A new approach: the effect of modified sutureless lateral pharyngoplasty technique on obstructive sleep apnea syndrome
The effect of modified sutureless lateral pharyngoplasty
Authors
Abstract
Aim The objective of our study is to compare the effectiveness of the modified sutureless lateral pharyngoplasty technique, when applied in addition to tonsillectomy, in children with obstructive sleep apnea syndrome.
Methods A retrospective analysis was conducted on 63 patients who underwent surgery at our clinic between May 2021 and June 2022. In the first group, the modified sutureless lateral pharyngoplasty technique was applied in addition to tonsillectomy for 30 patients. The second group, consisting of 33 patients, underwent tonsillectomy alone. Comparative evaluations between the groups were performed using preoperative and postoperative 6-month Modified Epworth Sleepiness Scale and Pediatric Sleep Scale.
Results In the preoperative period, there was no significant difference between the two groups regarding both scales (p = 0.504, p = 0.357). However, in the postoperative period, the group that underwent modified sutureless lateral pharyngoplasty exhibited significantly lower scores on both the modified Epworth sleepiness scale and the pediatric sleep scale (p = 0.011, p = 0.037). When comparing preoperative and postoperative scores within each group, significantly lower scores were observed for both scales in the postoperative period (p = 0.001).
Conclusion Our study reveals that the modified sutureless lateral pharyngoplasty technique can be regarded as a safe and effective alternative treatment method for children with sleep apnea by preserving the pharyngeal wall anatomy. This new approach may offer promising results in reducing obstructive sleep apnea symptoms.
Keywords
Introduction
Obstructive sleep apnea syndrome (OSAS) is a common childhood disorder with a prevalence of 1% to 3% 1. Adenotonsillar hypertrophy is the leading cause of upper airway obstruction in pediatric OSAS patients 2. Although daytime sleepiness is not a predominant symptom in children with OSAS, studies suggest variability in its prevalence 3. The condition is most frequently observed in children aged 3 to 8 years, with its incidence peaking during preschool. Adenotonsillectomy is the standard treatment for pediatric OSAS 4.
Many studies evaluating the effectiveness of adenotonsillectomy in pediatric OSAS have reported success rates ranging from 52.9% to 90.5% 5. However, despite its widespread use, adenotonsillectomy alone may not fully address lateral pharyngeal wall collapse, a key contributor to persistent OSAS symptoms in some patients. This limitation underscores the need for a more comprehensive yet minimally invasive surgical approach that optimizes airway patency while reducing operative time.
This study introduces Modified Sutureless Lateral Pharyngoplasty (MSLP) as an adjunct to tonsillectomy. MSLP aims to enhance upper airway stability by increasing the airway space between the tonsillar fossae while minimizing surgical invasiveness. We compare the outcomes of MSLP combined with tonsillectomy versus tonsillectomy alone to determine whether this novel technique provides superior benefits in managing pediatric OSAS.
Materials and Methods
We conducted a retrospective analysis of 63 patients diagnosed with OSAS at our otorhinolaryngology clinic between May 2021 and June 2022, following the criteria established by the American Academy of Sleep Medicine. We meticulously documented and analyzed demographic data, clinical examination findings, surgical history, and six-month assessments before and after surgery, which included the Modified Epworth Sleepiness Scale and the Pediatric Sleep Scale.
The study population was divided into two groups: Group 1 (n = 30) consisted of patients who underwent tonsillectomy combined with MSLP, while Group 2 (n = 33) included patients who had tonsillectomy alone. Exclusion criteria included adults, pediatric patients with syndromic features, acute infections, coagulopathy, craniofacial anomalies, prior adenotonsillectomy or adenoidectomy, a history of cleft lip or palate surgery, or prior partial tonsillectomy. All patients were followed for a minimum of six months. The Modified Epworth Sleepiness Scale and the Pediatric Sleep Scale were administered to the families of patients both preoperatively and at the six-month postoperative mark for a comprehensive evaluation.
