Effects of vitamin D deficiency on prognosis in intensive care unit patients
Vitamin D deficiency in intensive care unit
Authors
Abstract
Aim Vitamin D deficiency is frequently observed in intensive care unit patients, but its clinical effects on patients are still debated. The aim of this study is to determine the prevalence of vitamin D deficiency in intensive care patients and its effect on patient outcomes and mortality.
Methods 384 patients accepted to the study were divided into two groups as patients with (Group 1) and without (Group 2) Vitamin D deficiency according to their 25(OH)D levels. Demographic data of the patients, APACHE-2 scores, additional diseases, laboratory data, mechanical ventilation needs, follow-up periods in the intensive care unit, and mortality rates were recorded retrospectively from patient records.
Results Vitamin D deficiency was detected in 279 of the patients. The two groups were similar in terms of demographic characteristics of the patients. There was no significant difference between the two groups in terms of APACHE-2 scores, length of stay in the intensive care unit, need for endotracheal intubation, and mortality rates. The incidence of septicemia and infection parameters was significantly higher in the group with vitamin D deficiency (p<0.05). There was no significant difference between the two groups in terms of the incidence of malignancy.
Conclusion Vitamin D deficiency is frequently seen in critically ill patients and increases their susceptibility to infections, but there is no consensus on its effect on mortality. More extensive studies are needed on this subject.
Keywords
Introduction
Vitamin D can be defined as a fat-soluble vitamin, a prohormone in steroid structure, most of which is synthesized in the skin by exposure to sunlight, and a negligible portion can be obtained from dietary sources.1 Vitamin D deficiency (VDD) is widely reported in Turkey as well as all over the world.2 VDD is frequently seen in patients monitored in the intensive care unit (ICU), decreased exposure to sunlight, impaired synthesis, altered metabolism, and preexisting deficiencies.3 The impact of vitamin D on musculoskeletal health and bone mineralisation is well documented; nevertheless, the presence of vitamin D receptors in diverse cell types suggests that it might have broader physiological implications beyond bone metabolism.4 VDD has been associated with diseases affecting bone health, such as osteoporosis and osteomalacia, as well as myocardial remodeling and cardiovascular diseases.5 Autoimmune diseases, and some types of malignancy.6 In addition, research indicates that vitamin D plays a role in immunomodulation with its receptors on various immune cells (neutrophils, lymphocytes, macrophages, dendritic cells) and significantly influences the immune system by regulating cell growth, proliferation, differentiation, apoptosis, and immunoglobulin synthesis.7,8 In critically ill patients requiring ICU admission, VDD has been associated with poor prognosis and increased mortality rates due to disturbances in physiological, immunological, and metabolic functions,9 although some studies provide conflicting results on this association.7 Currently, serum 25-hydroxyvitamin D (25(OH)D) concentration is considered the most reliable biomarker for assessing vitamin D status due to its long half-life of roughly 14-21 days. In the literature, 25(OH)D levels below 20 ng/ml are classified as vitamin D deficiency; values between 21–29 ng/ml as vitamin D insufficiency; and values above 150 ng/ml as intoxication.10 Given the cheapness, availability, relatively broad safety profile, and potential to improve prognosis of vitamin D, some studies advocate routine administration of vitamin D to ICU patients.11 However, there is no consensus on the best methods of monitoring, target serum 25(OH)D levels, and treatment modifications.This study aims to determine the prevalence of VDD in ICU patients and to reveal its effects on disease prognosis, sepsis frequency, and mortality in the ICU.
Materials and Methods
This retrospective study included data from 1032 patients admitted to the general ICU between 01.01.2023 and 01.08.2024, following approval from the ethics committee. In this study, patients who had been admitted to more than one ICU during the study period or whose initial 25(OH)D measurements were unavailable were excluded, resulting in a final sample of 384 patients. Patients were classified into two groups according to serum 25(OH)D levels: Group 1, with VDD (25(OH)D < 20 ng/mL), and Group 2, without VDD (25(OH)D ≥ 20 ng/mL). Retrospective medical records were obtained from clinical data, including demographic information, APACHE-II scores, comorbidities, laboratory findings, mechanical ventilation (MV) requirements, ICU duration of stay, and mortality rates. No artificial intelligence-based technologies were used in the process; this study was done following the ethical guidelines of the Declaration of Helsinki.
