Efficacy of device-based inspiratory muscle training as an adjunct therapy in ankylosing spondylitis patients: a randomized controlled trial
IMT as adjunct therapy in AS; RCT
Authors
Abstract
Aim To evaluate the effectiveness of device-based inspiratory muscle training (IMT) compared with conventional exercises (CE) on pulmonary function, disease activity, functional status, mood, and quality of life in patients with ankylosing spondylitis (AS).
Methods This randomized controlled trial included 40 patients with AS who were allocated to receive standard physical therapy supplemented by either CE (n = 20) or IMT using the Respifit-S® device (n = 20). The interventions were performed for 30 minutes daily over 20 days. Outcomes, assessed pre- and post-intervention, included pulmonary function tests (PFTs), chest expansion, the Bath Ankylosing Spondylitis Disease Activity (BASDAI) and Functional (BASFI) Indices, a Visual Analog Scale (VAS) for pain, the Beck Depression Inventory (BDI), and the SF-36 questionnaire.
Results Baseline characteristics were comparable between the groups. Both groups showed significant post-intervention improvements in VAS pain, BASDAI, BASFI, chest expansion, BDI, Peak Expiratory Flow (PEF), and the SF-36 domains of General Health, Pain, and Physical Function (all p < 0.05). Compared to the CE group, the IMT group showed significantly greater improvements in chest expansion (p < 0.001), BDI scores (p = 0.012), and the SF-36 domains of Vitality (p = 0.049) and Physical Function (p = 0.008). No significant between-group differences were observed for changes in the VAS, BASDAI, BASFI, PEF, or other SF-36 domains. No adverse events occurred.
Conclusion While both conventional exercises and IMT improve clinical outcomes in AS, incorporating device-based IMT provides superior benefits in enhancing chest expansion, alleviating depressive symptoms, and improving specific quality of life domains. IMT represents a valuable adjunctive therapy in the comprehensive management of ankylosing spondylitis.
Keywords
Introduction
Ankylosing spondylitis (AS) is a chronic, inflammatory rheumatic disease 1,2. This condition primarily targets the axial skeleton and affects the spine and sacroiliac joints 1. Peripheral joints may also become involved during the disease course 2. Chronic inflammation associated with AS can lead to ossification and progressive fusion of the spinal and thoracic joints 3. This pathogenic process restricts mobility. Consequently, pulmonary dysfunction can develop over time 3.
The disease often results in thoracic hyperkyphosis and limited motion of the thoracic cage 2,4. These structural changes decrease chest wall compliance. Reduced chest wall compliance negatively affects the lung mechanics. Patients with AS frequently exhibit restrictive pulmonary patterns. These patients may experience diminished vital capacity 5. Restrictive pulmonary function is more common in individuals with AS than in matched control populations 5.
This restrictive pulmonary pattern in AS is often compounded by respiratory muscle weakness, which compromises both inspiratory and expiratory strength and can further limit exercise capacity 4,5. As exercise is a cornerstone of AS management, targeted interventions like Inspiratory Muscle Training (IMT) have emerged as a promising approach 6. IMT is a technique designed to improve the strength and endurance of inspiratory muscles, with demonstrated efficacy in other chronic conditions such as chronic obstructive pulmonary disease and heart failure 7. This training method has demonstrated efficacy in boosting the respiratory muscle strength in other patient groups. IMT has shown benefits in chronic conditions such as chronic obstructive pulmonary disease and heart failure. It can improve maximum inspiratory pressure and diaphragmatic function 7. Biologically, strengthening these muscles may not only improve direct measures like maximum inspiratory pressure but could also enhance overall thoracic mobility and chest wall expansion against the progressive stiffness of the disease. The use of specialized devices for IMT offers distinct advantages by standardizing the training load, permitting objective progress monitoring, and supporting patient adherence to the therapeutic regimen 7,8.