Modified Epworth Sleepiness Scale
The mESS (An adaptation of the Epworth Sleepiness Scale), consists of eight scenarios where parents evaluate the likelihood of their child falling asleep: no chance (0 points), slight chance (1 point), moderate chance (2 points), or high chance (3 points). The total score, with a maximum of 24 points, is determined by summing the points from the eight responses.
Originally introduced in 2004 during a study on sleepiness in children with OSAS, the mESS underwent modifications in 2009. Notably, two situations were altered compared to the adult ESS: Situation 3 replaced “theater or a meeting” with “classroom or movie theater,” and Situation 7 excluded the words “without alcohol.” Situation 8, related to driving, assumes the child is a passenger, mirroring situation 4 (“As a passenger in a car for 1 h without a break”) 6,7,8.
This study primarily utilized the original 8-item mESS. To address the similarity between situations 4 and 8, the CHAT study incorporated two additional questions (“doing homework or taking a test” and “playing a video game”) to capture other common childhood experiences. These questions resulted in two additional versions of the mESS, referred to as mESS9 and mESS10.
It’s important to note that while a cut-off of > 10 on the original ESS is commonly employed in adults to indicate abnormal sleepiness, there is no widely accepted cutoff for children 6,7,8. Pediatric Sleep Questionnaire-Sleepiness Subscale The pediatric sleep questionnaire (PSQ), Sleep-Related Breathing Disorders Scale, encompasses 22 questions addressing snoring, excessive daytime sleepiness, and inattentive/hyperactive behaviors. It has been previously validated in both children with and without sleep-disordered breathing, demonstrating accurate classification in 86.4% of children. In one group, it achieved a sensitivity of 0.85 and specificity of 0.87, while in the second group, correct classification stood at 85% with a sensitivity of 0.81 and specificity of 0.87 9.
The Sleepiness Subscale (PSQ-SS) within the scale comprises four questions that explore feeling unrefreshed in the morning, difficulty while waking up, daytime sleepiness issues, and teacher-observed sleepiness. Responses are scored as 1 for “yes” and 0 for “no.” The overall score is obtained by dividing the total score by the number of non-missing responses (excluding “Don’t Know”). A score surpassing 0.33 indicates significant sleepiness 9.
Surgical Procedure
All surgeries were performed under general anesthesia with orotracheal intubation using an automatic mouth retractor by the same surgeon. Particularly, no local anesthetic injection was administered to either group. In Group 1, bilateral tonsillectomy was performed by excising tonsils with the cold knife technique, ensuring effective bleeding control. A special mucosal field, extending from the posterior plica mucosal fold to the uvula, was determined to align the anterior and posterior plica on the same plane when looking into the oropharynx. Subsequently, this mucosal field was excised by using bipolar cauterization (Figures 1,2).
Conversely, in Group 2, bilateral tonsillectomy was performed using the cold knife technique, and the procedure ended with successful bleeding control.
This technique took extremely little time, and we observed no additional morbidity except for mild uvula edema.
Statistical Analysis
The normal distribution of variables was tested with the Kolmogorov-Smirnov test. Parametric tests were applied for variables with normal distribution, and nonparametric tests were used for variables that did not display normal distribution. Comparison between two independent groups was performed through the Mann-Whitney U test. The Wilcoxon Signed-Rank test was used in intra-group analyses. Categorical variables underwent analysis with the Chi-square test. The statistical analyses were carried out using IBM SPSS Package Program version 26.0 (IBM Corporation, Armonk, NY, USA). Results are expressed as mean ± SD. A P-value less than 0.05 was considered statistically significant.
Ethical Approval
This study was approved by the Ethics Committee of Necmettin Erbakan University (Date: 2022-11-04, No: 4028).