Ethical Approval
This study was approved by the Ethics Committee of Ankara Etlik City Hospital Scientific Research and Evaluation Ethics Committee (Date: 2024-04-03, No: 107).
Statistical Analysis
The data were analyzed using the GNU PSPP 2.0.0 software package (GNU Project, Free Software Foundation, Boston, MA). Continuous variables were reported as mean ± standard deviation (SD) or median with interquartile ranges, while categorical variables were expressed as percentages. Comparisons between groups were conducted using the Mann-Whitney U test for continuous variables and the Chi-square test for categorical variables. Correlations between variables were evaluated using Spearman’s rank correlation analysis. A p-value of < 0.05 was considered indicative of statistical significance.
Reporting Guidelines
This retrospective observational study was reported in accordance with the STROBE guidelines.
Results
384 patients, aged between 18 and 98, were included in this study. Of these, 279 patients (72.7%) were categorized as the group with VDD (Group 1) and 105 patients (27.3%) as the group without VDD (Group 2). The two groups were statistically similar in terms of demographic characteristics at baseline (Table 1).Comparison of MV requirements, MV duration, and ICU length of stay between Group 1 and Group 2 demonstrated no statistically significant differences. Similarly, no significant difference was found between the two groups in terms of intensive care unit mortality. (Table 2). The groups with and without VDD were compared in terms of infection parameters (CRP and procalcitonin) and sepsis frequency (Table 3). A significant increase in infection indicators and sepsis incidence was observed in Group 1. No significant difference was observed between the groups in terms of the incidence of pneumonia and septic shock. Comorbidities were present in 88% of the study population. The most prevalent comorbidities were malignancies, hypertension, and diabetes mellitus. Among the 384 patients, 139 had a documented malignancy, with prevalence rates of 37.9% in Group 1 and 31.4% in Group 2 (Table 3). No statistically significant difference was found between the two groups in terms of the incidence of malignancy.
Discussion
The current study was planned to observe the relationship between serum vitamin D levels of 384 intensive care patients and their clinical outcomes during intensive care follow-up.
It was determined that patients in the intensive care unit had a serious VDD, which was linked to higher infection parameters and more cases of sepsis; however, it did not affect how long they stayed in the ICU, whether they needed mechanical ventilation, or their mortality rates.In this study, 279 patients had VDD, which corresponded to 72.7% of the patients. The prevalence of VDD in the intensive care unit has been reported to be in a wide range, ranging from 26% to 82% in the literature.12 It is generally accepted that adequate vitamin D levels should be provided due to its effects on the respiratory system, musculoskeletal system, cardiovascular system, and immune system.6 VDD has been linked to a prolonged MV requirement, prolonged hospitalization, and adverse outcomes such as pneumonia and sepsis.13 Research has indicated that VDD may increase the risk of developing sepsis in critically ill patients and may also increase sepsis-related mortality, citing the positive effects of vitamin D on the immune system.9,14,15 Pham et al. reported that Vitamin D supplementation mitigates the risk and