The prognostic impact of 18F-FDG PET SUVmax in patients with non-small cell lung cancer
SUVmax in patients with non-small cell lung cancer
Authors
Abstract
Aim The maximum standardized uptake value (SUVmax) of 18F-fluorodeoxyglucose positron emission tomography (18F-FDG PET) enhances clinical prediction in non-small cell lung cancers (NSCLC). This study aimed to investigate whether SUVmax could serve as a prognostic factor and improve clinical prognostication.
Methods This retrospective study included 86 patients with NSCLC who underwent surgical resection. Using receiver operating characteristic (ROC) analysis, the SUVmax cut-off value was 12.3. Patients with SUVmax values below 12.3 were classified as Group A, while those with values above 12.3 were designated as Group B. Survival analyses were performed using the Kaplan–Meier method. Overall survival was defined as the time from diagnosis to death. Confidence intervals were reported at 95%, and a p-value of <0.05 was considered statistically significant. The variables analyzed for survival included gender, age, surgical approach, histopathological subtype of lung cancer, cancer stage, T score, and N score.
Results Survival analyses revealed statistically significant associations between SUVmax and age (p=0.043), gender (p=0.060), surgical approach (p=0.037), and histopathological subtype (p=0.026). Due to insufficient sample size within subgroups, separate p-values were calculated for each stage, T score, and N score. Based on the obtained p-values, no statistically significant correlation was found between SUVmax and overall survival across different stages, T scores, or N scores, except for stage 1A and T1b.
Conclusion SUVmax contributes to determining appropriate diagnostic and treatment protocols and aids in predicting the prognosis of the disease.
Keywords
Introduction
Lung cancer is the most frequently diagnosed malignancy in men and ranks third in women worldwide. It is the leading cause of cancer-related mortality in men and the second most common cause in women.1 Non-small cell lung cancer (NSCLC) accounts for approximately 14% of all lung cancer cases.2 Due to the persistently low long-term survival rates in patients with lung cancer, there remains a critical need for improved preventive strategies, earlier diagnostic methods, and the development of novel therapeutic approaches.
In recent years, semi-quantitative parameters obtained through 18F-fluorodeoxyglucose positron emission tomography (18F-FDG PET) have emerged as valuable prognostic markers in NSCLC, reflecting the glucose metabolism of primary tumors.3 The maximum standardized uptake value (SUVmax) is the most commonly utilized parameter in PET/CT imaging. Unlike immunohistochemical analysis, SUVmax can serve as a prognostic indicator even in the absence of surgical tissue samples. Indeed, several studies have demonstrated a correlation between elevated SUVmax values and poorer overall survival outcomes.4,5
In this study, we aimed to investigate the prognostic significance of SUVmax derived from 18F-FDG PET/CT imaging in patients with non-small cell lung cancer.
Materials and Methods
Patient Population
This retrospective study included 86 patients who underwent surgical resection and were diagnosed with non-small cell lung cancer (NSCLC). Staging was performed in accordance with the 8th edition of the TNM classification system, as recommended by the International Association for the Study of Lung Cancer (IASLC). Preoperative SUVmax values obtained from 18F-FDG PET/CT scans were recorded for all patients.
Variables analyzed in this study included age, sex, surgical approach, histopathological subtype of lung cancer, clinical stage, T stage, and N stage. Patients with confirmed infections or with acute or chronic pneumonia were excluded from the study. Additionally, patients with a postoperative follow-up period shorter than three years were not included. Survival time was calculated as the interval from the date of diagnosis to the date of death.
Due to the limited sample size, the statistical power for advanced subgroup analyses may be restricted, and interpretations were made with caution in this context. Furthermore, given the retrospective nature of the study, data completeness may vary; thus, it is emphasized that these findings should be supported by multicenter, prospective studies to ensure greater reliability and generalizability.
18F-FDG PET/CT Imaging Analysis
PET/CT scans of the patients were obtained using a Siemens Biograph mCT S(20) 3R (Knoxville, TN, USA) scanner. Images acquired in coronal, sagittal, and transverse planes were evaluated using the Syngo.via VB10B software (Siemens Medical Solutions Inc.). All images were independently assessed by a nuclear medicine specialist. Patients with contrast agent allergies were excluded from the study.
