A rare bilateral anatomical variant of the patellartendon with patellofemoral maltracking: A Case Report
Bilateral cross-double patellar tendon
Authors
Abstract
Introduction The cross-double patellar tendon, a rare anatomical variant, is characterized by two distinct tendinous structures that cross between the patella and the tibial tuberosity. This unique feature, observed in the first reported case of bilateral cross-double patellar tendon, is a significant and intriguing discovery. Recognizing this variant is crucial to avoid misdiagnosis as traumatic or postoperative pathology and to understand its potential role in patellofemoral dysfunction.
Case Presentation The 28-year-old man presented with chronic anterior knee pain and a history of childhood patellar instability. MRI of both knees revealed bilateral crossing tendinous bundles with intervening fat planes on T1-weighted sequences, distinguishing this congenital variant from acquired conditions. The potential impact of this variant on the extensor mechanism, patellar maltracking, and progressive cartilage degeneration is a cause for concern.
Conclusion The bilateral cross-double patellar tendon is a rare developmental anatomical variant with distinctive imaging features. Radiologists and orthopedic surgeons must be aware of this entity, as accurate diagnosis is key to preventing misinterpretation as pathology. This responsibility highlights the need for further urgent studies to determine its prevalence, biomechanical implications, and long-term outcomes.
Keywords
Introduction
The extensor mechanism of the knee comprises the quadriceps muscle group, the patella, and the patellar tendon, working in a coordinated fashion to enable knee extension and weight-bearing activities. The patellar tendon, traditionally described as a single, uniform structure connecting the inferior pole of the patella to the tibial tuberosity, serves as the final link in force transmission from the quadriceps muscles to the tibia. Understanding normal patellar tendon anatomy and recognizing anatomical variants is essential for accurate diagnosis and appropriate management of patellofemoral disorders.
Anatomical variations of the patellar tendon are infrequent, with the medical literature containing only scattered case reports documenting such anomalies. The most recently described variant is the double uncrossed patellar tendon, reported by Basha et al. in 2025.1 This landmark study emphasized the critical importance of recognizing anatomical variants to prevent misdiagnosis and unnecessary interventions, as these variants can mimic extensor mechanism tears, tendon delamination, or postoperative changes on imaging studies. This case report further underscores the clinical significance of recognizing such variants in the evaluation of chronic patellofemoral dysfunction.
The clinical significance of patellar tendon anatomical variants extends beyond their rarity as anatomical curiosities. Recent advances in understanding tendon biomechanics have demonstrated that even subtle alterations in tendon morphology can significantly impact functional properties and predispose to pathological changes.2 The present case report describes a previously undocumented anatomical variant: bilateral cross-double patellar tendon, where two distinct tendinous structures cross each other in their course from the patella to the tibial tuberosity. This variant differs fundamentally from the uncrossed double patellar tendon described by Basha et al.1 as the crossing pattern creates a unique anatomical configuration with potentially different biomechanical implications. The case is presented to expand our understanding of anatomical variations in the extensor mechanism and to highlight the clinical relevance of recognizing such variants in the evaluation of chronic patellofemoral dysfunction.
Case Presentation
A 28-year-old male patient presented with a three-year history of progressive left anterior knee pain, which had significantly worsened over the preceding months. The patient’s description of the pain as a deep, aching sensation localized to the anterior aspect of the knee, accompanied by mechanical symptoms and functional limitations during activities of daily living, underscores the impact of patellofemoral pain syndrome on his quality of life.
The patient’s medical history was significant for habitual patellar dislocation during childhood, which had required bilateral surgical stabilization procedures. This history of patellar instability and the subsequent surgical interventions provide important context for the current presentation of chronic anterior knee pain.
Physical examination revealed bilateral surgical scars consistent with previous patellar stabilization procedures. Palpation demonstrated tenderness along the medial and lateral joint lines of both knees, with particular sensitivity over the patellar facets and surrounding soft tissues. The patellar compression test was positive bilaterally, eliciting pain and apprehension during patellofemoral compression. Notably, patellar mobility assessment revealed medial patellar subluxation of the right knee, with abnormal patellar tracking during passive range of motion testing.
