The surgical outcomes of femur segmenter fractures: femur shaft and neck fracture combination
Fixation strategies in combined femoral neck and shaft fractures
Authors
Abstract
Aim In the presence of a femoral neck fracture in the same extremity, in addition to a femoral shaft fracture, treatment management is complex and carries challenges in terms of orthopedic surgery. There is no clear consensus on treatment management. The aim of this study was to evaluate the surgical outcomes in patients with this fracture combination.
Methods Patients aged between 18-65 years with femur shaft and neck fractures combination were evaluated within the scope of the study. The patients were evaluated in terms of age, gender, trauma type, implant type, fracture classification, and postoperative complications. Functional results were evaluated using the Friedman and Wyman criteria.
Results The data of 18 patients were evaluated within the scope of the study. 15 (83.3%) of the patients were male and 3 (16.7%) were female, and the mean age was 38.16 (18-62). The mean follow-up period was 36.38 (24-60) months. In the study group, there was no statistically significant relationship between the development of nonunion, avascular necrosis of the femoral head, the type of fracture of the femoral shaft and neck, and the type of implant used in the treatment (p > 0.05). Additionally, there was no statistically significant correlation between the type of implant used and the Friedman and Wyman criteria (p > 0.05).
Conclusion The presence of a femoral shaft fracture in addition to a femoral neck fracture complicates the treatment process. Different implant combinations can be preferred.
Keywords
Introduction
The presence of an ipsilateral neck fracture can be seen in up to 9% of femoral shaft cases 1. This combination of fractures, which usually occurs as a result of high-energy trauma, mostly consists of young men 2. Fracture fixation is difficult due to the segmental nature of the fracture pattern, and therefore, a combination of various methods may be preferred in the fracture fixation process, as in other anatomical fractures of the femur 3,4. In addition to the fracture, the risk of additional injuries in different body systems may be up to 75% due to the high-energy injury pattern 5. There is no clear consensus in terms of treatment models, and each method carries its own risk of complications 6. While each of the fracture patterns requires a lot of attention even when alone, the process becomes more complicated in the case of the combination of these two fractures.
In this study, we aim to evaluate the surgical treatment results in patients with femoral shaft fractures and femoral neck fractures.
Materials and Methods
The records of patients who applied to our orthopedics and traumatology department with a combination of a femoral shaft fracture and the same side femur neck fracture were reviewed retrospectively after the approval of the ethics committee, and the study was performed in accordance with the Helsinki declaration. Patients aged between 18 and 65 years of age, with a minimum of 24 months of data, the presence of a neck fracture in the same extremity in addition to a femoral shaft fracture, no neurological deficits, no traumatic brain injury, and those who applied to our emergency department within the first 24 hours after injury were included in the study. If there was a pathological fracture, the patient’s age was over 65 years, and the fracture pattern was the presence of a Gustilo-Anderson type 3 open fracture, these patients were excluded from the study.
The patients included in the study were evaluated in terms of gender, age, follow-up time, type of trauma, type of implant used in fracture fixation, union time, and postoperative complications. Garden classification and Pauwels classification were used for femoral neck fracture, AO classification for femoral shaft fracture, and Gustilo-Anderson classification in case of open fracture. In addition, the Friedman and Wyman criteria were used when evaluating functional results.
All patients were first evaluated in the emergency department. In accordance with the trauma protocol, abdominal and chest trauma examinations were also performed, and the principle of damage-controlled surgery was observed. When the patient’s vital signs were met with optimal conditions, the final fixation phase was initiated. (Figures 1, 2, 3)
Postoperative follow-ups were made with X-ray, and patients with fracture healing findings in 3 of 4 bone cortices were considered to have achieved union. Patients who did not have callus findings radiologically in their 6 six-month follow-up were accepted as non-union.
Statistical Analysis
Descriptive statistics for baseline and outcome data are reported. The comparison of two independent groups was analyzed with the t-test and the Mann-Whitney U test. The significance level was taken as p<0.05 in all statistical analyses. IBM SPSS version 22.0 (IBM Corp, Armonk, NY, USA) software was used for data analysis.
Informed Consent
Given the retrospective nature of the study, informed consent was not required from patients.
Ethical Approval
This study was approved by the Ethics Committee of Gaziantep University (Date: 2022-09-03, No: 2022/57).