Statistical Analysis
Statistical analyses were performed using SPSS version 25.0 (Statistical Package for the Social Sciences). Preoperative SUVmax values were recorded for all patients. Receiver Operating Characteristic (ROC) curve analysis was used to determine the optimal cut-off value for SUVmax that provided the highest sensitivity and specificity. Kaplan–Meier survival analysis was employed to assess survival outcomes. Survival time was defined as the duration from diagnosis to death. Confidence intervals were set at 95%, and a p-value of < 0.05 was considered statistically significant.
Ethical Approval
This study was approved by the Ethics Committee of the Inonu University Scientific Research and Publication Ethics Board (Date: 2020-09-29, No: 2020/940).
Reporting Guidelines
This study was reported in accordance with the STROBE guidelines.
Results
Patient Population
A total of 86 patients who underwent surgical resection for non-small cell lung cancer (NSCLC) in our clinic between 2010 and 2017 were included in the study. The mean age of the cohort was 60.9 years (range: 35–83). The mean age of male patients was 61.2 years (range: 35–83), while the mean age of female patients was 58.7 years (range: 38–76). Among the 86 patients who underwent anatomical resection (lobectomy, bilobectomy, or pneumonectomy), 47 (54.6%) underwent surgery via right-sided approaches and 39 (45.4%) via left-sided approaches. Video-assisted thoracoscopic surgery (VATS) was performed in 28 patients (32.6%), whereas thoracotomy was used in 51 patients (59.3%). The clinical characteristics of the patients are summarized in Table 1.
Determination of Cut-off Value
Preoperative SUVmax values were recorded for all patients. Receiver Operating Characteristic (ROC) curve analysis was performed to determine the SUVmax value that provided the best balance of sensitivity and specificity. According to the ROC analysis, SUVmax had a sensitivity of 84.4% and a specificity of 40.7%. The determined cut-off value for SUVmax was 12.3 (AUC: 0.603; 95% CI: 0.483–0.723; p = 0.112).
Based on this threshold, patients were categorized into two groups: Group A (SUVmax < 12.3), consisting of 27 patients (21 males, 6 females), and Group B (SUVmax > 12.3), consisting of 59 patients (54 males, 5 females).
Survival Findings
In patients under 64.5 years of age, the mean overall survival was 71.4 months in Group A (95% CI: 56.5–86.3; p = 0.043) and 44.5 months in Group B (95% CI: 34.3–54.8; p = 0.043). Among patients aged 64.5 years and above, the mean survival was 51.6 months in Group A (95% CI: 31.9–71.3; p = 0.043) and 39.7 months in Group B (95% CI: 28.5–51.0; p = 0.043). A statistically significant difference in overall survival was observed between Groups A and B in relation to age (p = 0.043). Accordingly, overall survival was higher in both age subgroups (< 64.5 and ≥ 64.5 years) within Group A (SUVmax < 12.3), whereas overall survival was lower in both subgroups within Group B (SUVmax > 12.3) (Figure 1A-1B).
In male patients, the mean overall survival was 61.3 months in Group A (95% CI: 45.9–76.7; p = 0.060) and 42.8 months in Group B (95% CI: 34.2–51.4; p = 0.060). Among female patients, the mean overall survival was 60.1 months in Group A (95% CI: 60.1–60.1; p = 0.060) and 55.4 months in Group B (95% CI: 53.0–57.8; p = 0.060). No statistically significant difference in survival was observed between Groups A and B based on gender (p = 0.060). These findings suggest that overall survival rates were similar between male and female patients in both Group A and Group B (Figure 2A-2B).
Among patients who underwent posterolateral thoracotomy, the mean overall survival was 60.8 months in Group A (95% CI: 43.4–78.3; p = 0.037) and 46.6 months in Group B (95% CI: 36.1–57.2; p = 0.037). For patients who underwent video-assisted thoracoscopic surgery (VATS), the mean overall survival was 64.0 months in Group A (95% CI: 42.5–85.5; p = 0.037) and 40.7 months in Group B (95% CI: 28.3–53.0; p = 0.037).
A statistically significant difference in survival was observed between Groups A and B when stratified by surgical approach (p = 0.037). In Group A, patients who underwent VATS demonstrated better overall survival compared to those who underwent thoracotomy. However, in Group B, the higher survival observed in thoracotomy patients was interpreted as favoring that approach.