Range of motion evaluation demonstrated full extension bilaterally, with flexion limited to 130 degrees on the left and 135 degrees on the right due to pain and mechanical restrictions. Ligamentous stability testing revealed no evidence of cruciate or collateral ligament laxity, and meniscal provocation tests were negative bilaterally.
Magnetic Resonance Imaging (MRI) of both knees was performed using a 1.5 Tesla scanner with comprehensive protocols, including sagittal T1-weighted sequences, proton density-weighted (PD) sequences, and transverse PD sequences with and without fat suppression. The imaging revealed the remarkable finding of bilateral cross-double patellar tendons, representing a previously undescribed anatomical variant.
The left knee demonstrated a cross-double patellar tendon configuration with two distinct tendinous structures originating from the inferior pole of the patella and crossing each other in the mid-portion of their course before inserting onto the tibial tuberosity (Figure 1A, 1B).
The superficial bundle appeared to maintain continuity with the pre-patellar quadriceps tendon, while the deep bundle demonstrated a more direct insertion pattern. Crucially, T1-weighted images revealed a bright signal between the superficial and deep bundles, consistent with intervening fat tissue originating from Hoffa’s fat pad, which served as a key diagnostic feature distinguishing this anatomical variant from pathological conditions.
Additional findings in the left knee included grade I-II meniscal degeneration affecting both medial and lateral menisci, mild chondromalacia of the femoral medial condyle, and full-thickness cartilage loss at the patellar apex with associated subchondral bone changes. Moderate joint effusion with synovial thickening was present, along with Hoffa’s fat pad edema and prepatellar soft tissue inflammation. A large Baker’s cyst and subgastrocnemius bursitis were also identified, along with mild gonarthrosis and mucoid degeneration of the anterior cruciate ligament.
The right knee demonstrated an identical cross-double patellar tendon morphology, confirming the bilateral nature of this anatomical variant (Figure 2A, 2B).
The crossing pattern, signal characteristics, and intervening fat planes were virtually identical to those observed in the left knee, strongly supporting a congenital rather than acquired etiology. Associated findings included similar meniscal degenerative changes, full-thickness chondral thinning at the patellar apex, joint effusion with synovial proliferation, and Hoffa’s fat pad edema comparable to the contralateral knee.
Ethics Approval
Ethics committee approval was obtained from the Ethics Committee of Istanbul Aydın University (Date: 2025-05-20, No: 2552), and written informed consent was obtained from the patient for publication of this case report and accompanying images.
Reporting Guidelines
This case is reported in accordance with the CARE guidelines.
Discussion
This case represents the first documented bilateral cross-double patellar tendon variant in the medical literature, significantly expanding our understanding of anatomical variations in the extensor mechanism of the knee. The unique crossing pattern of the tendinous structures distinguishes this variant from the recently described double uncrossed patellar tendon reported by Basha et al., where parallel tendinous structures extend without crossing.1 The bilateral symmetric presentation, characteristic imaging features, and absence of trauma history strongly support a developmental etiology for this rare anatomical variant.
The diagnostic imaging features of a cross-double patellar tendon are distinctive and crucial for accurate recognition. The key finding is the presence of two distinct tendinous structures crossing each other, clearly visualized on sagittal and axial MRI sequences. The bright T1 signal between the superficial and deep bundles, representing intervening fat tissue from Hoffa’s fat pad, serves as a pathognomonic feature distinguishing this anatomical variant from acquired pathology.3 This finding is consistent with the observations of Basha et al. regarding the importance of intervening fat planes in diagnosing patellar tendon anatomical variants.1
The differential diagnosis of patellar tendon abnormalities on MRI includes several important considerations that must be carefully evaluated. Traumatic patellar tendon rupture typically presents with discontinuity of tendinous fibers, retraction of tendon ends, and surrounding hemorrhage or edema, features that were absent in our case.4 Patellar tendinopathy is characterized by tendon thickening, increased T2 signal intensity, and degenerative changes; however, it does not produce the crossing pattern observed in our patient.4,5 Tendon delamination, where the tendon splits into separate layers, typically occurs in the setting of trauma or chronic overuse and lacks the symmetric bilateral presentation and intervening fat planes characteristic of anatomical variants.6
The biomechanical implications of the crossing tendon configuration are complex and potentially significant. Normal patellar tendon function relies on uniform force transmission from the quadriceps muscles to the tibia through a single, cohesive tendinous structure.7 The presence of crossing tendinous bundles may create areas of stress concentration at the intersection points, potentially predisposing to localized degeneration or inflammatory changes over time. Additionally, the altered force transmission patterns may contribute to abnormal patellar kinematics, as evidenced by the medial patellar subluxation observed in our patient.