severity of acute respiratory tract infections, particularly in deficient individuals.16 However, a study on COPD patients showed that despite the high incidence of VDD in intensive care due to reasons such as malnutrition and limited mobility, there was no relationship between VDD and sepsis, disease prognosis, and mortality.12 In this study, no significant difference was found in the incidence of pneumonia between the VDD and non-VDD groups, while a significant increase was found in infection parameters and sepsis incidence in the VDD group.Research noted that vitamin D supplementation reduces ICU and in-hospital mortality in critically ill patients.17 and that VDD is strongly associated with mortality.5 A study investigating the outcomes of vitamin D supplementation in patients receiving renal replacement therapy has shown that vitamin D supplementation significantly reduces in-hospital mortality.18 There are also studies suggesting that vitamin D supplementation may improve duration of mechanical ventilation, the length of hospital stay, and some clinical outcomes in critically ill patients, but its effect on ultimate mortality is uncertain.3 A large-scale study involving 19,816 patients showed that vitamin D supplementation reduced the time required for mechanical ventilation and the incidence of sepsis, but did not change 28-day mortality.19 In our study, we did not find any significant difference between the groups with and without vitamin D deficiency in terms of length of stay in the intensive care unit, need for endotracheal intubation, duration of mechanical ventilation, and intensive care unit mortality.Many studies have shown a correlation between VDD and some types of malignancies (colon, prostate, breast, and some hematological malignancies) and increased metastases due to the effects of vitamin D on cell growth, differentiation, and apoptosis, and its effects on the immune system.20,21 Inconsistently, the VIDA study, which included 5108 participants receiving high-dose Vitamin D supplements, concluded that supplementation neither prevented cancer nor reduced cancer-related mortality.22 In this study, no significant association was observed between Vitamin D deficiency and the incidence of solid organ malignancies or hematological malignancies.
Limitations
This study has several limitations. First, due to its retrospective design, causal relationships could not be established, and the findings are limited to associations. Secondly, selection bias might have occurred, as only patients with complete records were analyzed. Lastly, the study was conducted at a single center, which may limit the generalizability of the results to other populations.
Conclusion
VDD is a prevalent condition for critically ill patients and negatively affects the clinical outcomes and infection rates of patients. However, its effects on mortality remain unclear. Moreover, the effectiveness and dosage of vitamin D supplementation may vary depending on the patient’s features. Monitoring the quantity of vitamin D and administering supplementation, when necessary, has the potential to improve outcomes in ICU patients, but studies on this topic have yielded conflicting results. More comprehensive studies with larger populations are needed to assess vitamin D levels in intensive care patients and evaluate their effects on improving outcomes.
Tables
Table 1. Demographical data
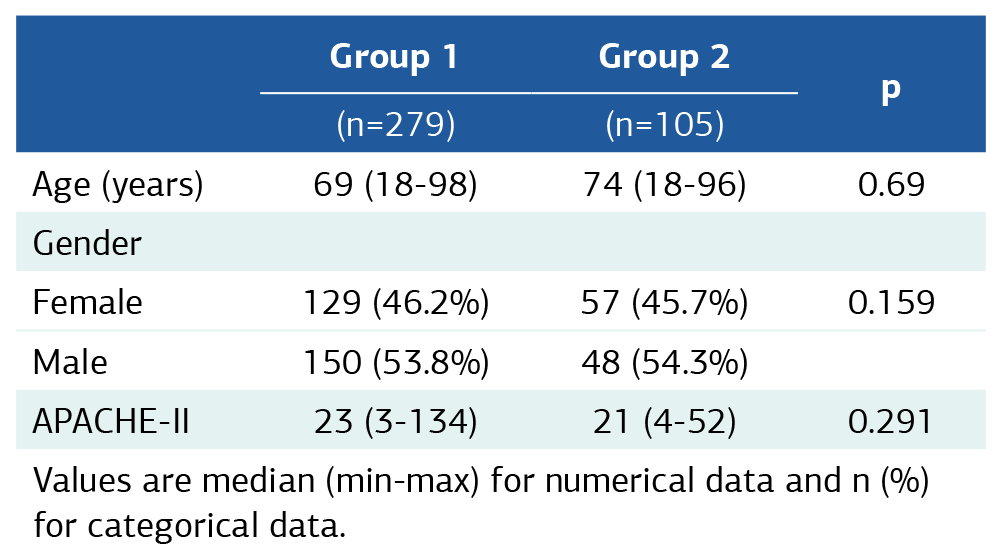
Values are median (min-max) for numerical data and n (%) for categorical data.