When evaluated based on histopathological subtypes, a statistically significant association was observed between overall survival and SUVmax groups (Group A and Group B) in patients with adenocarcinoma and squamous cell carcinoma (p = 0.026). Specifically, patients in Group A exhibited higher overall survival in both adenocarcinoma and squamous cell carcinoma subtypes, whereas survival was lower in Group B for the same histological types (Figure 3).
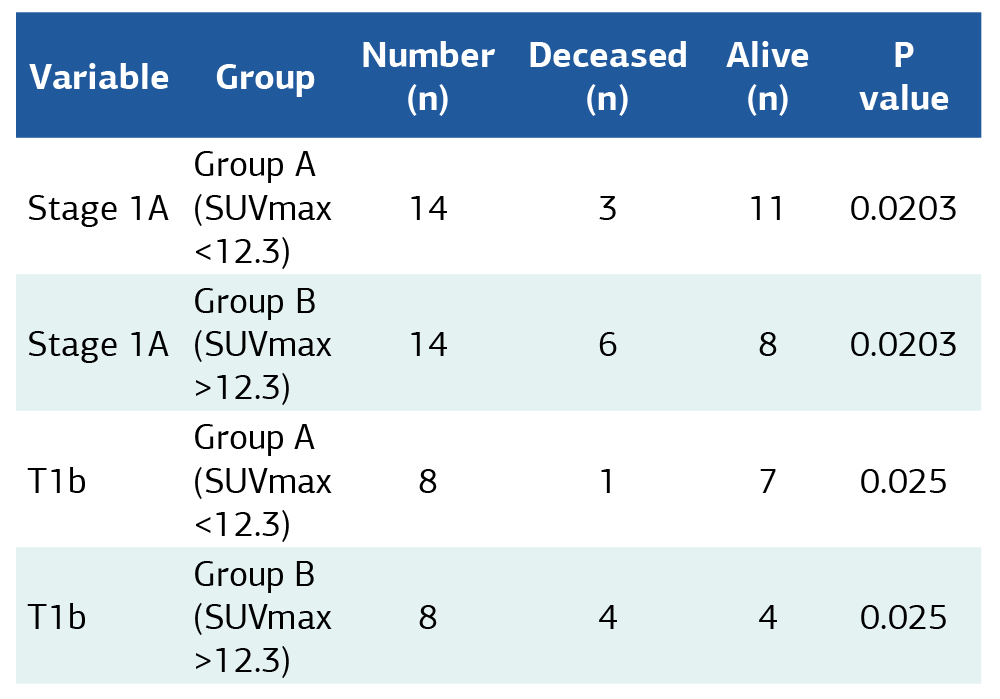
When analyzing the association between SUVmax and overall survival across all clinical stages, T scores, and N scores, separate p-values were calculated for each subgroup due to the limited number of patients (Table 2). According to these p-values, no statistically significant relationship was found between SUVmax and survival for the majority of stages, T and N scores-except for Stage 1A and T1b, where significance was noted. This lack of statistical significance in the remaining subgroups may be attributed to the limited sample size, which reduces statistical power.
Discussion
The standardized uptake value (SUV) is a widely accepted functional metabolic biomarker derived from 18F-FDG PET imaging. Among SUV parameters, the maximum standardized uptake value (SUVmax) is the most frequently utilized in PET/CT assessments. Unlike immunohistochemical markers, SUVmax can provide prognostic information even in the absence of surgically obtained tissue samples. Numerous studies have demonstrated that the SUVmax of the primary tumor is a valuable prognostic factor in patients with lung cancer.6,7,8,9
FDG-PET/CT contributes significantly to clinical evaluation by detecting metabolically active tumoral lesions with high accuracy in various oncologic settings. It is widely used in the staging, recurrence detection, and prognostication of lung cancer. In particular, FDG-PET/CT has become a well-established standard of care in the pre-treatment staging of patients with non-small cell lung cancer (NSCLC) undergoing curative-intent therapy.10,11
In the present study, the prognostic significance of SUVmax was thoroughly investigated in a cohort of surgically treated NSCLC patients.
Several studies have demonstrated that an increase in SUVmax is associated with a poorer prognosis. In a study conducted by Dhijal K. et al.12, patients with an SUVmax of 20 or higher were found to have significantly worse prognoses. Similarly, in our study, patients with an SUVmax greater than 12.3 exhibited poorer outcomes.