Despite these recognized respiratory impairments and the clear rationale for IMT, research evaluating its specific efficacy in the AS population remains notably limited, with a scarcity of high- quality studies assessing its precise effects 5,7. Therefore, we aimed to evaluate the effectiveness of device-based IMT on pulmonary function, disease activity, functional status, and quality of life in patients with ankylosing spondylitis 5,7,9.,
Materials and Methods
Study Design
This investigation was designed as a randomized, controlled, prospective clinical study.
Participants
Forty patients aged 18-70 years diagnosed with AS according to the modified New York criteria were recruited. Recruitment occurred between October 2012 and June 2013 at the Necmettin Erbakan University, Meram Faculty of Medicine Physical Medicine and Rehabilitation Outpatient Clinic.
Inclusion Criteria
Patients who fulfilled the modified New York criteria for AS aged 18-70 years were included.
Exclusion Criteria
Individuals with malignancy, pregnancy, severe systemic illness, recent surgical operations, or cooperation disorders were excluded.
Participants underwent comprehensive history-taking and physical examinations before study entry. Examinations assessed neck, back, lumbar, shoulder, elbow, hand, finger, hip, knee, ankle, and foot joint range of motion. Chest expansion measurements were also recorded. Neurological assessment included motor and sensory evaluations, deep tendon reflexes, and pathological reflexes. Demographic data, such as age, sex, height, weight, comorbidities, smoking status, medication use, and symptom duration, were documented.
Randomization and Interventions
Eligible patients were randomly assigned to two equal groups (Conventional Exercise or Inspiratory Muscle Training; n = 20 each) using a simple coin-toss method. Randomization was performed by an independent individual not involved in enrollment, with allocations placed in sequentially numbered, sealed opaque envelopes to maintain allocation concealment. To ensure comparability, both groups received an identical standard physical therapy regimen in addition to their assigned intervention. Both groups received standard physical therapy daily sessions for 20 days, including 30 minutes of hot packs to the dorsal-lumbar region, 6 minutes of ultrasound (2 W/ cm2) to the thoracic and lumbar areas, and 30 minutes of TENS to paravertebral muscles. Additionally, hydrotherapy was administered five times per week over two weeks. Each intervention group also underwent supervised 30-minute daily sessions for 20 consecutive days, following their respective protocols.
Group 1 (Conventional Exercise [CE] Group)
Sessions consisted of conventional respiratory exercises, including pectoral stretching, back extensor strengthening, abdominal breathing, pursed-lip breathing, and deep inspiration techniques.
Group 2 (IMT Group)
Sessions involved inspiratory muscle training using the Respifit-S® device (Biegler GmbH, Mauerbach, Austria), a portable inspiratory muscle training tool that enhances respiratory muscle strength and endurance through adjustable resistance. Its handheld module offers selectable aperture settings (A, B, C) to modulate inspiratory resistance, enabling tailored training intensity. Patient-specific settings were stored on a data key, and resistance was progressively increased when patients performed exercises with ease, ensuring individualized strength and endurance protocols under physician supervision. Each 30-minute intervention session was supervised by a physician.
The Measurement of Outcomes
The assessor responsible for evaluating all outcome measures was blinded to the group assignments of the participants. Assessments were performed by the same physician before and after the treatment period. The following parameters were evaluated: Pain and Functional Assessment: Pain intensity was measured using a 10-cm Visual Analog Scale (VAS) for resting pain, where 0 indicated no pain and 10 indicated severe pain. Functional status was assessed using the Bath Ankylosing Spondylitis Functional Index (BASFI). This index comprises 10 questions regarding daily activities and coping ability over the preceding week, scored on a 10 cm VAS. The total score is the average of the 10 questions 10.
Disease Activity: The Bath Ankylosing Spondylitis Disease Activity Index (BASDAI) was used to evaluate disease activity over the last week. It consists of 6 questions covering 5 major symptoms: fatigue, spinal pain, joint pain/swelling, localized tenderness, and morning stiffness (duration and severity). Responses used a 10 cm horizontal VAS. The final BASDAI score is scaled from 0-10. Its validity and reliability have also been established 11.