Results
The data of 18 patients who met the study criteria were scanned. Fifteen (83.3%) of the patients were male, and 3 (16.7%) were female. The mean age of the patient group was 38.16 (18-62), and the mean follow-up period was 36.38 (24-60) months. When we look at the type of trauma in the patient group, 15 patients (83.33%) were caused by a motorcycle accident, and it was seen that the reason was falling from a height in 3 patients (16.67%). Nine (50%) patients in the study group had injuries involving the abdomen, chest, head, and other extremities. When the femoral neck fractures in the patient group were evaluated according to the garden classification, 3 patients were type 2 (16.7%), 11 patients were type 3 (61.1%), 4 patients were type 4 (22.2%), and according to the Pauwels classification, 1 patient was type 1 (5.6%), 6 patients were type 2 (33.3%) and 11 patients were type 3 (61.1%). When the femoral shaft fractures were evaluated according to the AO classification, 8 patients were type A (44.4%), 8 patients were type B (44.4%), and 2 patients were type C (11.2%). When femoral shaft fractures were evaluated in terms of open fractures, 3 patients (16.66%) were in the type 2 group according to the Gustilo-Anderson classification, and the remaining 15 patients (83.37%) were found to have closed fractures.
The mean time to union was 5.5 (3-10) months in femoral shaft fractures and 3 (2-5) months in femoral neck fractures. In the presence of a femoral neck fracture, a cannulated screw was used in 13 patients (72.2%), a dynamic hip screw (DHS) in 1 patient (5.6%), intramedullary nailing in 1 patient (5.6%), and in 3 patients (16.7%), proximal femoral nailing (PFN) was preferred. In the presence of femoral shaft fracture, retrograde intramedullary nailing in 7 patients (38.9%), antegrade nailing in 3 patients (16.7%), LC-DCP plate in 3 patients (16.7%), PFN in 2 patients (11.1%), and external fixator in 3 patients (16.7%) was preferred. Femoral shaft fractures of these 3 (16.7%) patients who were treated with an external fixator were in the type 2 group according to the Gustilo-Anderson classification. In the next step, fixation with the LC-DCP plate was applied to these patients. Eight different combinations of fracture fixation methods were used in 18 patients. In terms of complications, one patient with a femoral shaft fracture (5.6%) had nonunion, and one patient (5.6%) had superficial infection. Nonunion was detected in 1 patient (5.6%) with a femoral neck fracture, and femoral head avascular necrosis was detected in 2 patients (11.11%). In one patient who was diagnosed with non-union in terms of a femoral shaft fracture in the follow-ups, revision was performed with antegrade nail exchange, and union was observed in the follow-ups. One patient who developed a superficial infection was treated with antibiotic therapy.
Total hip arthroplasty was performed in 1 patient who was diagnosed with nonunion and 2 patients with avascular necrosis in the follow-up after femoral head fracture. When functional results are examined with Friedman and Wyman criteria, 3 patients (16.66%) had poor results, 2 patients (11.11%) had moderate results, and 13 patients (72.23%) had good results. The relationship between the type of femoral neck fracture and the development of nonunion according to the Garden and Pauwels classification, and between the type of femoral shaft fracture and the development of nonunion according to the AO classification, was not statistically significant (p = 0.117; p = 0.491; p = 0.175). (Table 1) The relationship between the development of nonunion and the preferred implant type in the treatment of femoral neck and shaft fractures was not statistically significant (p = 0.119; p = 0.147).
The relationship between the preferred implant type in the treatment of combined femoral shaft and neck fractures and the Friedman and Wyman criteria was not statistically significant (p = 0.38; p = 0.42). Also, for femoral shaft and neck fracture, no statistically significant relationship could be established between the type of implant used and the union time (p = 0.19; p = 0.42).
Discussion
In this study, we evaluated the surgical results of patients with femoral shaft and neck fractures in the ipsilateral extremity. Our study results showed us that there can be many different treatment combinations in terms of treatment modalities.
The cause of femoral neck fractures accompanying femoral shaft fractures is mostly a high-energy trauma, and the patient group is predominantly young men 7. The combination of these fractures causes the treatment process to become more complex. Treatment options include the use of cannulated screws, DHS, and PFN for femoral neck fractures, in addition to antegrade IMN, retrograde IMN, and plating options for femoral shaft fractures 8. In our study, treatment planning was carried out with 8 different implant combinations. The advantages and disadvantages of each treatment modality are defined according to their biomechanical properties. The major complication for femoral shaft fractures has been defined as nonunion and can be seen in up to 10%. In addition, complication rates such as avascular necrosis, union of varus, and nonunion that may be experienced during the treatment processes of femoral neck fractures can reach 25% 9.