The relationship between SUVmax and demographic factors such as age and gender remains controversial in the literature. A study by Merve H.I. et al.13, which included 732 lung cancer cases, reported a significant association between SUVmax and both gender and age. In contrast, Özlem O. et al.14 found no statistically significant relationship between SUVmax and age in a cohort of 171 patients with early-stage lung cancer. In our study, overall survival was found to be similar between male and female patients. This lack of difference may be due to the relatively small number of female patients in the cohort. In terms of age, survival was lower in both Group A and Group B patients with higher SUVmax values, suggesting that elevated SUVmax may be associated with worse prognosis regardless of age.
Several studies have demonstrated an association between SUVmax values and histopathological subtypes of lung cancer.15 Notably, a study by Liu et al.16 reported that patients with squamous cell carcinoma had significantly higher SUVmax values compared to those with adenocarcinoma (p < 0.001). In line with the existing literature, our study also identified a statistically significant correlation between SUVmax and histopathological subtypes of lung cancer.
Numerous studies have investigated the relationship between SUVmax and lung cancer staging, including T and N scores. In a study by Davide T. et al.17, 180 patients with pathologic stage I lung adenocarcinoma were retrospectively analyzed, and significant correlations were found between 18F-FDG PET/CT parameters (SUVmean, SUVmax, and TLG) and disease-free survival. Consistent with that study, our analysis also revealed a statistically significant association between SUVmax and survival in stage 1A patients.
In another study by Li et al., which included 107 NSCLC patients ranging from stage I to IV with T1 tumors, it was demonstrated that SUVmax values significantly increased with advancing stage. Additionally, the same study found that N0M0 patients had significantly lower SUVmax values compared to N1–3M0 patients.18
In our study, a statistically significant relationship between SUVmax and survival within the NSCLC staging system was observed only in early-stage disease (specifically stage 1A and T1b). This finding suggests that SUVmax may have a more prominent prognostic role in the early stages of the disease. The lack of significant associations in later stages may be attributed to the limited number of patients, which could reduce the statistical power of the analysis. A statistically significant association between SUVmax and overall survival was observed in Stage 1A and T1b subgroups (Table 2). Detailed survival analyses across all stage, T, and N subgroups are provided in Supplementary Table 1.
While several studies have supported the role of SUVmax as a prognostic factor in lung cancer,19 a meta-analysis conducted by Chinese researchers-encompassing 36 studies and 5,807 patients-reported several limitations regarding the clinical application of PET/CT parameters as prognostic markers. The authors noted that heterogeneity among patient populations, variability in cancer stages, retrospective cohort designs, inconsistency in PET/CT acquisition methods, and diverse calculation protocols limit the generalizability and standardization of SUVmax as a prognostic tool (mean SUVmax: 2.43).20
Despite the limitations of our study, including its retrospective design and relatively small sample size, our findings reinforce the notion that SUVmax holds value as a prognostic indicator in patients with non-small cell lung cancer.
In addition to these considerations, we found that SUVmax was significantly associated not only with overall survival but also with age, histological subtype, and the surgical approach used. We believe that SUVmax has the potential to become a clinically useful prognostic biomarker, particularly if validated through multicenter, large-scale, prospective studies.
Limitations
Our study has several limitations. The retrospective design, single-center nature, and relatively small sample size were identified as primary weaknesses. Additionally, variability in SUVmax calculation protocols across different centers may limit the generalizability of the findings.
Conclusion
We believe that incorporating SUVmax values into the routine clinical and preoperative evaluation of patients with non-small cell lung cancer (NSCLC) may aid in establishing appropriate diagnostic and therapeutic strategies. Furthermore, in patients for whom surgery is complex and carries high risk, SUVmax may help reduce the need for invasive diagnostic procedures. Overall, it may contribute meaningfully to prognostic assessment and individualized treatment planning.