Pulmonary Function Tests (PFTs): PFTs were conducted using a Sensorimedics VMax22™ spirometer to quantitatively assess respiratory function. Measurements included Forced Vital Capacity (FVC), Forced Expiratory Volume in 1 s (FEV1), Peak Expiratory Flow (PEF), and Forced Expiratory Flow between 25-75% of FVC (FEF25-75). The optimal values from repeated maneuvers were recorded.
Chest Expansion: Measured circumferentially using a tape measure at the level of the nipples (4th rib) in males or just below the breasts in females. To minimize inter-rater variability, all chest expansion measurements for all participants at both baseline and follow-up were performed by the same single assessor. The difference between maximum inspiration and maximum expiration was recorded after at least two attempts, noting the largest value.
Mood: The Beck Depression Inventory (BDI), a 21-item scale measuring somatic, emotional, and cognitive symptoms of depression, was used. A score of 17 or higher indicates depression. The Turkish validity and reliability study was performed by Hisli 12.
Quality of Life: Assessed using the Short Form 36 (SF- 36) questionnaire. The 36-item tool measures eight health dimensions: physical functioning, role limitations due to physical problems, bodily pain, general health perception, vitality, social functioning, role limitations due to emotional problems, and mental health. Scores range from 0 (poor health) to 100 (good health) for each subscale; there is no total score. Its Turkish translation and validation have been documented 13.
Statistical Analysis
A sample size of 20 patients per group was determined to provide approximately 70% power to detect a large effect size (Cohen’s d = 0.8) between the groups for the primary outcome measures, using a two-sided independent samples t-test with a significance level (α) of 0.05. The assumption of a large effect size was deemed appropriate for several reasons. At the time of the study design, while specific data on IMT in AS were scarce, this estimate was informed by studies in other chronic conditions with respiratory compromise where targeted training demonstrated substantial improvements. Furthermore, it was hypothesized that a device-based, resistance-loaded intervention like IMT would yield a clinically meaningful and large effect on key respiratory parameters (such as chest expansion) compared to conventional, non-resisted exercises. Data analysis utilized SPSS version 16.0 (SPSS Inc., Released 2008. SPSS Statistics for Windows, Version 16.0. Chicago: SPSS Inc). Continuous data were presented as mean ± standard deviation, while frequency data were shown as percentages. The Kolmogorov-Smirnov test assessed the normality of the data distribution. For comparing continuous variables between groups, the Independent-samples t-test (for normal distribution) or the Mann-Whitney U test (for non- normal distribution) was employed. Categorical variables were compared using the Chi-square test or Fisher’s Exact test when expected frequencies were below 5. Within-group comparisons (pre- vs. post-treatment) utilized the Paired samples t-test (normal distribution) or Wilcoxon Signed-Rank test (non-normal distribution) for continuous variables, and the McNemar test for categorical variables. Spearman Correlation Analysis examined the relationships between the variables. A p-value less than 0.05 was considered statistically significant.
Informed Consent
All participants provided informed consent before enrollment in the trial.
Ethical Approval
This study was approved by the Ethics Committee of Necmettin Erbakan University, Meram Faculty of Medicine, Konya, Türkiye (Date: 2012-10-5, No: 2012/243). All participants provided informed consent before enrollment in the trial.
Results
Participant Characteristics
Forty patients diagnosed with AS completed the study protocol. Participants were randomly assigned to either the CE group (n = 20) or the IMT group (n = 20). No adverse events related to the interventions occurred; consequently, no patient withdrew due to side effects. The participant flow through the study is presented in Figure 2.
The baseline demographic and clinical features were comparable between the two cohorts. The mean age, Body Mass Index (BMI), smoking duration, symptom onset age, diagnosis age, diagnostic delay, and disease duration showed no significant intergroup differences (all p > 0.05), as detailed in Table 1. Both groups were predominantly male (CE: 65%, n = 13; IMT: 80%, n = 16), with a similar distribution of smoking status, comorbidities, and medication usage patterns. Furthermore, baseline values for key clinical measures -including VAS for pain, BASDAI, BASFI, chest expansion, and BDI scores- revealed no statistically significant variations. Likewise, the baseline scores across all eight domains of the Short Form 36 (SF-36) quality of life questionnaire and all pulmonary function test parameters did not differ significantly between the groups (all p > 0.05).