Results
Sixty-three patients, 30 in group 1 and 33 in group 2, were included in the study. There were 12 female and 18 male patients in group 1 and 14 female and 19 male patients in group 2. The mean age of both groups was 6 years. In group 1, the ages of the patients ranged between 3 and 16 years. In group 2, the ages of the patients ranged between 3 and 13 years. There was no statistically significant difference between the groups in terms of age, gender, and OSAS grade (p > 0.05) (Table 1).
There were no significant differences between group 1 and group 2 in terms of the preoperative sleep scale (42 (40-44) vs 42 (40-44)) and preoperative mESS (23 (21-24) vs 23 (21- 24)) scores (p = 0.504 and p = 0.357, respectively). However, the postoperative sleep scale and postoperative mESS (5 (0-29) and 3 (0-12), respectively) were significantly lower (p = 0.011 and p = 0.037, respectively).
When intra-group comparisons were examined, it was found that the pediatric sleep scale and mESS postoperative scores were statistically significantly lower than preoperative scores (p < 0.001) (Table 2).
It was found that preoperative - postoperative differences in both the pediatric sleep scale and mESS were higher in group 1 than in group 2, and the differences were statistically significant (p = 0.015 and p = 0.037, respectively) (Table 2 ).
Discussion
Adenotonsillectomy is considered the most effective treatment method for children with OSAS who have adenotonsillar hypertrophy 10. The significant decrease in daytime sleepiness observed in children who underwent early adenotonsillectomy supported early intervention rather than close follow-up 11. The lateral pharyngeal wall plays a significant role in surgery for OSAS. Current surgical trends lean towards minimally invasive techniques 12.
Patients with OSAS frequently experience multi-level obstruction involving the palate, lateral pharyngeal wall, and base of the tongue. The surgical approach to OSAS in such patients should comprehensively address all these areas, particularly lateral pharyngeal wall collapse. In individuals with OSAS, the lateral pharyngeal walls tend to be more flexible and collapsible under air pressure compared to healthy individuals. A study on anterior pharyngoplasty suggests that incorporating the lateral wall in surgery increases the likelihood of successful intervention by % 60.6 13. Furthermore, in patients with OSAS, the lateral pharyngeal walls are often thicker, representing a crucial anatomical factor contributing to airway narrowing 14. Cahali et al. described the lateral pharyngoplasty procedure in 10 patients with moderate or severe OSAS and lateral pharyngeal wall collapse on clinical endoscopic examination 15. Cahali et al. reported that the mean Apnea-Hypopnea Index (AHI) value of cases before the procedure was 45.8, and the AHI value in the postoperative 8th month decreased to 15.2 15. Inspired by this study, we aimed to characterize this procedure as modified sutureless lateral pharyngoplasty. This involved excising the mucosal fold at the junction of the posterior plica and uvula, in addition to tonsillectomy. This method was chosen for its efficiency and tissue-sparing nature, offering a less invasive alternative to conventional techniques.
In a recent study, Karakoç et al. compared the effectiveness of anterior palatoplasty, lateral pharyngoplasty, and expansive sphincter palatoplasty (ESP) techniques. AHI value improved from 16.90 to 14.27 (p = 0.135) in anterior palatoplasty, from 17.69 to 12.05 in lateral pharyngoplasty (p = 0.004), and from 26.83 to 9.08 in ESP groups (p < 0.001). In conclusion, the authors concluded that although all techniques were effective in selected OSAS patients, the ESP technique was one step ahead of the other two techniques 16.
We present the Modified Sutureless Lateral Pharyngoplasty (MSLP) technique as an alternative to classical tonsillectomy, anticipating its potential advantages based on mESS and Pediatric Sleep Scale assessments in pediatric patients. Our study revealed that both techniques were beneficial, with MSLP demonstrating greater significance in improving sleep-related outcomes compared to classical tonsillectomy. Notably, MSLP neither significantly prolonged surgical time nor introduced additional morbidity.