Figures
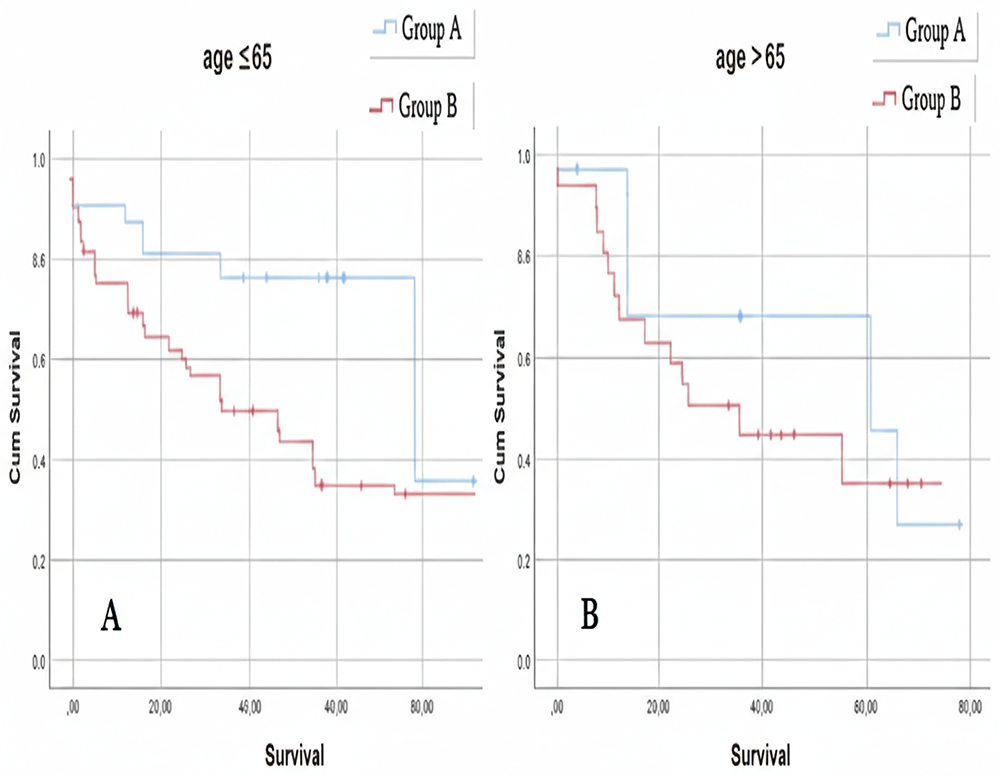
Figure 1. Survival curve by age and SUVmax
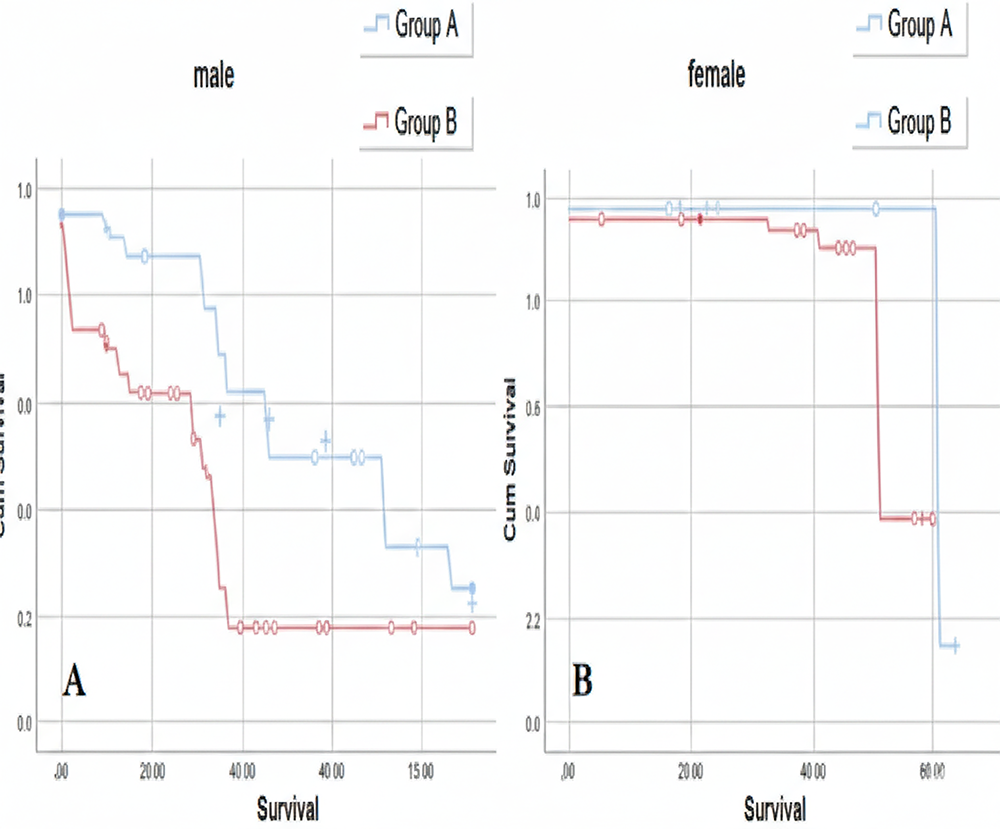
Figure 2. Survival curve by gender and SUVmax
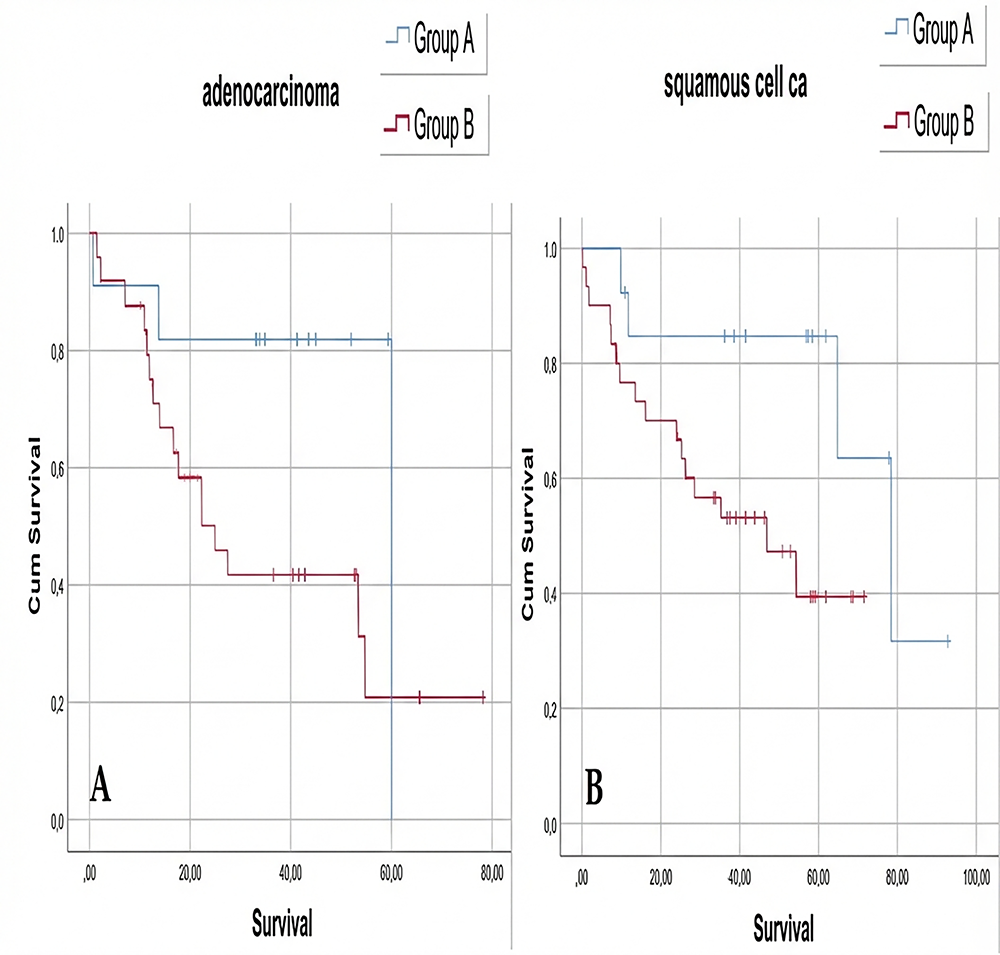
Figure 3. Survival curve by histopathological subtype and SUVmax
Tables
Table 1. Clinical characteristics of the patients (T: Tumor; N: Node; VATS: Video-assisted thoracoscopic surgery; n: Number)
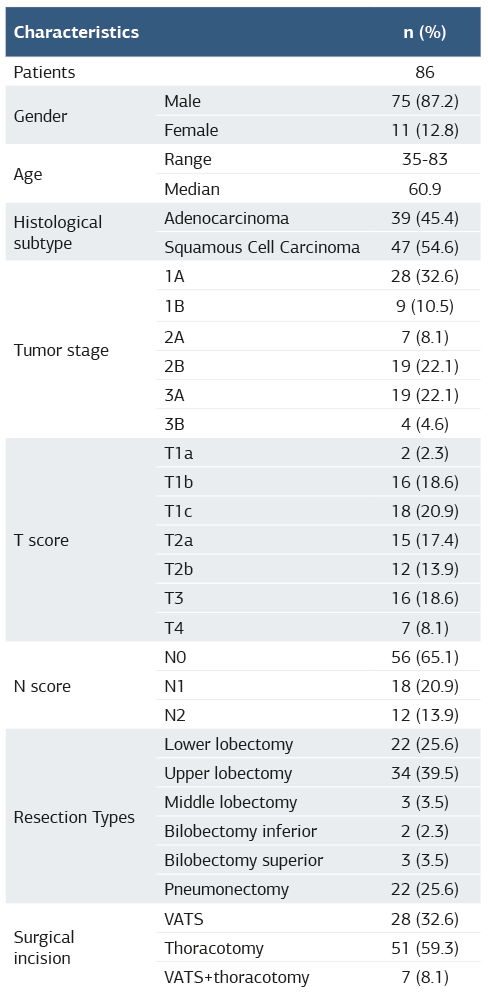
Table 2. Summary of significant subgroup survival analyses according to SUVmax groups (Stage 1A and T1b)
References
-
Huang J, Deng Y, Tin MS, et al. Distribution, risk factors, and temporal trends for lung cancer incidence and mortality: a global analysis. Chest. 2022;161(4):1101-1111.
-
Paz-Ares L, Dvorkin M, Chen Y, et al. Durvalumab plus platinum–etoposide versus platinum–etoposide in first-line treatment of extensive-stage small-cell lung cancer (CASPIAN): a randomised, controlled, open-label, phase 3 trial. Lancet. 2019;394(10212):1929-1939. doi:10.1016/S0140-6736(19)32222-6
-