Within-Group Changes (Pre vs. Post Treatment)
Following the 20-day intervention period, both groups demonstrated statistically significant improvements in several clinical measures. As shown in Table 2, both groups experienced significant reductions in pain, disease activity (BASDAI), functional limitation (BASFI), and depressive symptoms (BDI), alongside significant increases in chest expansion.
Both groups also showed significant improvements in certain SF-36 domains. The CE group improved significantly in General Health Perception (p < 0.001), Pain (p = 0.003), and Physical Function (p = 0.030). The IMT group showed significant gains in General Health Perception (p < 0.001), Pain (p < 0.001), Vitality (p = 0.005), Physical Function (p < 0.001), and Emotional Role Limitation (p = 0.021).
Regarding pulmonary function, only Peak Expiratory Flow (PEF) showed a statistically significant improvement within both groups (CE: p = 0.022; IMT: p = 0.023). Other pulmonary function parameters did not change significantly within either group.
Between-Group Comparisons (Change Scores)
A comparison of the change scores (post-treatment minus pre- treatment) revealed that the improvements in VAS pain, BASDAI, BASFI, and PEF were not significantly different between the groups (all p > 0.05). Similarly, there were no significant between-group differences for most SF-36 subscales.
However, the IMT group exhibited significantly greater improvements than the CE group in chest expansion (p < 0.001) and BDI scores (p = 0.012). Furthermore, the IMT group demonstrated superior gains in the SF-36 domains of Vitality (p = 0.049) and Physical Function (p = 0.008), highlighting specific benefits of inspiratory muscle training (Table 3).
Discussion
This study assessed the potential advantages of IMT for individuals with AS, a chronic inflammatory condition primarily affecting the axial skeleton 4,5. Our randomized controlled trial involved 40 patients allocated to either CE alone or IMT combined with CE. Baseline demographic and disease-specific characteristics were comparable between the groups, mitigating potential confounding 14,15,16 and supporting the attribution of outcomes to the interventions 7,17. Both exercise regimens demonstrated excellent tolerability; no adverse events led to participant withdrawal, indicating a favorable safety profile for these approaches in the AS population 18,19 and bolstering the reliability of our follow-up assessments 17.
Following the 20-day intervention, participants in both the CE and IMT groups exhibited significant clinical improvement. We observed notable enhancements in disease activity (BASDAI), functional status (BASFI), pain levels (VAS), and thoracic mobility (chest expansion). Psychological well-being, measured by the BDI, also improved significantly within both cohorts. Both groups improved in SF-36 General Health, Pain, and Physical Function domains, with IMT also enhancing Vitality and Emotional Role. These positive responses align with extensive evidence supporting structured exercise in AS management 2,14,20,21,22. Furthermore, Peak Expiratory Flow (PEF) showed beneficial changes. The gains achieved over this relatively brief period suggest that even focused, short-term rehabilitation can yield meaningful results in patients with AS. While other pulmonary function tests did not reach statistical significance here, improvements have been noted in other programs, often with longer durations 7,8,14.
The primary objective was to evaluate whether IMT provided distinct benefits over CE alone. Comparison of change scores revealed significant advantages for the IMT group in key outcomes. The significant improvement in chest expansion with IMT (p < 0.001) reflects its targeted effect on respiratory mechanics, often impaired in AS 23. Mechanistically, this may be attributed to enhanced diaphragmatic function and strengthening of intercostal muscles, which act directly against the costovertebral joint rigidity characteristic of the disease. Notably, the IMT group showed a greater reduction in depressive symptoms (BDI scores, p = 0.012). This enhanced psychological benefit may stem from several factors; beyond potentially improved oxygenation, the reduced physiological work of breathing can decrease exertional dyspnea and associated anxiety, contributing to a better sense of well-being and vitality 5,22. Additionally, the IMT group demonstrated superior gains in SF-36 Vitality (p = 0.049) and Physical Function (p = 0.008) domains (Table 3).