Table 2. Prognostic features
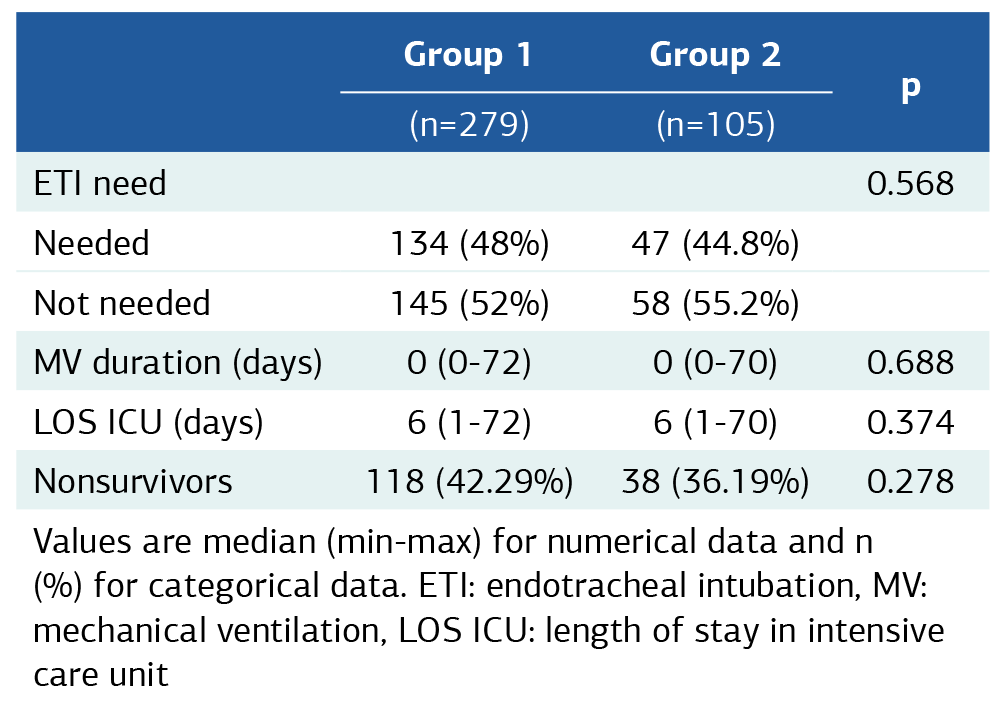
Values are median (min-max) for numerical data and n (%) for categorical data. ETI: endotracheal intubation, MV: mechanical ventilation, LOS ICU: length of stay in intensive care unit
Table 3. Infective properties and malignancy frequency
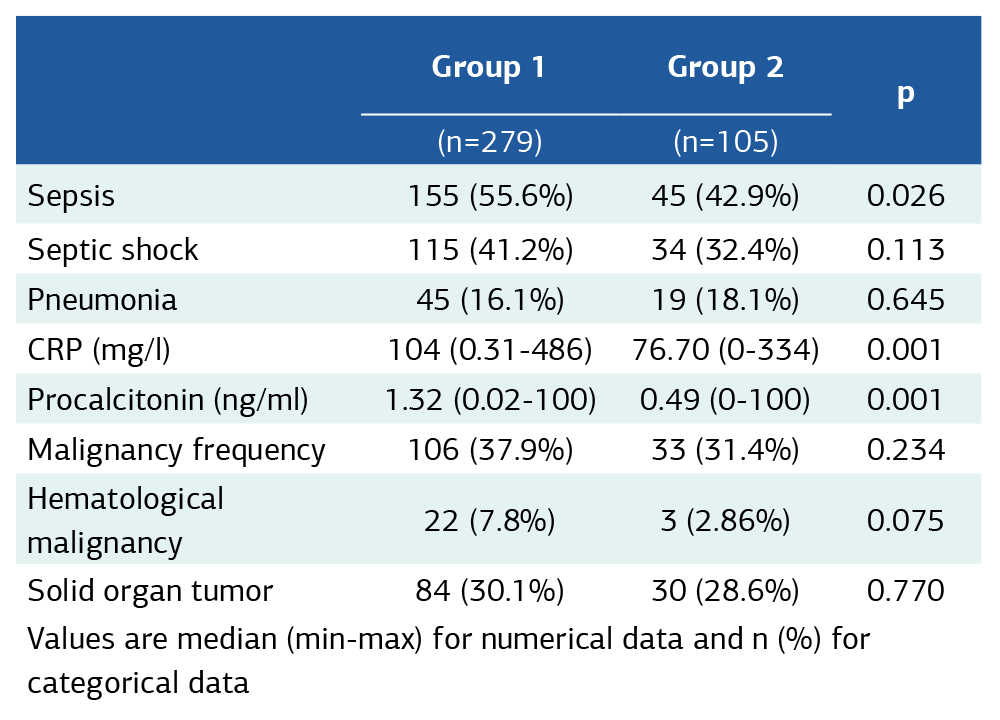
Values are median (min-max) for numerical data and n (%) for categorical data
References
-
Gallagher JC, Rosen CJ. Vitamin D: 100 years of discoveries, yet controversy continues. Lancet Diabetes Endocrinol. 2023;11(5):362-374.
-
Börekçi NÖ. Current information on vitamin D deficiency. Turk J Fam Pract. 2019;10(1):35-42.
-
Wang S, Ren R, Wang K, et al. Evaluation of vitamin D supplementation in critically ill patients: a narrative review of randomized controlled trials published in the last 5 years. Nutrients. 2025;17(5):816. doi:10.3390/nu17050816
-
Giustina A, Lazaretti-Castro M, Martineau AR, et al. A view on vitamin D: a pleiotropic factor? Nat Rev Endocrinol. 2024;20(4):202-208.
-
Hu C, Yang M. Trends of serum 25(OH) vitamin D and association with cardiovascular disease and all-cause mortality: from NHANES survey cycles 2001–2018. Front Nutr. 2024;11:1328136. doi:10.3389/fnut.2024.1328136
-
Jodar E, Campusano C, de Jongh RT, Holick MF. Calcifediol: a review of its pharmacological characteristics and clinical use in correcting vitamin D deficiency. Eur J Nutr. 2023;62(4):1579-1597.
-