Jiménez Londoño GA, García Vicente AM, Bosque JJ, et al. SUVmax to tumor perimeter distance: a robust radiomics prognostic biomarker in resectable non-small cell lung cancer patients. Eur Radiol. 2022;32(6):3889-3902.
-
Cheng G, Huang H. Prognostic value of 18F-fluorodeoxyglucose PET/computed tomography in non-small-cell lung cancer. PET Clin. 2018;13(1):59-72.
-
Huang YE, Pu YL, Huang YJ, et al. The utility of the nonattenuation corrected 18F-FDG PET images in the characterization of solitary pulmonary lesions. Nucl Med Commun. 2010;31(11):945-951.
-
Kohutek ZA, Wu AJ, Zhang Z, et al. FDG-PET maximum standardized uptake value is prognostic for recurrence and survival after stereotactic body radiotherapy for non-small cell lung cancer. Lung Cancer. 2015;89(2):115-120.
-
Nakamura H, Saji H, Marushima H, et al. Standardized uptake values in the primary lesions of non-small-cell lung cancer in FDG-PET/CT can predict regional lymph node metastases. Ann Surg Oncol. 2015;22(3):1388-1393.
-
Davies A, Tan C, Paschalides C, et al. FDG-PET maximum standardised uptake value is associated with variation in survival: analysis of 498 lung cancer patients. Lung Cancer. 2007;55(1):75-78.
-
Jin F, Zhu H, Fu Z, et al. Prognostic value of the standardized uptake value maximum change calculated by dual-time-point 18F-fluorodeoxyglucose positron emission tomography imaging in patients with advanced non-small-cell lung cancer. Onco Targets Ther. 2016;9:2993-3001.
-
Kuipers H, Hoogwater FJH, Holtman GA, et al. Diagnostic performance of preoperative CT in differentiating between benign and malignant origin of suspicious gallbladder lesions. Eur J Radiol. 2021;138:109619. doi:10.1016/j.ejrad.2021.109619
-
Ma J, He N, Yoon JH, et al. Distinguishing benign and malignant lesions on contrast-enhanced breast cone-beam CT with deep learning neural architecture search. Eur J Radiol. 2021;142:109878. doi:10.1016/j.ejrad.2021.109878
-
Dhital K, Saunders CA, Seed PT, et al. 18F-fluorodeoxyglucose positron emission tomography and its prognostic value in lung cancer. Eur J Cardiothorac Surg. 2000;18(4):425-428.