These findings provide valuable clinical insights. The marked improvement in chest expansion with IMT underscores its efficacy in addressing thoracic mobility limitations, a hallmark of AS, despite mixed results in prior studies on standard pulmonary function tests 5,7,9. The enhanced psychological outcomes (BDI, SF-36 Vitality) align with evidence linking exercise to improved mood in chronic diseases 23 and suggest IMT may offer unique benefits, potentially through better respiratory efficiency or reduced fatigue 17. The improved SF- 36 Physical Function further indicates a link between enhanced respiratory capacity and overall functional ability, a connection not consistently observed in previous AS exercise research 8. Conversely, within this study’s timeframe, adding IMT did not lead to significantly better outcomes than CE alone for VAS pain, BASDAI, BASFI, PEF, or the remaining SF-36 subscales. While some investigations have reported superior BASDAI improvements with IMT 5,7, our data did not replicate this. This discrepancy could be attributable to differences in study design; for instance, our 20-day intervention, while intensive, may have been insufficient to impact the systemic inflammatory processes reflected in the BASDAI, whereas longer protocols in other studies might have allowed such effects to emerge. Additionally, variations in baseline disease activity or patient characteristics across cohorts could influence the responsiveness of this outcome measure. The absence of a between-group difference in PEF concurs with certain studies
5 but differs from others 7,9, highlighting the existing heterogeneity in the literature.
Limitations
This study has several limitations that warrant consideration. This investigation utilized a relatively condensed 20-day intervention period and included 40 participants from a single center. Although this duration permitted the detection of significant changes, and the sample size is comparable to other initial AS exercise trials [3,5,20], longer programs and larger, multi-center cohorts are needed to increase statistical power and improve the generalizability of these findings [6,8,15]. Furthermore, the use of a novel device in the IMT group introduces the potential for a placebo or attention effect, which may have influenced subjective outcomes like the BDI and SF- 36 scores. Future trials should incorporate a sham-IMT group, using a device with negligible resistance, to control for this possibility and isolate the specific physiological effects of the training. It is important to note, however, that the total number of intervention sessions (n = 20) was substantial, and crucially, each session was conducted under direct physician supervision, ensuring high protocol fidelity. These initial results offer a valuable foundation for planning subsequent, more extensive investigations [17].
Conclusion
In conclusion, while both CE alone and IMT combined with CE effectively improved multiple clinical outcomes in patients with AS, our findings suggest that incorporating device-based IMT provides specific, significant advantages. These were most evident in enhancing chest expansion, alleviating depressive symptoms, and improving the vitality and physical function aspects of quality of life [24,25]. Consequently, IMT emerges as a potentially valuable adjunctive therapy in AS management. It may be particularly beneficial for patients with significant respiratory involvement or psychological distress. From a practical standpoint, the initial phase of IMT may benefit from clinical supervision to ensure proper technique and resistance progression, as was done in our trial. However, once proficiency is achieved, IMT holds significant potential as a component of a structured home-based exercise program, potentially increasing long-term accessibility and adherence. Future research should aim to confirm these effects in larger, more diverse populations over extended follow-up periods.
Figures

Figure 1. The Respifit-S® device Is used for inspiratory muscle training
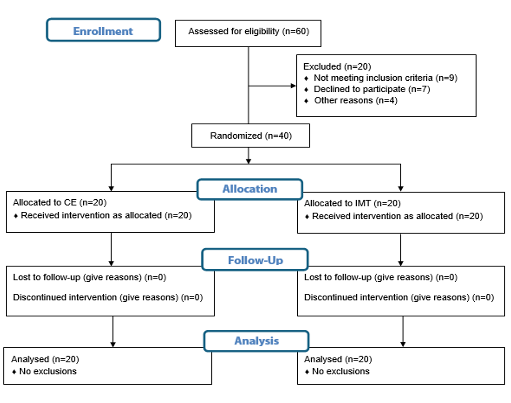
Figure 2. CONSORT flow diagram of the inspiratory muscle training study in ankylosing spondylitis patients
Tables
Table 1. Baseline demographic characteristics of patients
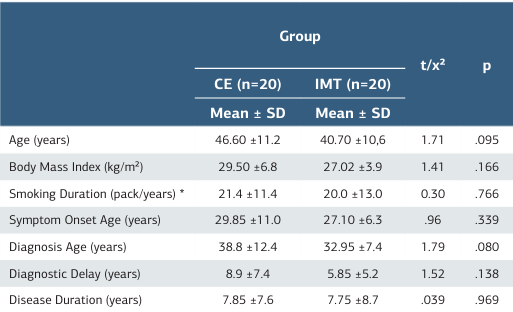
CE: Conventional Exercise Group; IMT: Inspiratory Muscle Training Group; SD: Standard Deviation. *Calculated among smokers only. t: t-test, χ²: Chi-square, p: Significance (α = 0.05). No significant differences between groups at baseline (p > 0.05).