The clinical significance of the cross-double patellar tendon extends beyond its rarity as an anatomical finding. The association with chronic anterior knee pain, patellofemoral cartilage degeneration, and patellar instability in our patient suggests important functional implications. The altered biomechanics resulting from the abnormal tendon configuration may contribute to increased patellofemoral contact pressures, particularly in specific regions of the patellofemoral joint, accelerating cartilage degeneration and contributing to pain symptoms.8
Recent research on patellofemoral joint biomechanics has demonstrated the critical importance of maintaining normal anatomical relationships in order to preserve joint function.6 The cross-double patellar tendon variant may represent an additional risk factor for patellofemoral dysfunction that has not been previously recognized. Traditional risk factors for patellar instability include trochlear dysplasia, increased Q-angle, patella alta, and soft tissue abnormalities. The cross-double patellar tendon variant may represent an additional anatomical risk factor that should be considered in the evaluation of patients with recurrent patellar instability.
The management implications of patellar tendon anatomical variants remain largely unexplored due to their rarity. Conservative management strategies, including physical therapy focused on quadriceps strengthening and patellar tracking optimization, represent the first-line approach for most patients with patellofemoral dysfunction.6 However, the optimal treatment approach for patients with anatomical variants may require modification of standard protocols to account for altered biomechanical relationships.
Recognition of the cross-double patellar tendon as a distinct anatomical variant has important implications for clinical practice. Radiologists must be aware of this variant to avoid misinterpreting it as a pathological condition. Orthopedic surgeons should also consider the presence of anatomical variants when evaluating and managing patients with chronic patellofemoral dysfunction. The bilateral symmetric presentation and characteristic imaging features serve as key diagnostic criteria for distinguishing this variant from acquired pathology.
This case highlights several important limitations in our current understanding of patellar tendon anatomical variants. The relationship between the anatomical variant and the patient’s symptoms, while strongly suggested by the clinical and imaging findings, cannot be definitively established without additional evidence from larger studies. The natural history of cross-double patellar tendons and their long-term functional implications remains unknown, representing important areas for future research.
Limitations
Long-term follow-up data are not available to assess the natural history and progression of symptoms in patients with this anatomical variant.
Conclusion
We report the first documented case of bilateral cross-double patellar tendon, a rare anatomical variant characterized by two distinct tendinous structures crossing between the patella and tibial tuberosity. This variant differs from the previously described double uncrossed patellar tendon and may contribute to patellofemoral dysfunction through altered biomechanics. Recognition of this variant is crucial for radiologists and orthopedic surgeons to ensure accurate diagnosis and avoid misinterpretation as pathological conditions. The bilateral symmetric presentation and characteristic imaging features, particularly the intervening fat planes in T1-weighted MRI sequences, serve as key diagnostic criteria. Further research is needed to understand the prevalence, natural history, and optimal management of this anatomical variant.