-
Idge HM, Ozturk A, Oruc O, et al. The relationship of PET/CT SUVmax with EGFR mutation status and ALK rearrangement in lung adenocarcinoma. Hell J Nucl Med. 2022;25(2):188-195.
-
Okumus O, Mardanzai K, Plönes T, et al. Preoperative PET-SUVmax and volume-based PET parameters of the primary tumor fail to predict nodal upstaging in early-stage lung cancer. Lung Cancer. 2023;176:82-88.
-
Divisi D, Rinaldi M, Necozione S, et al. Is it possible to establish a reliable correlation between maximum standardized uptake value of 18-fluorine fluorodeoxyglucose positron emission tomography/computed tomography and histological types of non-small cell lung cancer? Diagnostics (Basel). 2021;11(10):1901. doi:10.3390/diagnostics11101901
-
Liu X, Zou Q, Sun Y, et al. Role of multiple dual-phase 18F-FDG PET/CT metabolic parameters in differentiating adenocarcinomas from squamous cell carcinomas of the lung. Heliyon. 2023;9(10):e20180. doi:10.1016/j.heliyon.2023.e20180
-
Tosi D, Pieropan S, Cattoni M, et al. Prognostic value of 18F-FDG PET/CT metabolic parameters in surgically treated stage I lung adenocarcinoma patients. Clin Nucl Med. 2021;46(8):621-626.
-
Li M, Liu N, Hu M, et al. Relationship between primary tumor fluorodeoxyglucose uptake and nodal or distant metastases at presentation in T1 stage non-small cell lung cancer. Lung Cancer. 2009;63(3):383-386.
-
Vansteenkiste J, Fischer BM, Dooms C, Mortensen J. Positron-emission tomography in prognostic and therapeutic assessment of lung cancer: systematic review. Lancet Oncol. 2004;5(1):531-540.
-
Liu J, Dong M, Sun X, et al. Prognostic value of 18F-FDG PET/CT in surgical non-small cell lung cancer: a meta-analysis. PLoS One. 2016;11(1):e0146195. doi:10.1371/journal.pone.0146195
Declarations
Scientific Responsibility Statement
The authors declare that they are responsible for the article’s scientific content, including study design, data collection, analysis and interpretation, writing, and some of the main line, or all of the preparation and scientific review of the contents, and approval of the final version of the article.
Animal and Human Rights Statement
All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Funding
None
Conflict of Interest
The authors declare that there is no conflict of interest.
Ethics Declarations
This study was approved by the Ethics Committee of the Inonu University Scientific Research and Publication Ethics Board (Date: 2020-09-29, No: 2020/940).
Informed Consent
Written informed consent was obtained from all participants prior to enrollment.
Data Availability
The data supporting the findings of this article are available from the corresponding author upon reasonable request, due to privacy and ethical restrictions. The corresponding author has committed to share the de-identified data with qualified researchers after confirmation of the necessary ethical or institutional approvals. Requests for data access should be directed to bmp.eqco@gmail.com
Author Contributions
Conceptualization: M.A.
Methodology: M.A., I.G.
Formal Analysis: M.K.
Investigation: M.A., H.U.
Data Curation: M.K.
Writing – Original Draft: M.A.
Writing – Review & Editing: I.G., M.R.C.
Supervision: M.R.C.
Abbreviations
AUC: Area under the curve
CI: Confidence interval
CT: Computed tomography
FDG: Fluorodeoxyglucose
IASLC: International Association for the Study of Lung Cancer
NSCLC: Non-small cell lung cancer
PET: Positron emission tomography
ROC: Receiver operating characteristic
SUV: Standardized uptake value
SUVmax: Maximum standardized uptake value
TLG: Total lesion glycolysis
TNM: Tumor, Node, Metastasis
VATS: Video-assisted thoracoscopic surgery
Additional Information
Publisher’s Note
Bayrakol MP remains neutral with regard to jurisdictional and institutional claims.
Rights and Permissions
About This Article
How to Cite This Article
Mehmet Agar, Ilham Gulcek, Muhammed Kalkan, Hakki Ulutas, Muhammet Reha Çelik. The prognostic impact of 18F-FDG PET SUVmax in patients with non-small cell lung cancer. Ann Clin Anal Med 2026;17(Suppl 1):S44-49
Publication History
- Received:
- April 15, 2025
- Accepted:
- May 19, 2025
- Published Online:
- July 8, 2025
- Printed:
- February 20, 2026