Table 2. Pre- and post-treatment changes within groups
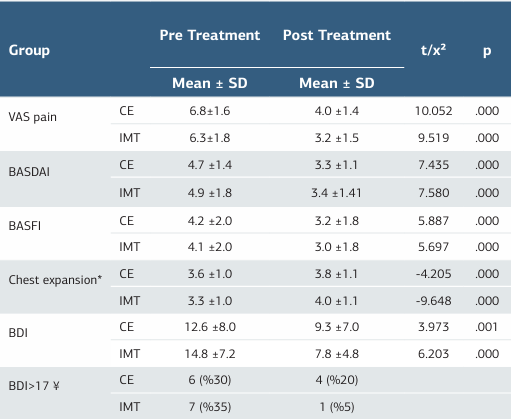
CE: Conventional Exercise Group; IMT: Inspiratory Muscle Training Group; SD: Standard Deviation. t: t-test, χ²: Chi-square, p: Significance (α = 0.05). VAS: Visual Analog Scale score, used for pain. BDI: Beck Depression Inventory Scores. * Chest expansion measure- ment in centimeters. BASFI: Bath Ankylosing Spondylitis Functional Index score. BASDAI: Bath Ankylosing Spondylitis Disease Activity Index score. ¥: Number of patients who have BDI scores >17.
Table 3. Between-group comparison of changes in parameters
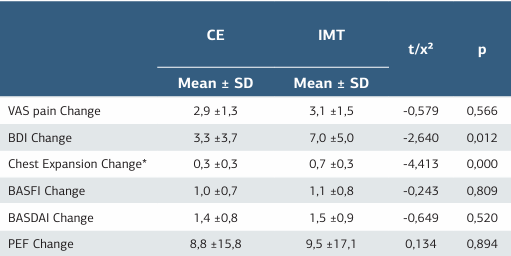
CE: Conventional Exercise Group; IMT: Inspiratory Muscle Training Group; SD: Standard Deviation. t: t-test, χ²: Chi-square, p: Significance (α = 0.05). VAS: Visual Analog Scale score, used for pain. BDI: Beck Depression Inventory Scores. *Change in chest expansion measurement in centimeters. BASFI: Bath Ankylosing Spondylitis Functional Index score. BASDAI: Bath Ankylosing Spondylitis Disease Activity Index score. PEF: Peak Expiratory Flow.
References
-
Ramiro S, Nikiphorou E, Sepriano A, et al. ASAS-EULAR recommendations for the management of axial spondyloarthritis 2022 update. Ann Rheum Dis. 2023;82(1):19-34. doi:10.1136/ard-2022-223296.
-
Szewczyk D, Sadura-Sieklucka T, Tarnacka B, Targowski T. Influence of manual therapy and stretching exercises on mobility status and pulmonary function tests among patients with ankylosing spondylitis. Med Rehabil. 2023;27(3):60-5. doi:10.5604/01.3001.0054.0124.
-
Bağlan Yentür S, Saraç DC, Sari F, et al. The effects of Pilates training on respiratory muscle strength in patients with ankylosing spondylitis. Physiother Theory Pract. 2024;40(1):31-41. doi:10.1080/09593985.2022.2109540.