Figures
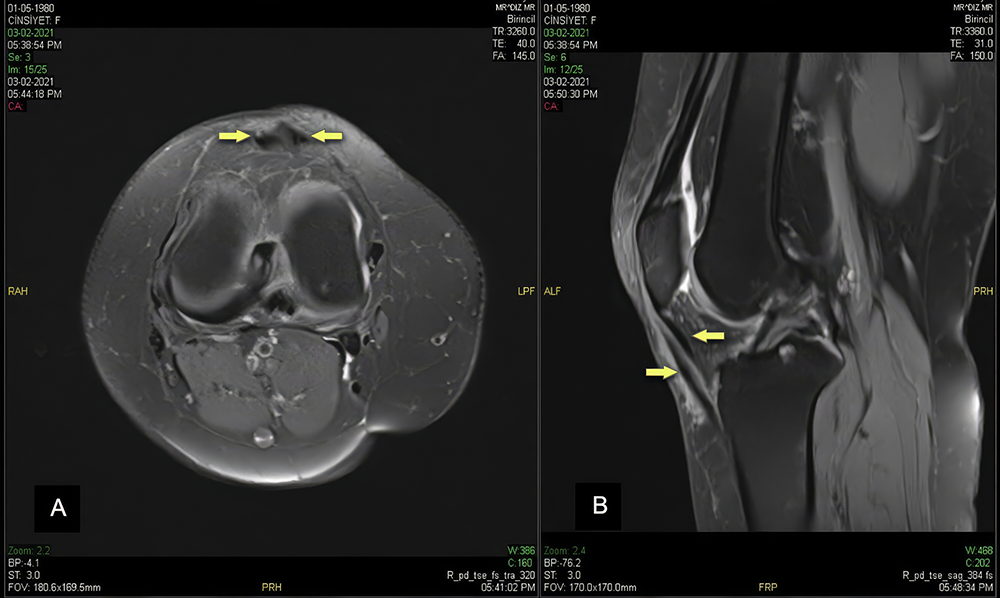
Figure 1. Axial (A) and sagittal (B) PD images of the left knee demonstrate cross-double patellar tendons
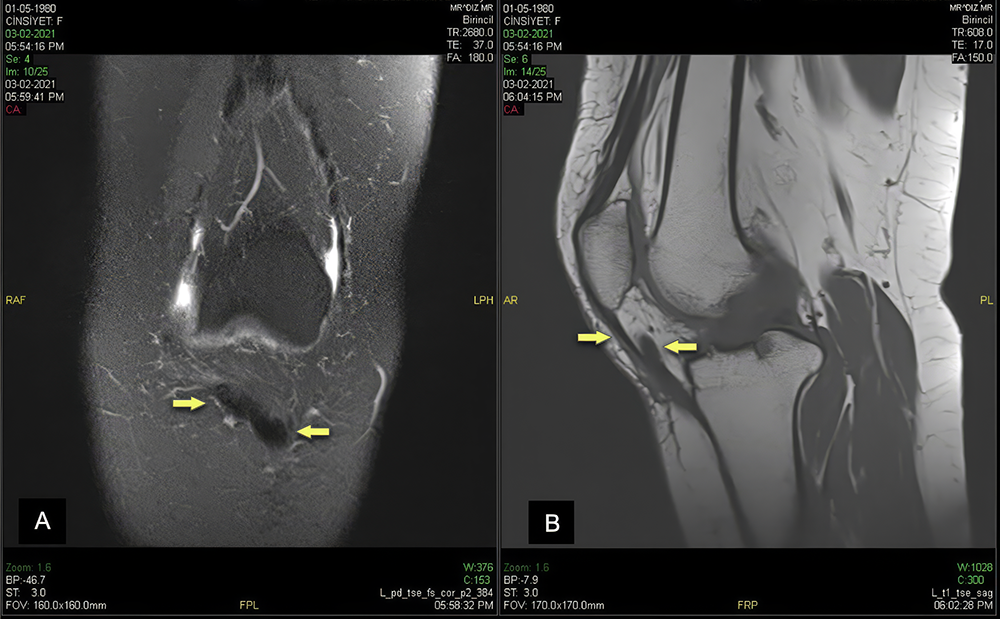
Figure 2. Coronal PD (A) and sagittal T1-weighted (B) images of the right knee demonstrate cross-double patellar tendons
References
-
Basha A, Shaikh A, Silva FD, Chaganti SR, Chhabra A. Double uncrossed patellar tendon: a rare knee variant case series. Egypt J Radiol Nucl Med. 2025;56:27. doi:10.1186/s43055-025-01441-0
-
Sims DT, Onambélé-Pearson GL, Burden A, Payton C, Morse CI. Morphological and mechanical properties of the human patella tendon in adult males with achondroplasia. Front Physiol. 2018;9:867. doi:10.3389/fphys.2018.00867
-
Haydar SMA, Miles J, Hargunani R. The uncrossed-doubled patellar tendon: a novel imaging finding. Radiol Case Rep. 2019;14(12):1509-12. doi:10.1016/j.radcr.2019.09.029
-
Cook JL, Rio E, Purdam CR, Docking SI. Revisiting the continuum model of tendon pathology: what is its merit in clinical practice and research?. Br J Sports Med. 2016;50(19):1187-91. doi:10.1136/bjsports-2015-095422
-
Masroori Z, Haseli S, Abbaspour E, et al. Patellar non-traumatic pathologies: a pictorial review of radiologic findings. Diagnostics (Basel). 2024;14(24):2828. doi:10.3390/diagnostics14242828
-
Powers CM, Witvrouw E, Davis IS, Crossley KM. Evidence-based framework for a pathomechanical model of patellofemoral pain: 2017 patellofemoral pain consensus statement from the 4th International Patellofemoral Pain Research Retreat, Manchester, UK: part 3. Br J Sports Med. 2017;51(24):1713-23. doi:10.1136/bjsports-2017-098717
-
Brinkman JC, Reeson E, Chhabra A. Acute patellar tendon ruptures: an update on management. J Am Acad Orthop Surg Glob Res Rev. 2024;8(4):e2400060. doi:10.5435/JAAOSGlobal-D-24-00060
-
Garcia S, Delattre N, Berton E, Rao G. Patellar tendon force differs depending on jump-landing tasks and estimation methods. Appl Sci. 2022;12(1):488. doi:10.3390/app12010488
Declarations
Scientific Responsibility Statement