Untersmayr E, Kallay E. Insights in immuno-nutrition: vitamin D as a potent immunomodulator. Nutrients. 2020;12(11):3554. doi:10.3390/nu12113554
-
Ismailova A, White JH. Vitamin D, infections and immunity. Rev Endocr Metab Disord. 2022;23(2):265-277.
-
Wasnik S, Kaur R. Correlation of vitamin D deficiency with mortality in critically ill patients admitted to the intensive care unit. Clin Crit Illn. 2024;7(1):1-11.
-
Ghosh A, M S, Sunny AS, Diwakar L, Issac TG. Prevalence and patterns of vitamin D deficiency and its role in cognitive functioning in a cohort from South India. Sci Rep. 2024;14(1):11215.
-
Geiger C, McNally JD, Christopher KB, Amrein K. Vitamin D in the critically ill: update 2024. Curr Opin Clin Nutr Metab Care. 2024;27(6):515-522.
-
Avcı S, Eraslan Doğanay G, Cırık MÖ. Relationship between vitamin D level and sepsis-mortality in intensive care unit. Sakarya Med J. 2022;12(2):250-255.
-
Malinverni S, Ochogavia Q, Lecrenier S, et al. Severe vitamin D deficiency in patients admitted to the emergency department with severe sepsis is associated with an increased 90-day mortality. Emerg Med J. 2023;40(1):36-41.
-
Jiménez-Sousa MÁ, Martínez I, Medrano LM, Fernández-Rodríguez A, Resino S. Vitamin D in human immunodeficiency virus infection: influence on immunity and disease. Front Immunol. 2018;9:458. doi:10.3389/fimmu.2018.00458
-
Li Y, Ding S. Serum 25-Hydroxyvitamin D and the risk of mortality in adult patients with Sepsis: a meta-analysis. BMC Infect Dis. 2020;20(1):189.