-
Dimofte G-C, Ciobotaru C, Iliescu M-G, Albadi I, Lupu A-A. Evaluation of respiratory rehabilitation in patients with ankylosing spondylitis. ARS Medica Tomitana. 2022;28(4):163-70. doi:10.2478/arsm-2022-0035.
-
Basakci Calik B, Gur Kabul E, Taskin H, et al. The efficiency of inspiratory muscle training in patients with ankylosing spondylitis. Rheumatol Int. 2018;38(9):1713-20. doi:10.1007/s00296-018-4093-2.
-
Millner JR, Barron JS, Beinke KM, et al. Exercise for ankylosing spondylitis: An evidence-based consensus statement. Semin Arthritis Rheum. 2016;45(4):411-27. doi:10.1016/j.semarthrit.2015.08.003.
-
Dragoi RG, Amaricai E, Dragoi M, Popoviciu H, Avram C. Inspiratory muscle training improves aerobic capacity and pulmonary function in patients with ankylosing spondylitis: a randomized controlled study. Clin Rehabil. 2016;30(4):340-6. doi:10.1177/0269215515578292.
-
So MW, Heo HM, Koo BS, Kim YG, Lee CK, Yoo B. Efficacy of incentive spirometer exercise on pulmonary functions of patients with ankylosing spondylitis stabilized by tumor necrosis factor inhibitor therapy. J Rheumatol. 2012;39(9):1854-8. doi:10.3899/jrheum.120137.
-
Wong ML, Anderson RG, Garcia K, et al. The effect of inspiratory muscle training on respiratory variables in a patient with ankylosing spondylitis: a case report. Physiother Theory Pract. 2017;33(10):805-14. doi:10.1080/09593985.2017.1346023.
-
Calin A, Garrett S, Whitelock H, et al. A new approach to defining functional ability in ankylosing spondylitis: the development of the Bath Ankylosing Spondylitis Functional Index. J Rheumatol. 1994;21(12):2281-5.
-
Garrett S, Jenkinson T, Kennedy LG, Whitelock H, Gaisford P, Calin A. A new approach to defining disease status in ankylosing spondylitis: the Bath Ankylosing Spondylitis Disease Activity Index. J Rheumatol. 1994;21(12):2286-91.
-
Hisli N. Beck Depresyon Envanteri’nin üniversite öğrencileri için geçerliği, güvenirliği [Validity and reliability of the Beck Depression Inventory for university students]. TPD. 1989;7(23):3-13.
-
Koçyiğit H, Aydemir Ö, Fişek G, Ölmez N, Memiş A. Kısa Form-36 (KF-36)’nın Türkçe versiyonunun güvenilirliği ve geçerliliği [Reliability and Validity of the Turkish Version of Short Form-36 (SF-36)]. İlaç Tedavi Derg.1999;12(2):102-6.
-
Dulger S, Aykurt Karlibel I, Kasapoglu Aksoy M, Altan L, Sengoren Dikis O, Yildiz T. How does smoking cessation affect disease activity, function loss, and quality of life in smokers with ankylosing spondylitis? J Clin Rheumatol. 2019;25(7):288-96. doi:10.1097/rhu.0000000000000851.
-
Lim JM, Cho OH. Effects of home-and-workplace combined exercise for patients with ankylosing spondylitis. Asian Nurs Res (Korean Soc Nurs Sci). 2021;15(3):181-8. doi:10.1016/j.anr.2021.03.001.
-
van der Esch M, van’t Hul AJ, Heijmans M, Dekker J. Respiratory muscle performance as a possible determinant of exercise capacity in patients with ankylosing spondylitis. Aust J Physiother. 2004;50(1):41-5. doi:10.1016/s0004- 9514(14)60247-6.
-
Tomas-Carus P, Biehl-Printes C, Del Pozo-Cruz J, Parraca JA, Folgado H, Perez- Sousa MA. Effects of respiratory muscle training on respiratory efficiency and health-related quality of life in sedentary women with fibromyalgia: a randomised controlled trial. Clin Exp Rheumatol. 2022;40(6):1119-26. doi:10.55563/ clinexprheumatol/0v55nh.