We hypothesized that MSLP would offer advantages by reducing procedure time and increasing airway space between the tonsillar fossae, while also decreasing lateral pharyngeal wall collapse. In our clinical assessment, we employed the Modified Epworth Sleepiness Scale (mESS) and the Pediatric Sleep Scale. However, these subjective caregiver-reported tools have inherent limitations, as polysomnography (PSG) can be difficult to perform in pediatric patients. Incorporating objective parameters such as the apnea–hypopnea index (AHI) and oxygen saturation levels remains essential for a more comprehensive evaluation of the technique. Future studies should include preoperative polysomnography to determine whether MSLP produces comparable benefits in adult patients. In our technique, we prioritized preserving the anatomy of the upper airway. No significant short- or long-term complications were observed, except for moderate uvular edema, which resolved without intervention. Postoperative recovery and return to daily activities were similar between the MSLP and control groups. To the best of our knowledge, no previous studies have evaluated this technique in pediatric populations. Given its short operative time, minimal invasiveness, and preservation of anatomical integrity, MSLP appears suitable for integration into routine surgical practice in appropriately selected patients.
Limitations
This study has several limitations. First, the outcomes were assessed using subjective caregiver-reported scales (mESS and Pediatric Sleep Scale), as polysomnography could not be performed in pediatric patients. The absence of objective parameters such as AHI and oxygen saturation limits the strength of our findings. Second, the sample size was relatively small, and the lack of comparable studies in the literature reduces generalizability. Finally, the follow-up period may not have been sufficient to detect rare or delayed complications. Future studies incorporating preoperative PSG and larger cohorts are needed to validate the effectiveness of MSLP.
Conclusion
This study reveals that the MSLP technique can be considered as an alternative, safe, and effective treatment method by preserving the pharyngeal wall anatomy in children with obstructive sleep apnea. This new approach may offer optimal, promising results in the reduction of sleep apnea symptoms.
Figures
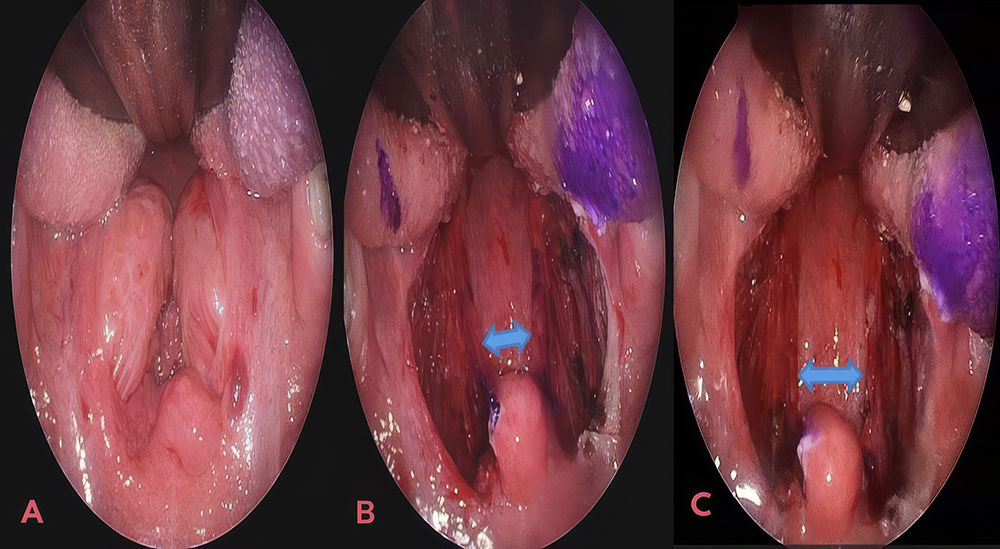
Figure 1. A: Preoperative view showing tonsillar hypertrophy, B: Post-tonsillectomy view, C: Postoperative view following Modified Sutureless Lateral Pharyngoplasty (MSLP) with tonsillectomy, demonstrating the widened airway space
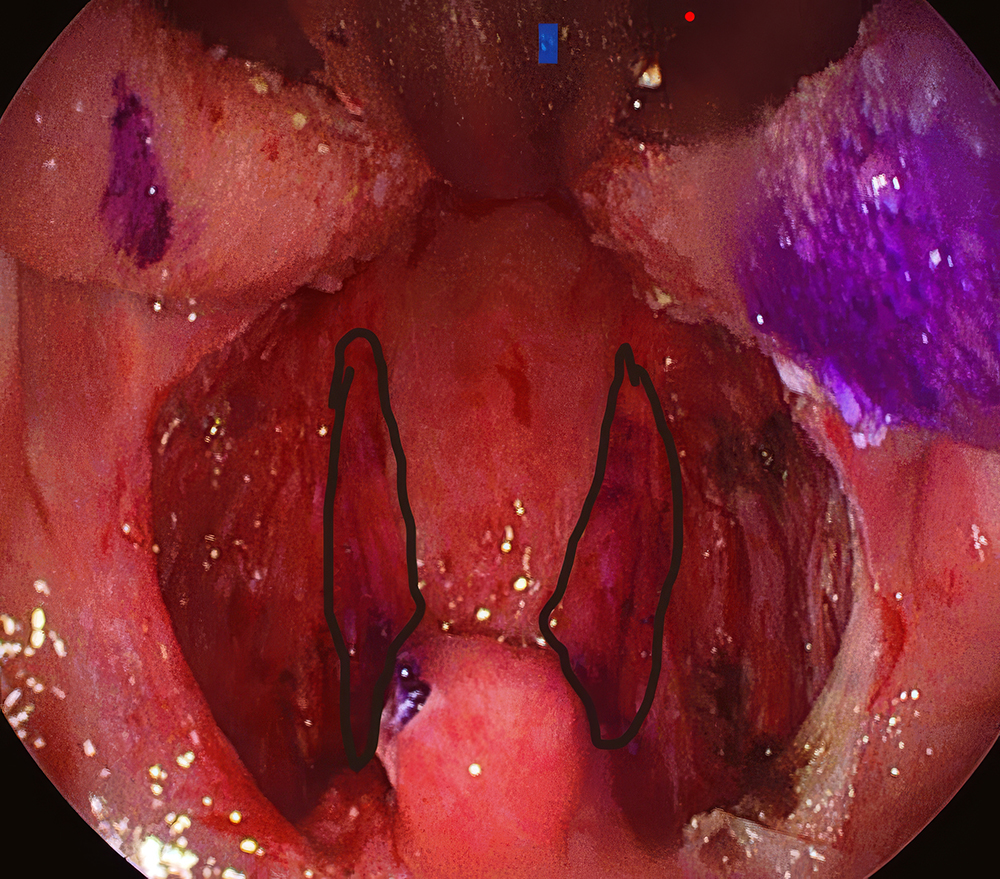
Figure 2. View of the surgical field resected with the modified lateral pharyngoplasty technique
Tables
Table 1. Comparison of age, gender, and tonsil grade values between groups
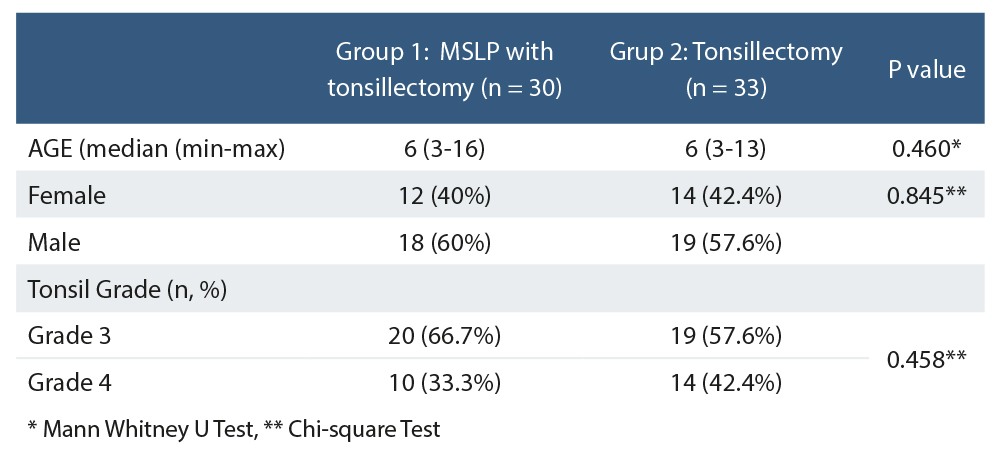