The data in our study, in line with the literature, showed that the young male patient group was more affected. Treatment management in cases with neck fracture in addition to femoral shaft fracture is more complex, and the risk of complications is higher than in cases with only femoral shaft fracture 10. The importance of anatomic reduction in the treatment of femoral neck fracture and the risk of avascular necrosis are among the reasons for this condition 11. Another issue that determines the treatment strategy is which fracture should be fixed first. It has been suggested that prioritizing fixation in non-displaced femoral neck fractures reduces possible complications 12.In the presence of a displaced femoral neck fracture, it is more appropriate to prioritize the fixation of the femoral shaft fracture. In the cases in our study group, treatment planning was made in line with this surgical principle. In our cases, the fixation method with a cannulated screw was mainly preferred in femoral neck fracture fixation. In their meta-analysis, Xia et al. evaluated the case results of fixation with DHS and cannulated screws in the 1662 patient group and reported that avascular necrosis was seen at a lower rate in the cannulated screw group, and there was no difference in terms of nonunion 13. In our patient group, the choice of fixation was DHS in 1 patient who developed nonunion. Fixation with DHS and PFN was observed in 2 patients who developed avascular necrosis. Current data still show that the rate of femoral head avascular necrosis can reach 6% and nonunion rates can reach 20% in these fracture associations 14. In cases of femoral shaft fracture, our predominant preference was retrograde IMN. The anatomical localization of the fracture in the patient group and the thought that it would be easier to intervene in two fractures in the same extremity in case of need for revision were effective in our selection. The literature has reported that the need for revision is seen at a lower rate when these two fractures are combined with 2 different implant selections 15. In the combination of femoral shaft and neck fracture, the incidence of femoral shaft nonunion can be seen between 3% and 10% 16. In this respect, the rate of cases diagnosed with femoral shaft nonunion in our study is compatible with the literature. Mohapatra et al. evaluated the patient group according to the Friedman and Wyman criteria in their prospective study on 18 patients and reported poor results in 2 patients (11.12%) and good results in 13 patients (72.22%) 17. Kharel et al. reported poor results in 2 patients (8.34%) and good results in 16 patients (66.66%) in their study on 24 patients 18. In this respect, our study results are compatible with the literature. In addition, in these studies, good outcome rates are seen in 72%, and functionally poor results can be seen in the remaining 28% of the patient group. This result shows the importance of planning and surgical management in treatment processes.
Limitations
In addition to the number of patients and patient distribution, the high number of preferred implant combination types constitutes a limitation of the study. In addition, the number of patients and the small distribution of groups may be a factor that complicates the statistical data analysis.
Conclusion
In the presence of a femoral neck fracture in addition to a femoral shaft fracture, different implant types can be used in combination in the treatment selection. If the femoral neck fracture is non-displaced, the priority is fixation of this fracture. If it is displaced, it is appropriate to give priority to the femoral shaft fracture.
Figures
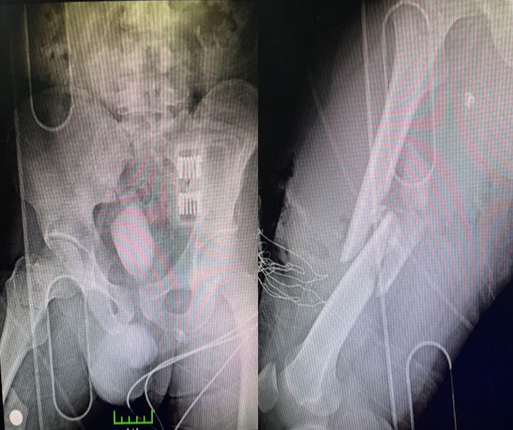
Figure 1. 38-year-old male patient. Applying to the emergency room after a traffic accident. A femoral neck fracture and an ipsilateral femoral shaft comminuted fracture are present

Figure 2. First, the cannula is screwed for the femoral neck fracture of the patient. An external fixator is applied for a femoral shaft fracture with the idea of damage-controlled surgery

Figure 3. First-year anteroposterior X-ray images of the patient who was followed up postoperatively
References
-
Alho A. Concurrent ipsilateral fractures of the hip and shaft of the femur. A systematic review of 722 cases. Ann Chir Gynaecol. 1997;86(4):326-36.
-
Tornetta P, 3rd, Kain MS, Creevy WR. Diagnosis of femoral neck fractures in patients with a femoral shaft fracture. Improvement with a standard protocol. J Bone Joint Surg Am. 2007;89(1):39-43. doi:10.2106/JBJS.F.00297.
-
Jones CB, Walker JB. Diagnosis and management of ipsilateral femoral neck and shaft fractures. J Am Acad Orthop Surg. 2018;26(21):e448-e454. doi:10.5435/ JAAOS-D-17-00497.
-
Erinc S, Cam N, Kanar M, Mustafa Ozdemir H. Comparison of two surgical techniques for periprosthetic supracondylar femoral fractures: Minimally invasive locking plate versus retrograde femoral nails. Med Bull Sisli Etfal Hosp. 2021;55(4):477-85. doi:10.14744/semb.2021.34270.