-
Defi IR, Gultom C, Chorman MJ, Jennie J. High-intensity interval training can improve hand grip strength, inspiratory muscle, and quality of life in systemic sclerosis subjects. Reumatologia. 2021;59(2):98-103. doi:10.5114/ reum.2021.105454.
-
Zwaag J, Naaktgeboren R, van Herwaarden AE, Pickkers P, Kox M. The effects of cold exposure training and a breathing exercise on the inflammatory response in humans: a pilot study. Psychosom Med. 2022;84(4):457-67. doi:10.1097/ psy.0000000000001065.
-
Akaltun MS, Altindag O, Gur A. The effect of pulmonary rehabilitation programme on work productivity and clinical parameters in patients with ankylosing spondylitis. Int J Clin Pract. 2021;75(8):e14279. doi:10.1111/ ijcp.14279.
-
Çuni B, Çetin A. The effects of home-based exercises on muscle strength in ankylosing spondylitis patients treated with or without anti-TNF alpha. J PMR Sci. 2022;25(1):73-81. doi:10.31609/jpmrs.2021-83989.
-
Ortancil O, Sarikaya S, Sapmaz P, Basaran A, Ozdolap S. The effect(s) of a six-week home-based exercise program on the respiratory muscle and functional status in ankylosing spondylitis. J Clin Rheumatol. 2009;15(2):68-70. doi:10.1097/ rhu.0b013e31819b5ed0.
-
Jensen MK, Andersen SS, Andersen SS, Liboriussen CH, Kristensen S, Jochumsen M. Modulating heart rate variability through deep breathing exercises and transcutaneous auricular vagus nerve stimulation: a study in healthy participants and in patients with rheumatoid arthritis or systemic lupus erythematosus. Sensors (Basel). 2022;22(20):7884. doi:10.3390/s22207884.
-
Ozmen I, Yildirim E, Karakis M, Ozturk M, Aydin R, Sahal E. Are the gains from pulmonary rehabilitation the same in idiopathic pulmonary fibrosis and other interstitial lung diseases? Sarcoidosis Vasc Diffuse Lung Dis. 2024;41(3):e2024038. doi:10.36141/svdld.v41i3.15530.
-
Sari F, Oskay D, Tufan A. The effect of respiratory muscle training on respiratory muscle strength, diaphragm thickness/mobility, and exercise capacity in patients with systemic lupus erythematosus and associated shrinking lung syndrome. Lupus. 2024;33(3):289-92. doi:10.1177/09612033241226755.
Declarations
Scientific Responsibility Statement
The authors declare that they are responsible for the article’s scientific content, including study design, data collection, analysis and interpretation, writing, and some of the main line, or all of the preparation and scientific review of the contents, and approval of the final version of the article.
Animal and Human Rights Statement
All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Funding
None
Conflict of Interest
The authors declare that there is no conflict of interest.
Ethics Declarations
This study was approved by the Ethics Committee of Necmettin Erbakan University, Meram Faculty of Medicine, Konya, Türkiye (Date: 2012-10-5, No: 2012/243)
Acknowledgment
This article is derived from the medical specialty thesis of Dr. Ender Salbaş, completed at Necmettin Erbakan University, Meram Faculty of Medicine, Department of Physical Medicine and Rehabilitation (Thesis No: 340929, Year: 2013).
Data Availability
The datasets used and/or analyzed during the current study are not publicly available due to patient privacy reasons but are available from the corresponding author on reasonable request.
Additional Information
Publisher’s Note
Bayrakol MP remains neutral with regard to jurisdictional and institutional claims.
Rights and Permissions
About This Article
How to Cite This Article
Ender Salbaş, Hatice Uğurlu. Efficacy of device-based inspiratory muscle training as an adjunct therapy in ankylosing spondylitis patients: a randomized controlled trial. Ann Clin Anal Med 2026;17(1):43-48
Publication History
- Received:
- September 12, 2025
- Accepted:
- October 20, 2025
- Published Online:
- November 1, 2025
- Printed:
- January 1, 2026