* Mann Whitney U Test, ** Chi-square Test
Table 2. Preoperations and postoperation comparison of the pediatric sleep scale and the mESS between and within groups
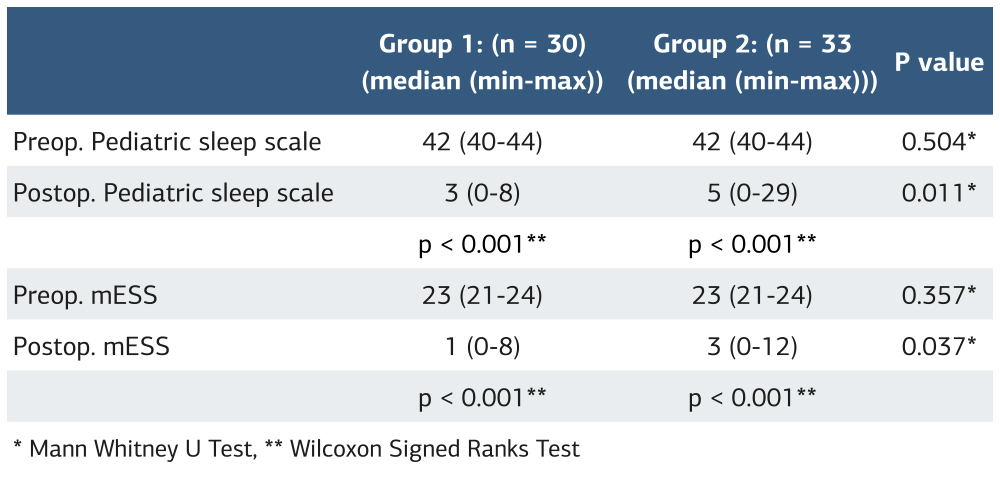
* Mann Whitney U Test, ** Wilcoxon Signed Ranks Test
References
-
Farber JM. Clinical practice guideline: diagnosis and management of childhood obstructive sleep apnea syndrome. Pediatrics. 2002;110(6):1255-7. doi:10.1542/peds.110.6.1255-a.
-
Martin J, Hiscock H, Hardy P, Davey B, Wake M. Adverse associations of infant and child sleep problems and parent health: an Australian population study. Pediatrics. 2007;119(5):947-55. doi:10.1542/peds.2006-2569.
-
Melendres MC, Lutz JM, Rubin ED, Marcus CL. Daytime sleepiness and hyperactivity in children with suspected sleep-disordered breathing. Pediatrics. 2004;114(3):768-75. doi:10.1542/peds.2004-0730.
-
Marcus CL, Brooks LJ, Draper KA, et al. Diagnosis and management of childhood obstructive sleep apnea syndrome. Pediatrics. 2012;130(3):e714-55. doi:10.1542/peds.2012-1672.
-
Guilleminault C, Li KK, Khramtsov A, Pelayo R, Martinez S. Sleep disordered breathing: surgical outcomes in prepubertal children. Laryngoscope. 2004;114(1):132-7. doi:10.1097/00005537-200401000-00024.
-
Anderson B, Storfer-Isser A, Taylor HG, Rosen CL, Redline S. Associations of executive function with sleepiness and sleep duration in adolescents. Pediatrics. 2009;123(4):e701-7. doi:10.1542/peds.2008-1182.