-
Pham H, Rahman A, Majidi A, Waterhouse M, Neale RE. Acute respiratory tract infection and 25-hydroxyvitamin D concentration: a systematic review and meta-analysis. Int J Environ Res Public Health. 2019;16(17):3020.
-
Li C, Zhao K, Ren Q, et al. Vitamin D supplementation during intensive care unit stay is associated with improved outcomes in critically ill patients with sepsis: a cohort study. Front Cell Infect Microbiol. 2024;14:1485554.
-
Pi H, Xiong H. Potential benefits of vitamin D intake for improving outcomes in critical care patients receiving renal replacement therapy: a retrospective study based on the MIMIC-IV database. Med Clin Biochem. 2025;22(2):1125.
-
Guan J, Ma S, Liang Z, et al. Potential benefits of vitamin D for sepsis prophylaxis in critically ill patients. Front Nutr. 2023;10:1073894. doi:10.3389/fnut.2023.1073894
-
Carlberg C, Velleuer E. Vitamin D and the risk for cancer: a molecular analysis. Biochem Pharmacol. 2022;196:114735. doi:10.1016/j.bcp.2021.114735
-
Samanta I, Patil DJ, More CB. Assessment of vitamin D levels in patients with oral potentially malignant disorders and oral squamous cell carcinoma: a cross-sectional study. J Oral Biol Craniofac Res. 2024;14(1):27-32.
-
Scragg RKR. Overview of results from the Vitamin D Assessment (ViDA) study. J Endocrinol Invest. 2019;42(12):1391-1399.
Declarations
Scientific Responsibility Statement
The authors declare that they are responsible for the article’s scientific content, including study design, data collection, analysis and interpretation, writing, and some of the main line, or all of the preparation and scientific review of the contents, and approval of the final version of the article.
Animal and Human Rights Statement
All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Funding
None
Conflict of Interest
The authors declare that there is no conflict of interest.
Ethics Declarations
This study was approved by the Ethics Committee of Ankara Etlik City Hospital Scientific Research and Evaluation Ethics Committee (Date: 2024-04-03, No: 107)
Informed Consent
Due to the retrospective design of the study and the use of anonymized patient data, written informed consent was waived by the Ethics Committee.
Data Availability
The data supporting the findings of this article are available from the corresponding author upon reasonable request, due to privacy and ethical restrictions. The corresponding author has committed to share the de-identified data with qualified researchers after confirmation of the necessary ethical or institutional approvals. Requests for data access should be directed to bmp.eqco@gmail.com
Author Contributions
Conceptualization: P.K.B.
Methodology: P.K.B., G.M.K.
Formal Analysis: P.K.B.
Investigation: P.K.B., G.M.K.
Data Curation: P.K.B.
Writing – Original Draft Preparation: P.K.B.
Writing – Review & Editing: G.M.K.
Supervision: G.M.K.
Abbreviations
APACHE-II: Acute Physiology and Chronic Health Evaluation II
CRP: C-Reactive Protein
ICU: Intensive Care Unit
LOS ICU: Length of Stay in Intensive Care Unit
MV: Mechanical Ventilation
VDD: Vitamin D Deficiency
25(OH)D: 25-Hydroxyvitamin D
Additional Information
Publisher’s Note
Bayrakol MP remains neutral with regard to jurisdictional and institutional claims.
Rights and Permissions
About This Article
How to Cite This Article
Pınar Karabak Bilal, Gül Meral Kocabeyoğlu. Effects of vitamin D deficiency on prognosis in intensive care unit patients. Ann Clin Anal Med 2026;17(Suppl 1):S50-53
Publication History
- Received:
- June 12, 2025
- Accepted:
- July 14, 2025
- Published Online:
- July 21, 2025
- Printed:
- February 20, 2026