-
Cannada LK, Viehe T, Cates CA, et al. A retrospective review of high-energy femoral neck-shaft fractures. J Orthop Trauma. 2009;23(4):254-60. doi:10.1097/BOT.0b013e31819a6651.
-
Wolinsky PR, Johnson KD. Ipsilateral femoral neck and shaft fractures. Clin Orthop Relat Res. 1995;(318):81-90.
-
Tsai CH, Hsu HC, Fong YC, Lin CJ, Chen YH, Hsu CJ. Treatment for ipsilateral fractures of femoral neck and shaft. Injury. 2009;40(7):778-82. doi:10.1016/j. injury.2009.03.009.
-
Gupta A, Jain A, Mittal S, Chowdhury B, Trikha V. Ipsilateral femoral neck and shaft fractures: case series from a single Level-I trauma centre and review of literature. Eur J Orthop Surg Traumatol. 2023;33(4):803-9. doi:10.1007/s00590- 021-03199-3.
-
Lu Y, Wang Y, Song Z, et al. Treatment comparison of femoral shaft with femoral neck fracture: a meta-analysis. J Orthop Res. 2020;15(1):19. doi:10.1186/ s13018-019-1496-z.
-
Watson JT, Moed BR. Ipsilateral femoral neck and shaft fractures: complications and their treatment. Clin Orthop Relat Res. 2002;(399):78-86. doi:10.1097/00003086-200206000-00011.
-
Kumar S, Geevarughese NM, Rajnish RK, Lakshminarayana S, Aggarwal AN, Ul Haq R. Outcomes of displaced, comminuted, intracapsular neck femur fracture in young adults managed with three screw inverted triangle versus four screw diamond configuration: A comparative pilot study. Indian J Orthop. 2022;56(4):566-72. doi:10.1007/s43465-021-00558-4.
-
Hak DJ, Mauffrey C, Hake M, Hammerberg EM, Stahel PF. Ipsilateral femoral neck and shaft fractures: current diagnostic and treatment strategies. Orthopedics. 2015;38(4):247-51. doi:10.3928/01477447-20150402-05.
-
Xia Y, Zhang W, Zhang Z, Wang J, Yan L. Treatment of femoral neck fractures: sliding hip screw or cannulated screws? A meta-analysis. J Orthop Res. 2021;16(1):54. doi:10.1186/s13018-020-02189-1.
-
Oh CW, Kim JW, Park KC, et al. Clinical outcomes and affecting factors of ipsilateral femoral neck and shaft fractures - Multination, multicenter analysis. J Orthop Sci. 2023;28(3):614-20. doi:10.1016/j.jos.2021.12.021.
-
Bhandari M. Ipsilateral femoral neck and shaft fractures. J Orthop Trauma. 2003;17(2):138-40. doi:10.1097/00005131-200302000-00013.
-
Boulton CL, Pollak AN. Special topic: Ipsilateral femoral neck and shaft fractures--does evidence give us the answer? Injury. 2015;46(3):478-83. doi:10.1016/j.injury.2014.11.021.
-
Mohapatra N, Sethy G, Rana R. Ipsilateral fracture neck and shaft of femur: A prospective analysis of two methods. J Orthop Trauma. 2017;9(1):17. doi:10.4103/jotr.jotr_16_16.
-
Kharel KJIJOS. Ipsilateral femoral neck and shaft fractures: An analysis of two treatment methods. Int J Orthop Sci. 2017;3(2k):774-7. doi:10.22271/ortho.2017. v3.i3k.116.
Declarations
Scientific Responsibility Statement
The authors declare that they are responsible for the article’s scientific content, including study design, data collection, analysis and interpretation, writing, and some of the main line, or all of the preparation and scientific review of the contents, and approval of the final version of the article.
Animal and Human Rights Statement
All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Funding
None
Conflict of Interest
The authors declare that there is no conflict of interest.
Ethics Declarations
This study was approved by the Ethics Committee of Gaziantep University (Date: 2022-09-03, No: 2022/57)
Data Availability
The datasets used and/or analyzed during the current study are not publicly available due to patient privacy reasons but are available from the corresponding author on reasonable request.
Additional Information
Publisher’s Note
Bayrakol MP remains neutral with regard to jurisdictional and institutional claims.
Rights and Permissions
About This Article
How to Cite This Article
Bahri Bozgeyik, Sezgin Bahadır Tekin, Çağrı Karabulut. The surgical outcomes of femur segmenter fractures: femur shaft and neck fracture combination. Ann Clin Anal Med 2026;17(1):54-57
Publication History
- Received:
- October 11, 2025
- Accepted:
- November 18, 2025
- Published Online:
- December 4, 2025
- Printed:
- January 1, 2026