-
Chan EY, Ng DK, Chan CH, et al. Modified epworth sleepiness scale in chinese children with obstructive sleep apnea: a retrospective study. Sleep Breath. 2009;13(1):59-63. doi:10.1007/s11325-008-0205-7.
-
Gonçalves MT, Malafaia S, Moutinho Dos Santos J, Roth T, Marques DR. Epworth sleepiness scale: a meta-analytic study on the internal consistency. Sleep Med. 2023;109:261-9. doi:10.1016/j.sleep.2023.07.008.
-
Chervin RD, Weatherly RA, Garetz SL, et al. Pediatric sleep questionnaire: prediction of sleep apnea and outcomes. Arch Otolaryngol Head Neck Surg. 2007;133(3):216-22. doi:10.1001/archotol.133.3.216.
-
Choi JH, Kim EJ, Choi J, et al. The effect of adenotonsillectomy on changes of position during sleep in pediatric obstructive sleep apnea syndrome. Am J Rhinol Allergy. 2009;23(6):e56-8. doi:10.2500/ajra.2009.23.3363.
-
Paruthi S, Buchanan P, Weng J, et al. Effect of adenotonsillectomy on parent-reported sleepiness in children with obstructive sleep apnea. Sleep. 2016;39(11):2005-12. doi:10.5665/sleep.6232.
-
Cammaroto G, Stringa LM, Iannella G, et al. Manipulation of lateral pharyngeal wall muscles in sleep surgery: a review of the literature. Int J Environ Res Public Health. 2020;17(15):5315. doi:10.3390/ijerph17155315.
-
Binar M, Karakoc O. Anterior palatoplasty for obstructive sleep apnea: a systematic review and meta-analysis. Otolaryngol Head Neck Surg. 2018;158(3):443-9. doi:10.1177/0194599817739857.
-
Güler İ, Kuzucu İ, Baklacı D, Kum RO, Kum NY, Özcan M. Efficiency of expansion sphincter pharyngoplasty in the treatment of obstructive sleep apnea syndrome. Turk Arch Otorhinolaryngol. 2018;56(4):206-9. doi:10.5152/tao.2018.3665.
-
Cahali MB. Lateral pharyngoplasty: a new treatment for obstructive sleep apnea hypopnea syndrome. Laryngoscope. 2003;113(11):1961-8. doi:10.1097/00005537-200311000-00020.
-
Karakoc O, Binar M, Aydin U, Genc H, Akcam T, Gerek M. A tertiary center experience with velopharyngeal surgical techniques for treatment of snoring and obstructive sleep apnea. Auris Nasus Larynx. 2018;45(3):492-8. doi:10.1016/j.anl.2017.06.005.
Declarations
Scientific Responsibility Statement
The authors declare that they are responsible for the article’s scientific content, including study design, data collection, analysis and interpretation, writing, and some of the main line, or all of the preparation and scientific review of the contents, and approval of the final version of the article.
Animal and Human Rights Statement
All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Funding
None.
Conflict of Interest
The authors declare that there is no conflict of interest.
Ethics Declarations
This study was approved by the Ethics Committee of Necmettin Erbakan University (Date: 2022-11-04, No: 4028)
Data Availability
The datasets used and/or analyzed during the current study are not publicly available due to patient privacy reasons but are available from the corresponding author on reasonable request.
Additional Information
Publisher’s Note
Bayrakol MP remains neutral with regard to jurisdictional and institutional claims.
Rights and Permissions
About This Article
How to Cite This Article
Erdem Bayrakcı, Mehmet Akif Eryılmaz, Abitter Yücel, Sema Güleç. A new approach: the effect of modified sutureless lateral pharyngoplasty technique on obstructive sleep apnea syndrome. Ann Clin Anal Med 2026;17(2):158-162
Publication History
- Received:
- December 6, 2025
- Accepted:
- December 30, 2025
- Published Online:
- December 31, 2025
- Printed:
- February 1, 2026

