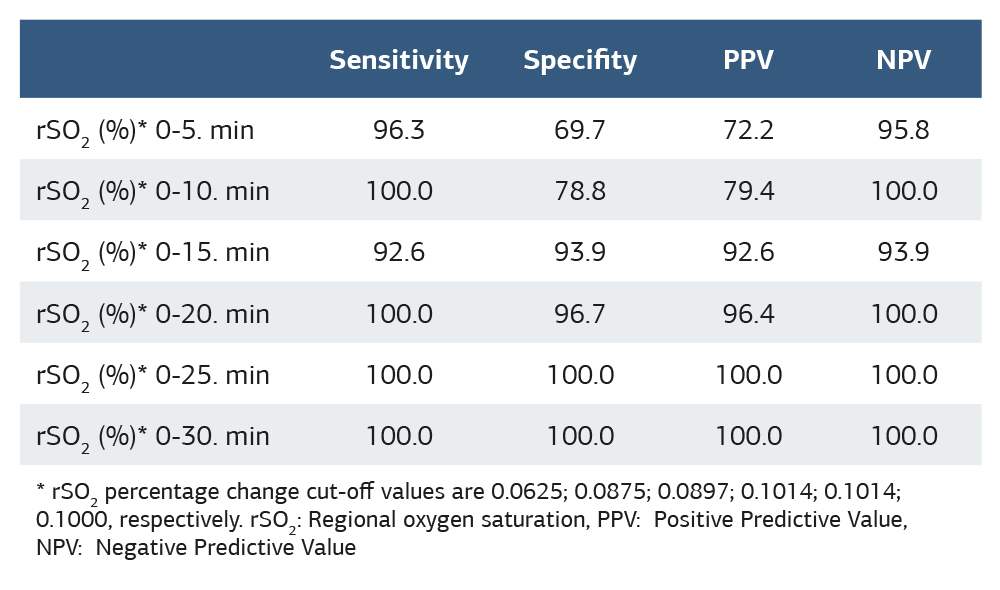
* rSO2 percentage change cut-off values are 0.0625; 0.0875; 0.0897; 0.1014; 0.1014; 0.1000, respectively. rSO2: Regional oxygen saturation, PPV: Positive Predictive Value, NPV: Negative Predictive Value
References
-
Karahan MA, Binici O, Büyükfırat E. Tissue oxygen saturation change on upper extremities after ultrasound-guided infraclavicular brachial plexus blockade: prospective observational study. Medicina (Kaunas). 2019;55(6):274. doi:10.3390/medicina55060274.
-
Picard L, Belnou P, Debes C, et al. Impact of regional block failure in ambulatoryh and surgery on patient management: a cohort study. J Clin Med. 2020;9(8):2453. doi:10.3390/jcm9082453.
-
Bottomley T, Gadsden J, West S. The failed peripheral nerve block. BJA Educ. 2023;23(3):92-100. doi:10.1016/j.bjae.2022.12.002.
-
Ode K, Selvaraj S, Smith AF. Monitoring regional blockade. Anaesthesia. 2017;72(Suppl 1):70-5. doi:10.1111/anae.13742.
-
Moerman A, Wouters P. Near-infrared spectroscopy (NIRS) monitoring in contemporary anesthesia and critical care. Acta Anaesthesiol Belg. 2010;61(4):185-94.
-
Zou Y, Tang Z, Ahn W, et al. Increase in regional oxygen saturation in the thigh indicates successful block of the femoral nerve after lumbar plexus block. Br J Anaesth. 2018;121(4):973-4. doi:10.1016/j.bja.2018.03.036.
-
Tighe PJ, Elliott CE, Lucas SD, Boezaart AP. Noninvasive tissue oxygen saturation determined by near-infrared spectroscopy following peripheral nerve block. Acta Anaesthesiol Scand. 2011;55(10):1239-46. doi:10.1111/j.1399- 6576.2011.02533.x.
-
Zhang S, Liu Y, Liu X, Liu T, Li P, Mei W. Infrared thermography for assessment of thoracic paravertebral block: a prospective observational study. BMC Anesthesiol. 2021;21(1):168. doi:10.1186/s12871-021-01389-4.
-
Pisano A, Di Fraja D, Palmieri C. Monitoring cerebral oximetry by near-infrared spectroscopy (NIRS) in anesthesia and critical care: progress and perspectives. In: Cascella M, editor. General anesthesia research. New York, NY: Humana Press; 2020:75-96.
-
Oh SK, Won YJ, Lim BG. Surgical pleth index monitoring in perioperative pain management: usefulness and limitations. Korean J Anesthesiol. 2024;77(1):31-45. doi:10.4097/kja.23158.
-
Hamunen K, Kontinen V, Hakala E, Talke P, Paloheimo M, Kalso E. Effect of pain on autonomic nervous system indices derived from photoplethysmography in healthy volunteers. Br J Anaesth. 2012;108(5):838-44. doi:10.1093/bja/aes001.
-
Bossolasco M, Olivero F, Palmisano S, Manassero A, Coletta G. Surgical pleth index to evaluate analgesia during esophagogastroduodenoscopy (EGD) procedures: 3AP5-2. Eur J Anaesthesiol. 2011;28:37-8. doi:10.1097/00003643-201106001-00115.
-
Ajayan N, Hrishi AP, Mathew O, Saravanan G. Evaluation and correlation of nociceptive response index and spectral entropy indices as monitors of nociception in anesthetized patients. J Neurosci Rural Pract. 2023;14(3):440-6. doi:10.25259/JNRP_75_2023.
-
He B, Zhang N, Peng M. Meta-analysis of the effect of entropy-assisted general anesthesia on the quality of postoperative recovery. Medicine (Baltimore). 2023;102(25):e34091. doi:10.1097/MD.0000000000034091.
-
Mizukoshi K, Hamanaka Y, Niwayama M. Investigation of oxygen saturation in regions of skin by near infrared spectroscopy. Skin Res Technol. 2022;28(5):695-702. doi:10.1111/srt.13169.
Declarations
Scientific Responsibility Statement
The authors declare that they are responsible for the article’s scientific content, including study design, data collection, analysis and interpretation, writing, and some of the main line, or all of the preparation and scientific review of the contents, and approval of the final version of the article.
Animal and Human Rights Statement
All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Funding
None
Conflict of Interest
The authors declare that there is no conflict of interest.
Ethics Declarations
This study was approved by the Ethics Committee of Bursa Yuksek Ihtisas Training and Research Hospital (Date: 2022-06-15, No: 2011-KAEK-25 2022/06- 05)
Data Availability
The datasets used and/or analyzed during the current study are not publicly available due to patient privacy reasons but are available from the corresponding author on reasonable request.
Additional Information
Publisher’s Note
Bayrakol MP remains neutral with regard to jurisdictional and institutional claims.
Rights and Permissions
About This Article
How to Cite This Article
Gürcan Güler, Korgün Ökmen, Buket Özyaprak, Mehmet Gamlı, Ahsen Gür Çelik, Damla Bozan Güler, Şule Balk Uçar, Evaluation of lumbar plexus block success in lower extremity surgeries using near ınfrared spectroscopy (NIRS). Ann Clin Anal Med 2026;17(2):125-129
Publication History
- Received:
- April 11, 2025
- Accepted:
- May 19, 2025
- Published Online:
- June 23, 2025
- Printed:
- February 1, 2026