The authors declare that they are responsible for the article’s scientific content, including study design, data collection, analysis and interpretation, writing, and some of the main line, or all of the preparation and scientific review of the contents, and approval of the final version of the article.
Animal and Human Rights Statement
All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Funding
None.
Conflict of Interest
The authors declare that there is no conflict of interest.
Ethics Declarations
Ethics committee approval was obtained from the Ethics Committee of Istanbul Aydın University (Date: 2025-05-20, No: 2552).
Informed Consent
Ethics committee approval was obtained from the Ethics Committee of Istanbul Aydın University (Date: 2025-05-20, No: 2552), and written informed consent was obtained from the patient for publication of this case report and accompanying images.
Data Availability
The datasets used and/or analyzed during the current study are not publicly available due to patient privacy reasons but are available from the corresponding author on reasonable request.
Author Contributions
Conceptualization: A.U., O.G.
Methodology: A.U., O.G.
Formal Analysis: A.U.
Investigation: A.U., O.G., M.Y.K.
Data Curation: A.U.
Resources: O.G., M.Y.K.
Writing – Original Draft Preparation: A.U.
Writing – Review & Editing: O.G., M.Y.K.
Visualization: A.U.
Abbreviations
BMI: Body Mass Index
C/S: Cesarean Section
FGR: Fetal Growth Restriction
GDM: Gestational Diabetes Mellitus
NICU: Neonatal Intensive Care Unit
SD: Standard Deviation
S/D: Systole/Diastole Ratio
UA: Umbilical Artery
UCI: Umbilical Cord Coiling Index
VB: Vaginal Birth
Additional Information
Publisher’s Note
Bayrakol MP remains neutral with regard to jurisdictional and institutional claims.
Rights and Permissions
About This Article
How to Cite This Article
Ali Uludag, Ozgur Genc, Mehmet Yadigar Kırıcı. A rare bilateral anatomical variant of the patellar tendon with patellofemoral maltracking: A Case Report. Ann Clin Anal Med 2026;17(Suppl 1):S77-80
Publication History
- Received:
- August 3, 2025
- Accepted:
- September 29, 2025
- Published Online:
- October 16, 2025
- Printed:
- February 20, 2026

